A Randomized Controlled Trial of a Smoking Cessation Intervention Among People With a Psychotic Disorder
Abstract
Objective: Despite extremely high rates of smoking among individuals with psychotic disorders and the associated financial and health costs, few studies have investigated the efficacy of smoking cessation interventions among this group. The purpose of this study was to compare an integrated psychological and nicotine replacement therapy intervention for people with a psychotic disorder with routine care alone. Method: The authors recruited 298 regular smokers with a psychotic disorder residing in the community and randomly assigned them to a routine care comparison condition (N=151) or an eight-session, individually administered smoking cessation intervention (N=147), which consisted of nicotine replacement therapy, motivational interviewing, and cognitive behavior therapy. Outcome variables included continuous and point-prevalence abstinence rates, smoking reduction status, and changes in symptoms and functioning. Results: While there were no overall differences between the treatment group and comparison group in abstinence rates, a significantly higher proportion of smokers who completed all treatment sessions stopped smoking at each of the follow-up occasions (point-prevalence rates: 3 months, 30.0% versus 6.0%; 6 months, 18.6% versus 4.0%; and 12 months, 18.6% versus 6.6%). Smokers who completed all treatment sessions were also more likely to have achieved continuous abstinence at 3 months (21.4% versus 4.0%). There was a strong dose-response relationship between treatment session attendance and smoking reduction status, with one-half of those who completed the intervention program achieving a 50% or greater reduction in daily cigarette consumption across the follow-ups, relative to less than one-fifth of the comparison subjects. There was no evidence of any associated deterioration in symptoms or functioning. Conclusions: These findings demonstrate the utility of a nicotine replacement therapy plus motivational interviewing/cognitive behavior therapy smoking cessation intervention among individuals with a psychotic disorder. Further development of more efficacious interventions is required for those who do not respond to existing interventions.
Individuals with a psychotic disorder have consistently been shown to have very high rates of smoking, ranging from 70% to 88% (1 – 3) , compared with approximately 50% for psychiatric disorders other than schizophrenia and 25% for the general population (4) . Consequently, there is cause for concern because of the serious financial and health costs. It has been estimated that smokers with schizophrenia in the United States spend just over one-third of their weekly income on cigarettes (5) . Smokers with psychiatric illnesses are less likely to stop smoking compared with individuals without psychiatric illnesses, probably because of higher levels of nicotine dependence (1) . Smoking-related diseases may contribute to reductions in life expectancy, with the most common cause of death among people with schizophrenia being ischemic heart disease (6) . Smokers with a psychotic disorder may smoke cigarettes in order to alleviate negative symptoms, cognitive dysfunction, or medication side effects (7) in addition to smoking for many of the same reasons as smokers without a psychiatric illness (3) . Paradoxically, smokers with a psychotic disorder have been reported to experience increased psychiatric symptoms, number of hospitalizations, and a need for higher medication doses (8) .
Several small trials have been conducted among smokers with schizophrenia, using combinations of either nicotine replacement therapy (9 , 10) or bupropion with group interventions (11 – 13) . Such interventions have been shown to be useful among smokers without a mental illness (14) . However, available treatment trials for smokers with schizophrenia have been criticized on methodological grounds, including heterogeneous samples, small sample sizes, and lack of defined interventions and comparison groups, with cessation being achieved among very few participants and recommendations that future smoking cessation interventions be evaluated using more rigorous methodology (15) . There is also a need to assess smoking outcomes other than cessation (16) .
The primary purpose of this study was to evaluate the effect of individually administered motivational interviewing and cognitive behavior therapy plus nicotine replacement therapy on smoking cessation or reduction among individuals with a psychotic disorder and, second, to evaluate impact on psychiatric symptoms. It was hypothesized that a greater proportion of participants receiving motivational interviewing/cognitive behavior therapy plus nicotine replacement therapy would report smoking cessation or reduction, relative to a routine care control condition.
Method
Study Design
All participants provided written informed consent and were assessed at pretreatment, 3 months (15 weeks after initial assessment), and 6 and 12 months following initial assessment. Participants who met the inclusion criteria were randomly allocated to one of two groups: 1) treatment condition, which included eight individual 1-hour sessions of motivational interviewing and cognitive behavior therapy plus nicotine replacement therapy, in addition to treatment as usual and provision of booklets for smoking cessation (17) and for supporters (18) or 2) comparison condition, which included treatment as usual and the same booklets and assessment schedules; treatment as usual included access to general practitioners and publicly funded community mental health teams. A letter was sent to each participant’s general practitioner, case manager, or treating psychiatrist to notify them of the involvement of their patient. Follow-up assessments were conducted by a member of the research team blind to group allocation. Participants were reimbursed $20 for their time, travel, and participation on each assessment occasion.
Participants and Procedure
Participants were 298 smokers with a nonacute psychotic disorder who were recruited from Sydney, Australia and the Newcastle region of NSW, Australia. Referrals were received from community health agencies (82.2%), inpatient psychiatric units (8.3%), and the Neuroscience Institute of Schizophrenia and Allied Disorders schizophrenia register (7.0%). Participants recruited through inpatient units were contacted 2 months postdischarge and invited to take part. Inclusion criteria were at least 18 years of age, smoking at least 15 cigarettes per day, and having an ICD-10 diagnosis of a psychotic disorder. Participants were also required to express an interest in quitting smoking. Exclusion criteria were medical conditions that would preclude use of nicotine patches, being acutely psychotic (in which case, participants were reassessed 1 month postscreening), and having an acquired cognitive impairment.
Participants were informed that they would be randomly assigned to one of two conditions at the end of the initial assessment interview, which was achieved simply by asking them to draw a sealed envelope from a set of envelopes in which there was initially an equal distribution of treatment/control allocations at each site. Preferably, treatment sessions were conducted at the research center or at a nearby community clinic. However, if a participant was unable to attend these centers, sessions were conducted in the participant’s home. The pretreatment assessment lasted 1.5 hours to 2 hours, while follow-up assessments lasted approximately 1 hour. This research was approved by relevant regional and university ethics committees in Sydney and Newcastle. Any participant who missed three consecutive treatment sessions was considered a treatment dropout.
Measures
Key demographic, clinical, and outcome measures are reported in this article. The assessment instruments used have been reported in another article (19) and are described only briefly in this study.
Diagnostic measures
Diagnosis was determined using the Diagnostic Interview for Psychosis (20) , a semistructured interview that confirms diagnosis using the Operational Criteria for Psychosis (21) and produces a diagnostic classification in accordance with ICD-10. The diagnostic categories obtained were later collapsed to match the psychosis categories reported in the Low Prevalence Disorders Study (22) . In addition to providing a clinical diagnosis, the Diagnostic Interview for Psychosis gathered information on sociodemographic characteristics, premorbid adjustment, current symptoms and medication, social functioning, and service utilization. Antipsychotic medication was categorized according to “atypical” versus “typical” subtypes.
Smoking outcome measures
The primary smoking outcome measures were continuous abstinence, point-prevalence abstinence, and smoking reduction status. These were all evaluated on an intention-to-treat or program effectiveness basis (23) . Secondary smoking outcome analyses were based on the amount of treatment actually received, on a self-selection basis. Continuous abstinence refers to the proportion of participants who reported not smoking at all from the nominated quit date to the current assessment point (3, 6, or 12 months). Point-prevalence abstinence refers to the proportion of participants who had been abstinent for the 7 days preceding the follow-up assessment (16) . Smoking reduction status was based on an assessment of whether or not participants had reduced their daily consumption of cigarettes by 50% or greater (including abstinence) relative to baseline (16) , which may be a particularly useful index among individuals with a psychotic disorder (11) . Current abstinence from smoking was confirmed using a Micro 11 Smokerlyser, which assesses breath levels of carbon monoxide. A carbon monoxide level of <10 ppm signified that the participant was unlikely to have smoked in the last 8 hours. Nicotine dependence was measured by the Fagerstrom Test for Nicotine Dependence (24) . Motivation to stop smoking was measured using the 11-item Readiness and Motivation to Quit Smoking Questionnaire, which provides an elaborated stages of readiness scale, ranging from 0 (precontemplation level 1: not contemplating quitting or cutting down) to 4 (preparation stage).
Measures of psychopathology and quality of life
Psychiatric symptoms were assessed using the 24-item Brief Psychiatric Rating Scale (26) , the Beck Depression Inventory-II (27) , and the State-Trait Anxiety Inventory (28) . General functioning was measured using the 12-item Short Form Survey (29) , which produces mental component scores and physical health component scores, with lower scores indicating greater disability.
Therapy
The motivational interviewing/cognitive behavior therapy intervention was delivered individually to participants by a trained therapist, who followed a treatment manual written by the authors specifically for this population (30) . Regular supervision with a senior clinical psychologist (A.B.) was provided. Therapists completed a therapist checklist following each treatment session to ensure the treatment protocol was followed and the consistency of treatment maintained. The intervention consisted of six weekly sessions of 1-hour duration followed by two booster sessions at weeks 8 and 10 (eight sessions total). A summary of the sessions is listed below.
Week 1: Conducting motivational interviewing (31) , comprising feedback from the initial assessment, assessing the good and not so good aspects of smoking, identifying concerns regarding smoking, utilizing the SANE smokefree self-help booklets (17 , 18) , setting goals, outlining a treatment plan, and assigning homework. Week 2: Review of the week and homework exercise, assessment of personal triggers and high-risk situations, planning to stop smoking, introduction to coping with urges, devising a craving plan, provision of information about withdrawal symptoms, and a homework assignment. Week 3: Managing withdrawal and cognitive restructuring, reviewing withdrawal symptoms, setting a quit date, discussing the use of nicotine replacement therapy, engaging a support person (if requested), discussing the abstinence/rule violation effect, identifying and challenging unhelpful negative thoughts, and supplying nicotine patches (7 days×21 mg). Week 4: Review of cognitive strategies and skills enhancement, discussion of seemingly irrelevant decisions, development of personal skills and problem solving skills, and supplying nicotine patches (7 days×21 mg). Week 5: Reviewing and consolidating, coping skills training, cigarette refusal skills training, assertiveness and communication skills development, stress management, and supplying nicotine patches (7 days×21 mg). Week 6: Relapse prevention and lifestyle modification, including rationale for relapse prevention, identifying high-risk situations, regulating consequences, and supplying nicotine patches (14 days×21 mg). Week 8: (booster session 1), review of the previous 2 weeks and relapse prevention plan, discussion about tapering nicotine replacement therapy, and supplying nicotine patches (7 days×21 mg +7 days×14 mg). Week 10: (booster session 2), review of the previous 2 weeks and relapse prevention plan and supplying any remaining patches (7 days×14 mg +14 days×7 mg).
Statistical Analysis
Data were analyzed using SPSS for Windows (version 12.0). For the key smoking-related outcome variables, overall intention-to-treat analyses (23) were conducted (treatment group [N=147] versus comparison group [N=151]), together with subgroup analyses based on patterns of treatment session attendance. For these analyses, missing data were classified either as nonabstinent or as failing to achieve the required rate of reduction. Odds ratios and associated confidence intervals (CI) are also reported, with the comparison group as the reference point (odds ratio=1.00). For the continuous outcome variables (e.g., current tobacco use, symptoms), planned comparisons between assessment phases, from repeated-measures analyses of variance (ANOVAs), were used to examine group differences in patterns of change. As a partial control for the number of statistical tests, the threshold for statistical significance was set at p<0.01.
Results
Overall recruitment and attrition profiles are presented in Figure 1 . Of the 473 individuals referred to the study, 113 were ineligible (23.9%), while an additional 62 (13.1%) declined, leaving a recruited sample of 298 regular smokers with an ICD-10 psychotic disorder.
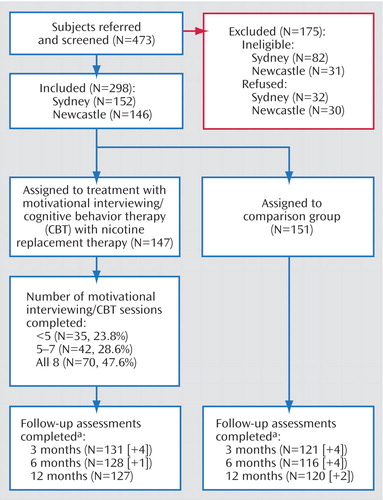
a Bracketed numbers refer to assessments completed outside of the designated time period.
Characteristics of Participants at the Pretreatment Assessment
As detailed elsewhere (19) , there were 156 men and 142 women recruited to the study, with an average age of 37.24 years (SD=11.09 years). The typical participant was Australian born (84.9%), single (65.8%), receiving welfare support (95.6%), and they had not completed senior high school (64.8%). Just over one-half of the study group (56.7%) had a diagnosis of schizophrenia or a schizoaffective disorder. More extensive pretreatment sample characteristics are reported in our earlier article (19) , together with an examination of smoking characteristics and reasons for smoking and quitting.
Attendance at Treatment Sessions and Follow-Up
As shown in Figure 1 , approximately one-half (47.6%) of the treatment group attended all eight treatment sessions, while one-quarter (23.8%) attended less than five sessions. Patterns of follow-up attendance were considered when preparing data sets for analysis. Participants who did not complete their follow-up assessment within the designated time period (i.e., less than one-half of the time interval between follow-ups) were classified as continuous smokers for the intention-to-treat analyses. Only those who completed their follow-up within the designated time period were retained in the nonintention-to-treat analyses. On this basis, eight, five, and two people, respectively, who completed their 3-, 6-, and 12-month follow-up evaluations, had their nonconforming data excluded from the relevant nonintention-to-treat analyses. The resulting patterns of attendance were very similar across all phases (84.6% [N=252] at 3 months; 81.9% [N=244] at 6 months; and 82.9% [N=247] at 12 months). However, since only two-thirds (65.1%) of the participants attended all follow-up sessions, the major nonintention-to-treat analyses involved comparisons between pairs of time points. There were no significant differences between groups in follow-up attendance patterns.
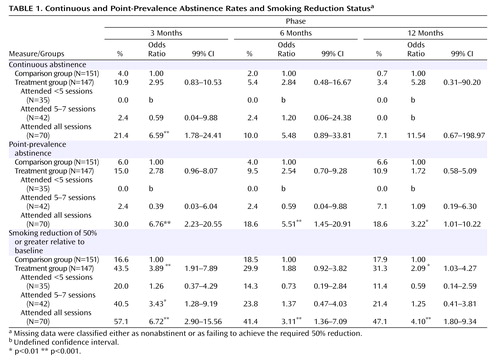
Overall Changes in Smoking
Table 1 displays continuous and point-prevalence abstinence rates and smoking reduction status for the 3-, 6-, and 12-month follow-up assessments. In the intention-to-treat analyses, we found no significant overall differences between the treatment group and comparison group in continuous abstinence or point-prevalence abstinence rates measured at 3-, 6-, and 12-months. However, there was a significant difference in smoking reduction status at 3 months, with 43.5% of the treatment group reducing their cigarette consumption by at least 50% relative to baseline, relative to only 16.6% of the comparison group (odds ratio=3.89, p<0.001). At the subsequent follow-up sessions, approximately 30% of the treatment group and 18% of the comparison group reported comparable reductions, although this difference was only significant at 12 months ( Table 1 ).
Table 1 also reports comparisons between the comparison group and treatment subgroups defined on the basis of their patterns of attendance. There were no baseline differences between these four groups regarding key sociodemographic or clinical variables. Participants who completed all treatment sessions were significantly more likely than the comparison group to have improved at the 3-month follow-up on all three smoking outcome measures (i.e., continuous and point-prevalence abstinence and reduction status). Relative to the comparison group, participants who completed all treatment sessions were also significantly more likely to be abstinent at the 6- and 12-month follow up sessions (point prevalence) and/or to have reduced their consumption by at least 50%. Participants who completed five to seven sessions were also significantly more likely to have decreased their smoking by half at 3 months.
There were no overall differences in abstinence rates or smoking reduction patterns according to medication status upon entry to the study (atypical versus typical antipsychotic medication), nor did medication status impact on the effects observed for treatment session attendance. At each of the follow-up assessments, all but one of the participants who reported that they were abstinent (31 at 3 months, 20 at 6 months, and 24 at 12 months) produced carbon monoxide levels <10 ppm, the exception being one person at 12 months who reported continued high levels of cannabis use. Under the circumstances, this person was classified as abstinent in the analysis, which is in keeping with accepted practice.
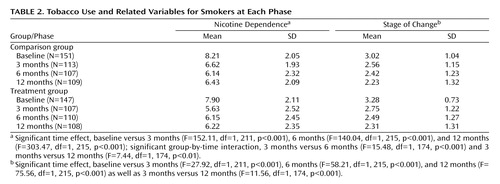
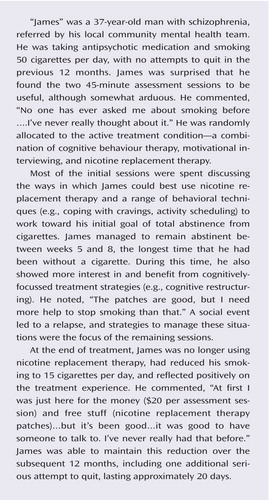
Table 2 and Figure 2 presents profiles for selected smoking-related variables for current smokers at each phase. For nicotine dependence (Fagerstrom Test for Nicotine Dependence scores) and daily cigarette consumption, there were significant reductions from baseline to each of the follow-up sessions. The treatment group also displayed an increase in Fagerstrom Test for Nicotine Dependence scores from 3 months to the subsequent follow-up sessions, relative to smokers in the comparison group, whose nicotine dependence tended to decline. For stage of change, continuing smokers reported a significant decrease in motivation to stop smoking at each of the follow-ups, relative to baseline, as well as a significant decrease from 3 months to 12 months.
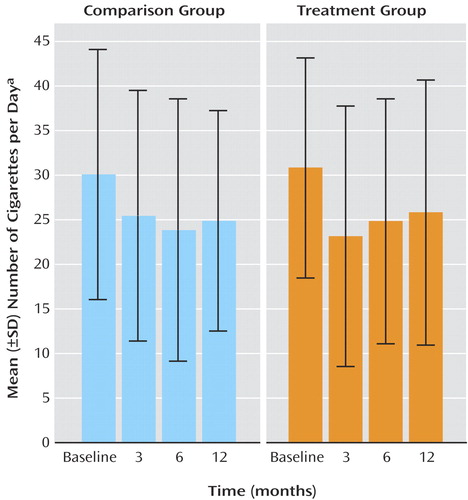
a Significant time effect, baseline versus 3 months (F=43.00, df=1, 211, p<0.001), 6 months (F=59.50, df=1, 215, p<0.001), and 12 months (F=38.85, df=1, 215, p<0.001).
Patterns of Nicotine Replacement Therapy Use
At each follow-up, participants reported on their nicotine replacement therapy use during the preceding period (including patches and other methods). At 3 months, 29.8% of the comparison group and 84.0% of the treatment group reported nicotine replacement therapy use during the preceding 3 months. Among members of the treatment group who attended less than five sessions, 58.6% reported nicotine replacement therapy use, compared with 89.2% and 92.3%, respectively, of those who attended five to seven sessions and all treatment sessions, which largely reflects the link between nicotine replacement therapy provision and treatment attendance. At 6 months, 22.4% of the comparison group and 37.5% of the treated group reported nicotine replacement therapy use during the preceding period. By 12 months, the reported rates had converged, with 28.3% of the comparison group and 31.0% of the treated group reporting nicotine replacement therapy use during the preceding 6 months. Reported use of nicotine replacement therapy at 3 months was associated with a net reduction of 8.14 cigarettes per day, in that nicotine replacement therapy users (N=137) reported a reduction of 12.25 (SD=16.96) cigarettes per day compared with 4.11 (SD=10.6) for nonusers (N=106) (p<0.001). Among the latter group, those who subsequently reported nicotine replacement therapy use at 6 months also showed a net reduction of 8.28 cigarettes per day, with new nicotine replacement therapy users (N=12) reporting a reduction of 10.42 (SD=13.29) compared to 2.14 (SD=9.15) for continued nonusers (N=76) (p<0.01). Among participants who shifted from nonuse of nicotine replacement therapy at 6 months to nicotine replacement therapy use at 12 months (N=20), there was a reduction of 4.10 (SD=14.34) cigarettes per day, compared with an increase of 0.49 (SD=8.46) among participants who were nonusers on both occasions (N=131), a net difference of 4.59 cigarettes per day, which was not significant (p=0.04).
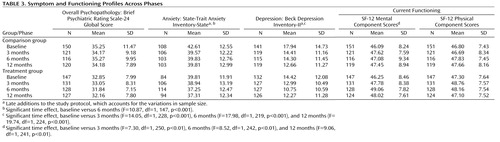
Changes in Symptoms and Functioning
Table 3 presents symptom and functioning profiles across phases. There were no significant differences between groups or across occasions for Brief Psychiatric Rating Scale-24 global scores or Short Form Survey-12 physical component scores. State-Trait Anxiety Inventory state anxiety scores reduced significantly from baseline to 3 months, while Beck Depression Inventory-II depression scores were significantly lower at each of the follow-up sessions relative to baseline. Similarly, baseline SF-12 mental component scores were significantly lower than each of the follow-up occasions, indicative of a general improvement in mental functioning. However, there was no significant group-by-time interaction in the nonintention-to-treat analyses, suggesting that any improvements in symptoms and functioning could not be attributed to specific aspects of the treatment program.
Discussion
The abstinence results are discussed first, followed by consideration of the smoking reduction findings and other potential intervention effects. One of the major findings was that, at all follow-up occasions, a significantly higher proportion of smokers with a psychotic disorder who completed all treatment sessions were currently abstinent, relative to those in the comparison group (point-prevalence rates: 3 months, 30.0% versus 6.0%; 6 months, 18.6% versus 4.0%; and 12 months, 18.6% versus 6.6%). Smokers who completed all treatment sessions were also more likely to have achieved continuous abstinence at 3 months (21.4% versus 4.0%). Moreover, no participants who attended fewer than five treatment sessions reported abstinence at any follow-up point, and very few participants attending five to seven sessions reported that they were abstinent. It appears that if smokers with a psychotic disorder complete all counseling sessions of a smoking cessation intervention (at which nicotine patches are also distributed), then they are more likely to stop smoking than smokers who do not complete those intervention sessions. A similar relationship was also reported in a small, uncontrolled study among smokers with schizophrenia (9) . Therapy procedures to enhance completion of smoking cessation interventions (e.g., intervention completion contracts, other reinforcement contingencies) may enhance cessation rates in future studies.
As in other studies (e.g., 9 , 10 , 12) , the overall cessation rate achieved at the end of treatment was modest and below that reported among smokers without a psychiatric illness (33) . However, the lower cessation rates observed among the current sample are not unexpected, given that people with a chronic mental illness often have higher nicotine dependence (1) , smoke more each day, and are less likely to have made previous attempts to stop smoking (19) . From a methodological perspective, researchers seeking a higher degree of certainty in the assessment of current smoking abstinence may also require lower carbon monoxide thresholds (e.g., <3 ppm) (32) .
Arguably, there was a more marked (treatment) dose-response relationship evident in the smoking reduction findings ( Table 1 ). Approximately one-half (41.4% to 57.1%) of the participants who completed the intervention reduced their smoking by at least 50% relative to baseline, compared with less than one-fifth of the comparison group (16.6% to 18.5%). This also extended to those who completed five to seven sessions (at least at 3 months). Given that reducing smoking does not appear to undermine future cessation efforts and may increase motivation (34) , this is a potentially important finding. In a recent review of published nicotine replacement therapy studies (primarily involving smokers not trying to quit), Hughes and Carpenter (16) reported that 12% to 35% of participants receiving the active treatment reduced their daily cigarette consumption by 50% or greater (including abstainers), compared with 3% to 22% among participants in the control condition. The corresponding 12-month data from this study (31.3% versus 17.9%) are generally consistent with these findings, attesting to the value of targeting reduction, not just abstinence.
The high numbers of cigarettes smoked and levels of nicotine dependence reported in this study (19) highlights the need for earlier smoking interventions among young people with mental health problems before they become heavy smokers. Current practice guidelines for psychiatrists recommend nicotine replacement therapy use even in early cessation attempts among individuals with psychiatric disorders, as they appear to have more withdrawal symptoms when they stop smoking (35) . In our study, nicotine replacement therapy commencement was associated with a net reduction of five to eight cigarettes per day, suggesting that higher doses or a longer duration of nicotine replacement therapy use may be necessary to obtain additional benefits. More generally, we should further explore the delivery and uptake of smoking interventions in primary care settings as well as any potential barriers (36) . There is also an urgent need for further development of more efficacious interventions among smokers with severe mental illnesses who do not respond to interventions such as those evaluated in this study. Pharmacological approaches giving consideration to bupropion (e.g., 13 ) and Rimonabant, a cannabinoid receptor-1 antagonist (37) , or different combinations of nicotine replacement therapy and motivational interviewing/cognitive behavior therapy interventions are worthy of further investigation. Although other studies have reported benefits of atypical versus typical antipsychotic medication on smoking (e.g., 10 ), our study did not find a significant benefit, and future studies should address this issue. It is also worth considering specific interventions for those starting on a regimen of clozapine, since this is known to decrease cravings (38) .
Further study is needed to evaluate long-term nicotine replacement therapy use or extended cognitive behavior therapy interventions, allowing for resumption of treatment following relapse. It has also been suggested that smokers who reduce the number of cigarettes smoked should be informed that they should stop smoking but, if unable to do so in the short-term, that reducing smoking can be helpful in increasing their likelihood of quitting (11) . Hughes (34) and McChargue and colleagues (15) have suggested that reduction-focused smoking interventions among smokers with schizophrenia who do not wish to abstain from cigarettes should be evaluated, which also takes into account medication impacts and changes. The finding that individuals who continue smoking reported a significant decrease in motivation to stop smoking ( Table 2 ) is not at odds with these recommendations by Hughes and McChargue et al. and probably reflects relatively high levels of motivation at the point of recruitment, rather than negative expectations associated with ongoing study participation. There are also important financial and health benefits of smoking reduction among individuals with severe mental illnesses (34) . Another important finding was that there was a significant improvement for the study groups as a whole on several mental health measures and no worsening of psychotic symptoms over time Table 3 ), which is consistent with other studies (e.g., 9 , 10) . Thus, the evidence suggests that participation in a smoking cessation study is not associated with the worsening of symptoms.
Our study is currently the largest randomized controlled trial of a smoking intervention among individuals with a psychotic disorder. Since there was no control for therapy time, the possibility exists that the superior outcomes for the smoking intervention participants were because of additional therapist attention and support rather than the specific motivational interviewing/cognitive behavior therapy and nicotine replacement therapy intervention. However, this seems unlikely given the levels of dependence in this study and the evidence supporting the efficacy of combined nicotine replacement therapy and motivational interviewing/cognitive behavior therapy among nonpsychiatric populations (14 , 16) . Given the ubiquitous nature of smoking among people with a psychotic disorder, the heavy costs of smoking among this group and the modest but encouraging findings, further randomized controlled trials examining more comprehensive interventions are probably required as well as assessments of the long-term outcomes of smoking cessation and reduction interventions.
1. Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA: Prevalence of smoking among psychiatric outpatients. Am J Psychiatry 1986; 143:993–997Google Scholar
2. De Leon J: Smoking and vulnerability for schizophrenia. Schizophr Bull 1996; 22:405–409Google Scholar
3. Reichler H, Baker A, Lewin T, Carr V: Smoking among in-patients with drug-related problems in an Australian psychiatric hospital. Drug Alcohol Rev 2001; 20:231–237Google Scholar
4. Herran A, de Santiago A, Sandoya M, Fernandez MJ, Diez-Manrique JF, Vazquez-Barquero JL: Determinants of smoking behavior in outpatients with schizophrenia. Schizophr Res 2000; 41:373–381Google Scholar
5. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH: Smoking and mental illness: a population based prevalence study. JAMA 2000; 284:2606–2610Google Scholar
6. Lawrence D, Holma D, Jablensky A: Preventable Physical Illness in People with Mental Illness. Perth, University of Western Australia, 2001Google Scholar
7. Dalack GW, Healy DJ, Meador-Woodruff JH: Nicotine dependence in schizophrenia: clinical phenomena and laboratory findings. Am J Psychiatry 1998; 115:1490–1501Google Scholar
8. Williams JM, Ziedonis D: Addressing tobacco among individuals with a mental illness or an addiction. Addict Behav 2004; 29:1067–1083Google Scholar
9. Addington J, el-Guebaly N, Campbell W, Hodgins DC, Addington D: Smoking cessation treatment for patients with schizophrenia. Am J Psychiatry 1998; 155:974–976Google Scholar
10. George TP, Ziedonis DM, Feingold A, Pepper TW, Satterburg CA, Winkel J, Rounsaville BJ, Kosten TR: Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry 2000; 157:1835–1842Google Scholar
11. Evins AE, Corinne C, Rigotti NA, Freudenreich O, Henderson DC, Olm-Shipman CM, Goff DC: Two-year follow-up of a smoking cessation trial in patients with schizophrenia: increased rates of smoking cessation and reduction. J Clin Psychiatry 2004; 63:307–311Google Scholar
12. George TP, Vessicchio JC, Termine A, Bregartner TA, Feingold A, Rounsaville BJ, Kosten TR: A placebo controlled trial of bupropion for smoking cessation in schizophrenia. Biol Psychiatry 2002; 52:53–61Google Scholar
13. Weiner E, Ball MP, Summerfelt A, Gold J, Buchanan RW: Effects of sustained-release bupropion and supportive group therapy on cigarette consumption in patients with schizophrenia. Am J Psychiatry 2001; 158:635–637Google Scholar
14. Silagy C, Lancaster T, Stead L, Mant D, Fowler G: Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2004; CD000146Google Scholar
15. McChargue DE, Gulliver SB, Hitsman B: Would smokers with schizophrenia benefit from a more flexible approach to smoking treatment? Addiction 2002; 97:785–793Google Scholar
16. Hughes JR, Carpenter MJ: The feasibility of smoking reduction: an update. Addiction 2005; 100:1074–1089Google Scholar
17. SANE Australia: The SANE Smokefree Guide for Consumers. Melbourne, SANE Australia, 2000Google Scholar
18. SANE Australia: The SANE Smokefree Guide for Supporters. Melbourne, SANE Australia, 2000Google Scholar
19. Baker A, Richmond R, Haile M, Lewin TJ, Carr VJ, Taylor RL, Constable PM, Jansons S, Wilhelm K, Moeller-Saxone K: Characteristics of smokers with a psychotic disorder and implications for smoking interventions. Psychiatry Res (in press)Google Scholar
20. Castle DJ, Jablensky A, McGrath JJ, Carr V, Morgan V, Waterreus A, Valuri G, Stain H, McGuffin P, Farmer A: The Diagnostic Interview for Psychoses (DIP): development, reliability and applications. Psychol Med 2006; 36:69–80Google Scholar
21. Jablensky A, McGrath J, Herrman H, Castle D, Gureje O, Evans M, Carr V, Morgan V, Korten A, Harvey C: Psychotic disorders in urban areas: an overview of the study on low prevalence disorders. Aust NZ J Psychiatry 2000; 34:221–236Google Scholar
22. McGuffin P, Farmer A, Harvey, I: A polydiagnostic application of operational criteria in studies of psychotic illness: development and reliability of the OPCRIT system. Arch Gen Psychiatry 1991; 48:764–770Google Scholar
23. Wright CC, Sim J: Intention-to-treat approach to data from randomized controlled trials: a sensitivity analysis. J Clin Epidemiol 2003; 56:833–842Google Scholar
24. Fagerstrom KO, Kunze M, Schoberberger R, Breslau N, Hughes JR, Hurt RD, Puska P, Ramstrom L, Zatonski W: Nicotine dependence versus smoking prevalence: comparisons among countries and categories of smokers. Tob Control 1996; 5:52–56Google Scholar
25. Crittenden KS, Manfredi C, Lacey L, Warnecke R, Parsons J: Measuring readiness and motivation to quit smoking among women in public health clinics. Addict Behav 1994; 19:497–507Google Scholar
26. Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green M, Shaner A: Appendix 1: Brief Psychiatric Rating Scale (BPRS) expanded version (4.0) scales, anchor points and administration manual. Int J Methods Psychiatr Res 1993; 3:227–243Google Scholar
27. Beck AT, Steer RA, Garbin MG: Beck Depression Inventory-Second Edition. Orlando, Harcourt Brace Jovanovich and Company, 1988Google Scholar
28. Spielberger CD: Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, Calif, Consulting Psychologists Press, 1983Google Scholar
29. Ware JE, Kosinski M, Keller SD: A 12-item short form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233Google Scholar
30. Baker A, Kay-Lambkin F, Bucci S, Haile M, Richmond R, Carr V: Intervention for Tobacco Dependence Among People with a Mental Illness. Sydney, Australia, National Drug and Alcohol Research Centre, 2004Google Scholar
31. Miller WR, Rollnick S: Motivational Interviewing: Preparing People to Change Addictive Behaviour (2nd ed.). New York, Guilford, 2002Google Scholar
32. US Department of Health and Human Services, Tobacco Use and Dependence Guideline Panel (chaired by MC Fiore): Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, Md, US Department of Health and Human Services, 2000Google Scholar
33. Javors MA, Hatch JP, Lamb RJ: Cut-off levels for breath carbon monoxide as a marker for cigarette smoking. Addiction 2005; 100:159–167Google Scholar
34. Hughes JR: Reduced smoking: an introduction and review of the evidence. Addiction 2000; 95(suppl 1):S3–S7Google Scholar
35. Work Group on Nicotine Dependence: Practice guideline for the treatment of patients with nicotine dependence. Am J Psychiatry 1996, 153(suppl): S1–S33Google Scholar
36. Fiore MC, McCarthy DE, Jackson TC, Zehner ME, Jorenby DE, Mielke M, Smith SS, Guiliani TA, Baker TB: Integrating smoking cessation treatment into primary care: an effectiveness study. Prev Med 2004; 38:412–420Google Scholar
37. Le Foll B, Goldberg SR: Cannabinoid CB1 receptor antagonists as promising new medications for drug dependence. J Pharmacol Exp Ther 2005; 312:875–883Google Scholar
38. Potvin S, Stip E, Roy JY: Clozapine, quetiapine and olanzapine among addicted schizophrenia patients: towards testable hypotheses. Int Clin Psychopharmacol 2003; 18:121–132Google Scholar