Jet Lag: Clinical Features, Validation of a New Syndrome-Specific Scale, and Lack of Response to Melatonin in a Randomized, Double-Blind Trial
Abstract
OBJECTIVE: The goals of this study were to validate a new rating scale for measuring severity of jet lag and to compare the efficacy of contrasting melatonin regimens to alleviate jet lag. METHOD: This was a randomized, double-blind trial of placebo and three alternative regimens of melatonin (5.0 mg at bedtime, 0.5 mg at bedtime, and 0.5 mg taken on a shifting schedule) for jet lag. The subjects were 257 Norwegian physicians who had visited New York for 5 days. Jet lag ratings were made on the day of travel from New York back to Oslo (6 hours eastward) and for the next 6 days in Norway. The main outcome measures were scale and item scores from a new, syndrome-specific instrument, the Columbia Jet Lag Scale, that identifies prominent daytime symptoms of jet lag distress. RESULTS: There was a marked increase in total jet lag score in all four treatment groups on the first day at home, followed by progressive improvement over the next 5 days. However, there were no significant group differences or group-by-time interactions. In addition, there was no group effect for sleep onset, time of awakening, hours slept, or hours napping. Ratings on a summary jet lag item were highly correlated with total jet lag scores (from a low of r=0.54 on the day of travel to a high of r=0.80 on day 3). The internal consistency of the total jet lag score was high on each day of the study. CONCLUSIONS: The use of melatonin for preventing jet lag needs further study.
Jet lag refers to a variety of unpleasant symptoms that afflict most individuals for several days after traveling rapidly through several time zones. Typical symptoms include daytime sleepiness, fatigue, impaired alertness, and trouble initiating and maintaining sleep. The disturbance is thought to arise from the failure of the internal biological clock to adjust quickly to phase shifts in the external environment—in particular, the light-dark cycle—at the flight destination (1, 2). Beyond the circadian rhythm factor, stresses of travel preparation and sleep deprivation associated with the flight can contribute to jet lag. Although jet lag typically lasts only a few days, its symptoms can be quite disruptive, impairing work performance (1, 3, 4) or interfering with vacation activities. The severity of jet lag is related to the number of time zones traveled, with the effects generally worse for eastward travel (5, 6). To our knowledge, the prevalence of jet lag and the relative frequency of various jet lag symptoms have not been systematically studied.
Recently, self-treatment of jet lag with exogenous melatonin has become widespread (and promoted by health experts in the media [7]), on the presumption of its ability to reset the circadian clock (8) and promote sleep onset (9, 10). Virtually all field studies (11–18) have claimed a benefit of melatonin over placebo with varying distances and directions of travel, although some have shown statistically nonsignificant differences, with negligible effect sizes, based on small samples.
In one large sample (melatonin, N=474; placebo, N=112), pooled across many studies, use of melatonin led to a 50% reduction in self-rated jet lag (19). The visual analog ratings of jet lag, however, were global and not symptom-specific. By contrast, in a jet lag simulation study of easterly travel, with a 9-hour time shift, use of melatonin showed only a minor advantage in subjective alertness, which was apparent only on the first postshift day (immediately following sleep deprivation). There were no significant differences in daytime fatigue, tenseness, sleepiness, or psychomotor performance despite accelerated resynchronization of some (but not all) physiological rhythms (20). In another 9-hour simulation study, use of melatonin immediately benefited alertness and performance, even before circadian phase shifts set in (21), which suggests that improvement of jet lag symptoms occurs, in part, independent of rhythm resynchronization.
A problem in comparing studies has been the variety of measures used to index jet lag and the lack of a syndrome-specific scale of jet lag severity. Most studies have been conducted by circadian rhythm researchers with a primary focus on sleep disturbance and rate of rhythm adjustment, often neglecting the many bothersome daytime symptoms of jet lag. Although several studies have obtained self-ratings of daytime symptoms, rarely have the scales clearly distinguished between detection of a symptom and the extent to which that symptom is annoying or interferes with desired activities. If a transient symptom were merely detectable but not impairing or bothersome, the advisability of administration of melatonin could be questioned. Finally, some studies have failed to include baseline measures before travel to control for symptoms that may be unrelated to jet lag, such as fatigue and insomnia due to business or vacation activities and sleeping in a novel environment. Such baseline symptoms may also reflect incomplete recovery from jet lag caused by preceding travel to the city of departure.
The present study had three interrelated goals: 1) to develop and validate a daily rating scale for measuring jet lag severity that could serve as a criterion measure in studies of jet lag; 2) to use this scale to learn more about the clinical features of jet lag—its phenomenology, course, and severity in a large subject sample; and 3) to compare a set of contrasting regimens for melatonin administration, controlling for dose and timing. Our expectation was that subjects receiving at least one of the regimens would experience lower symptom severity than subjects receiving placebo.
METHOD
In developing the rating instrument, as we reviewed the literature, we culled a list of 31 symptoms cited as representing jet lag. This list was reviewed by several colleagues and focus groups of frequent travelers. The items were refined and collapsed into a set of 14 common jet lag symptoms, with rare items deleted. To create a daily self-rating scale, each symptom was listed with a 5-point anchored scale according to how much it bothered the individual (0=not at all, 1=a little bit, 2=moderately, 3=quite a bit, 4=extremely). A daily total jet lag score was computed by summing the scores on these 14 symptoms. Subjects also made a daily rating on a summary jet lag item: “Overall, since you last got ready for nighttime sleep, how much were you bothered by any symptoms of jet lag?” This item used the same anchor points as the individual symptoms. In addition, questions were included about sleep medication, alcohol consumption, amount of time napping, and number of hours slept the previous night.
This first version of the Columbia Jet Lag Scale was used in a pilot study of 97 subjects who traveled eastward or westward through more than six time zones after attending a psychiatric meeting in Melbourne, Australia, in August 1996. The subjects’ mean age was 45 years (SD=9.7), 67% of the group were male, and the mean number of days in Australia before returning home was 10.4 (SD=6.6). Subjects made daily ratings on the final day of their stay and each day after returning home, for 5 days. Five of the 14 symptoms that had the lowest correlations with the total jet lag score were eliminated from the revised jet lag scale: confusion about where you are or what time it is, dozing off or short naps, restless nighttime sleep, initial insomnia, and early morning awakening. Thus, sleep phase disturbance was not considered to cause primary subjective distress. The remaining nine contributing items were fatigue, daytime sleepiness, impaired concentration, decreased alertness, trouble with memory, physical clumsiness, weakness, lethargy, and light-headedness. The revised total jet lag score, with a possible range of 0–36, had high internal consistency for each of the 6 days of the study (Cronbach’s alpha=0.78–0.94).
The final version of the Columbia Jet Lag Scale used in the present study (see appendix 1 for a list of the scale items) included, for each of 7 days beginning on the baseline day of air travel, the following components: the nine symptoms used to calculate the total jet lag score, a summary jet lag item, the amount of daytime napping, the time of sleep onset the previous night, the time of final awakening, and the times study capsules were taken. Since alcohol and sleep medication were rarely used during the Melbourne pilot study (subjects were advised to avoid both), these items were not included in the final scale.
Subjects were recruited from 10 groups of Norwegians (N=572)—over 90% of whom were physicians—who visited New York City for 5 days between October 1996 and March 1997 as part of a pharmaceutical-company-sponsored educational program. During lectures on circadian rhythm disorders, the design of the study was presented, with an invitation to participate if the following requirements were met: subjects had to be taking a flight back to Oslo (six time zones eastward) and planning to stay in Norway for at least 5 days; be ages 21–65 years; and have a usual time of awakening on weekdays between 5:00 a.m. and 9:00 a.m. Potential subjects were asked to exclude themselves if they were hypertensive or currently receiving a β-adrenergic blocker; were regularly receiving medication for depression, anxiety, or other psychiatric problems; had current alcohol or other drug abuse or dependence; had chronic problems with insomnia or frequently used melatonin or sleeping pills; and (for women) were pregnant, lactating, or intending to become pregnant within the month. Three hundred thirty-nine persons gave written informed consent to participate in the study. Of those who agreed to participate, 257 (76%) returned completed forms at the end of the study. The mean age of these subjects was 44 years (SD=7, range=24–62). Seventy-nine percent (N=203) were male.
Subjects were randomly assigned to placebo (N=60) or one of three alternative regimens of melatonin administration beginning on the day of travel and continuing daily for the 5 days after travel. On the sixth day after travel, the subjects made ratings but did not take any study capsules. The first experimental group (N=64) took 5.0 mg of melatonin at bedtime, a common dose in other studies (12–15, 17). The second group (N=70) took 0.5 mg at bedtime. This small dose produces total blood levels similar to those secreted endogenously over the entire night (although there is a distinctly higher initial peak concentration 30 minutes after administration, followed for at least 9 hours by an exponential decline) (22). The third group (N=63) also received 0.5 mg of melatonin, but capsules were taken 1 hour earlier each day beginning in the early evening. The timing of the first dose (on the day of travel) was 11 hours after the subject’s usual wake-up time. This shifting schedule was designed to facilitate circadian phase advance according to the phase-response curve described by Lewy et al. (8). Analysis of melatonin content in the capsules by gas chromatography/mass spectrophotometry verified that each dose was within 5% of the stated concentration and that the placebo capsule was melatonin-free.
To keep subjects blind to group assignment, all subjects took an early evening and a bedtime capsule, only one of which—for the three active treatment groups—contained the melatonin. Subjects were instructed to ask for a sleep mask when attempting to sleep on the airplane and to avoid drinking alcohol. Subjects were also asked to try to reestablish their normal bedtime and usual time of awakening when they got home and not to take any medicine (other than the study capsules) to help them sleep. Subjects made ratings on the Columbia Jet Lag Scale for the 7 days of the study before retiring each night, beginning with the baseline rating on the last day in New York before their return to Oslo and ending 1 day after they took their final capsules.
On each of the first 5 days of the study, approximately 2% of the subjects did not take the study capsules but did make daily ratings (this proportion rose to approximately 10% on the last day, when very few subjects had any symptoms of jet lag). The rating on the summary jet lag item as well as the total jet lag item score was missing for approximately 1%–3% of subjects on each day of the study.
RESULTS
As shown in figure 1, total jet lag score on the last day in New York (day 0) was not at an asymptomatic baseline and, in fact, exceeded scores obtained on days 3 to 6 after travel. Nonetheless, there were marked score increases in all four groups on the first day home, followed by progressive improvement over the next 5 days. A repeated measures multivariate analysis of variance for the 6 days after travel was conducted on the total jet lag score, each of its nine component symptoms, and the rating of the summary jet lag item, with baseline ratings as a covariate. There was a main effect of time on all outcome measures (for total jet lag score, Wilks’s lambda=0.22, p<0.0001). However, there were no significant differences between groups (F=0.61, df=3, 216, p=0.62) and no significant group-by-time interactions (which indicates that the curves had parallel descents) (Wilks’s lambda=1.08, p=0.37). In addition, there was no evidence of effects of group (F=0.64, df=3, 224, p=0.59), group-by-time effects on sleep onset (Wilks’s lambda=0.93, p=0.16), time of awakening (F=0.48, df=3, 229, p=0.70; Wilks’s lambda=0.98, p=0.96), hours slept (F=0.28, df=3, 216, p=0.84; Wilks’s lambda=0.95, p=0.49), or hours napping (F=0.23, df=3, 237, p=0.87; Wilks’s lambda=0.96, p=0.57). A post hoc power analysis indicated that if standardized group differences exceeded 0.40 (moderate effect size), they would be detected with power of 80%.
We searched in vain for a subgroup of subjects for whom one or more of the melatonin regimens was better than placebo. First, we limited the analysis to the subjects whose baseline ratings indicated full recovery from jet lag due to travel to New York 5 days earlier (summary jet lag score=0) (N=126, 49%). Next, we limited the analysis to the subjects who on the first day home reported at least moderate jet lag on the summary ratings (N=159, 62%). Finally, we limited the analysis to the subjects who were asymptomatic at baseline but reported at least minimal jet lag on the second day home, when presumably they had recovered from the sleep deprivation effects of the travel (N=69, 27%). In these and other subgroup analyses—including control for a possible group-by-season interaction—we again found no significant differences between groups.
At baseline, after 4 days in New York, 85% of the subjects reported the absence of or only a little bit of jet lag. On the first day after return to Norway, when jet lag symptoms were most severe, nearly two-thirds, 63%, reported at least moderate jet lag, while about one-third, 37%, reported none at all or only a little bit. (On subsequent days of the study, only 4% reported severity greater than on day 1.) Even after 6 days, 9% of the subjects reported that at least a little bit of jet lag persisted. Across the study, jet lag severity showed no association with age (all correlations were less than 0.08) or sex (for main effect of sex, F=1.21, df=1, 218, p=0.27).
As with the global rating, the frequency of individual jet lag symptoms peaked on the first day after travel. By the second day the frequency was similar to that at baseline, and it gradually subsided to below baseline levels by day 4. The most commonly reported symptoms were fatigue, daytime sleepiness, decreased daytime alertness, and trouble concentrating or thinking clearly.
On each of the 7 study days, ratings on the summary jet lag item were highly correlated with total jet lag score for the same day (from a low of r=0.54 at baseline to a high of r=0.80 on day 3). The internal consistency of the total jet lag score was high on each of the 7 days of the study (alpha=0.89–0.93).
There was no significant difference in the number of subjects who reported possible drug side effects within the active treatment groups or in those groups compared with the placebo group. However, one subject who received 0.5 mg of melatonin reported, within 20 minutes of taking the first dose, difficulty swallowing and breathing, symptoms that subsided after 45 minutes. The subject stopped taking the capsules but agreed, after the study was completed, to take another single dose to see whether the symptoms would recur. Similar symptoms, although somewhat milder, did recur.
DISCUSSION
The strengths of this study include the large size of the study group, with adequate power to detect moderate group differences, and the daily ratings of jet lag symptoms with the use of a new scale that assesses how much the individual finds the most salient symptoms bothersome. The scale yielded a focused description of the daytime symptoms of jet lag, which was lacking in past studies.
A limitation of our study is that we did not examine posttravel symptoms of sleep disturbance—such as difficulty with sleep onset and maintenance and early morning awakening—that might be more closely tied to circadian rhythm disturbance. However, our pilot Melbourne study indicated that these sleep symptoms had low correlations with the overall judgment of how much the individual was bothered by jet lag. Another limitation was that the 4-day sojourn in New York was apparently insufficient for many subjects to fully synchronize their underlying circadian rhythms to New York time, including subjects who had no symptoms at baseline (23).
We did not attempt to measure circadian phase at baseline, and we recognize that the timing of melatonin administration may not have been optimal in some cases, which is also true for most past studies. If effective use of the treatment relies on precise timing relative to the individual’s phase-response curve (19), practical application for the traveling public is not feasible. However, an alternative dosing regimen, currently under investigation by one of us (A.J.L.), may facilitate phase shift by maintaining physiological levels of plasma melatonin (by means of multiple 0.1-mg doses) throughout the afternoon and evening hours, thus ensuring contact with the phase-advance portion of the melatonin phase-response curve (24). Furthermore, slower rates of postflight adaptation (travel over longer distances) may be needed to detect a beneficial phase-shifting effect of melatonin administration.
We had expected—in this, the largest double-blind, controlled trial of the use of melatonin for jet lag reported to date—to find a benefit of melatonin, with differential effects as a function of drug dose, or timing, or both. We are puzzled by the contrast with past studies with positive findings. There is no obvious reason that our ethnically and professionally homogeneous group (Norwegian physicians) should not have responded to melatonin if it were an effective treatment for jet lag. We wondered if our subjects were atypical in that they experienced jet lag symptoms only mildly or had a higher threshold for reporting symptoms as bothersome. However, the distribution of summary jet lag ratings for our subjects at baseline and when jet lag was most severe (the first day at home) was nearly identical to that of the 97 subjects who participated in our pilot study, in which most subjects had traveled eastward or westward more than six time zones to Melbourne, remained there longer than the Norwegians did in New York, and constituted a more diverse study group. We doubt that individuals who declined to participate in our study differed markedly from the study subjects in terms of susceptibility to jet lag. For all of these reasons, we believe that the overall prevalence levels of jet lag and the frequency of individual jet lag symptoms experienced by our study group may generalize to other populations at risk for jet lag.
Our subjects knew that they had three out of four chances of receiving melatonin. Could this have resulted in a large placebo effect, which could have swamped differences between the groups? If this happened, then the actual drug effect could not have been very large.
It is possible that subjects in other studies have detected the presence of the drug and responded positively according to expectations. (In one study that found only a minimal effect [14], subjects were unable to detect the active agent.) Our twice-daily administration of study capsules (at least one of which was a placebo) may have made it difficult for subjects to guess whether they were receiving melatonin.
Despite our finding of no group differences, the validity of our measures (summary jet lag item and total jet lag score) is supported by their ability to demonstrate gradual improvement in the severity of jet lag over time. Past studies have usually relied on a small number of scales to index severity, without reference to the broad symptoms of jet lag as a syndrome. By contrast, the Columbia Jet Lag Scale contains the full phenomenology of the symptoms most highly correlated with the distress associated with jet lag.
It remains unclear to what extent jet lag symptoms reflect the factors of circadian rhythm desynchrony, stresses of preparation for travel, travel itself (including sleep loss), and the pattern of activities at destinations away from home. If melatonin acts specifically to accelerate adjustment of circadian rhythm, its benefit might be difficult to measure against the background of such concurrent stresses. If melatonin taken before bedtime acts primarily to promote sleep onset (an effect also achievable with short-acting benzodiazepine hypnotics), its benefit might not be strongly reflected in bothersome daytime symptoms.
When all studies of melatonin for jet lag are considered, taking into account variations in assessment instruments, dosing regimens, distances and directions of travel, subject demographics, and sample sizes, the demonstration of clinical benefit is equivocal. Therefore, the use of melatonin for preventing jet lag needs further study.
Received Oct. 30, 1998; revision received Feb. 25, 1999; accepted March 17, 1999. From the New York State Psychiatric Institute; the Department of Psychiatry, Columbia University, New York; Rikshospitalet, Oslo; and Oregon Health Sciences University, Portland. Dr. Spitzer’s address is Biometrics Research, Unit 60, New York State Psychiatric Institute, 1051 Riverside Dr., New York, NY, 10032; [email protected] (e-mail). Supported in part by funds from the New York State Office of Mental Health. Melatonin and placebo capsules were supplied by Allergy Research Group, Inc.
 |
APPENDIX 1. Items on the columbia Jet Lag Scale, to be Answered Each Day of the Study
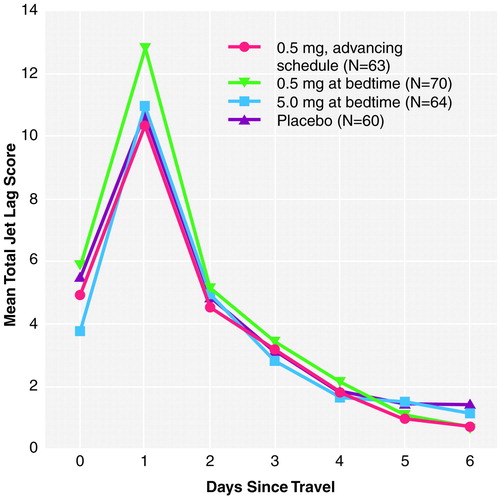
FIGURE 1. Jet Lag Ratings for the Baseline Day of Travel (Day 0), 5 Posttravel Treatment Days (Days 1–5), and the Final Day of Assessment (Day 6)a
Three groups received melatonin, which varied by dose and time of administration; one group received placebo.
1. Winget CM, DeRoshia CW, Markley CL, Holley DC: A review of human physiological and performance changes associated with desynchronosis of biological rhythms. Aviat Space Environ Med 1984; 55:1085–1096Google Scholar
2. Comperatore CA, Krueger GP: Circadian rhythm desynchronosis, jet lag, shift lag, and coping strategies. Occup Med 1990; 5:323–341Medline, Google Scholar
3. Klein KE, Wegmann HM, Athanassenas G, Hohlweck H, Kuklinski P: Air operations and circadian performance rhythms. Aviat Space Environ Med 1976; 17:221–230Google Scholar
4. Graeber RC: Alterations in performance following rapid transmeridian flight, in Rhythmic Aspects of Behavior. Edited by Brown FM, Graeber RC. Hillsdale, NJ, Lawrence Erlbaum Associates, 1982, pp 173–212Google Scholar
5. Aschoff J, Hoffmann K, Pohl H, Wever R: Re-entrainment of circadian rhythms after phase-shifts of the Zeitgeber. Chronobiologia 1975; 2:23–78Medline, Google Scholar
6. Klein KE, Wegmann HM: Significance of circadian rhythms in aerospace operations, in NATO: AGARDograph 247. Edited by the Advisory Group for Aerospace Research and Development. London, NATO Technical Editing and Reproduction, 1980, pp 1–60Google Scholar
7. Brody JE: Debate aside, melatonin can reset the body’s clock. New York Times, Sept 27, 1995, p C9Google Scholar
8. Lewy AJ, Ahmed S, Jackson JM, Sack RL: Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992; 9:380–392Crossref, Medline, Google Scholar
9. Wirz-Justice A, Armstrong SM: Melatonin: nature’s soporific? J Sleep Res 1996; 5:137–141Google Scholar
10. Zhdanova IV, Wurtman RJ: Efficacy of melatonin as a sleep-promoting agent. J Biol Rhythms 1997; 12:644–650Crossref, Medline, Google Scholar
11. Arendt J, Aldhous ME, Marks V: Alleviation of jet lag by melatonin: preliminary results of controlled double blind trial. BMJ 1986; 292:1170Crossref, Medline, Google Scholar
12. Arendt J, Aldhous ME, English J, Marks V, Ardent JH: Some effects of jet lag and their alleviation by melatonin. Ergonomics 1987; 30:1379–1393Google Scholar
13. Skene DJ, Aldhous ME, Ardent J: Melatonin, jet-lag and sleep-wake cycle, in Sleep ’88. Edited by Horn J. New York, Gustav Fisher Verlag, 1989, pp 39–41Google Scholar
14. Petrie K, Conaglen JV, Thompson L, Chamberlain K: Effect of melatonin on jet lag after long haul flights. BMJ 1989; 298:705–707Crossref, Medline, Google Scholar
15. Nickelsen T, Lang A, Bergau L: The effect of 6-, 9- and 11-hour time shifts on circadian rhythms: adaptation of sleep parameters and hormonal patterns following the intake of melatonin or placebo. Advances in Pineal Res 1991; 5:303–309Google Scholar
16. Claustrat B, Brun J, David M, Sassolas G, Chazot G: Melatonin and jet lag: confirmatory results using a simplified protocol. Biol Psychiatry 1992; 32:705–711Crossref, Medline, Google Scholar
17. Petrie K, Dawson AG, Thompson L, Brook R: A double-blind trial of melatonin as a treatment for jet lag in international cabin crew. Biol Psychiatry 1993; 33:526–530Crossref, Medline, Google Scholar
18. Suhner A, Schlagenhauf P, Johnson R, Tschopp A, Steffen R: Comparative study to determine the optional melatonin dosage form for the alleviation of jet lag. Chronobiol Int 1998; 15:655–666Crossref, Medline, Google Scholar
19. Arendt J, Skene DJ, Middleton B, Lockley SW, Deacon S: Efficacy of melatonin treatment in jet lag, shift work and blindness. J Biol Rhythms 1997; 12:604–617Crossref, Medline, Google Scholar
20. Samel A, Wegmann HM, Vejvoda M, Maass H, Gundel A, Schutz M: Influence of melatonin treatment on human circadian rhythmicity before and after a simulated 9-hr time shift. J Biol Rhythms 1991; 6:235–248Crossref, Medline, Google Scholar
21. Deacon S, Arendt J: Adapting to phase shifts, II: effects of melatonin and conflicting light treatment. Physiol Behav 1996; 59:675–682Crossref, Medline, Google Scholar
22. Lewy AJ, Bauer AK, Ahmed S, Thomas KJ, Cutler NL, Singer NM, Moffit MT, Sack RL: The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 1998; 15:71–83Crossref, Medline, Google Scholar
23. Boulos Z, Campbell SS, Lewy AJ, Terman M, Dikj D-J, Eastman CI: Light treatment for sleep disorders: consensus report, VII: jet lag. J Biol Rhythms 1995; 10:167–176Crossref, Medline, Google Scholar
24. Lewy AJ, Bauer VK, Cutler NL, Sack RL: Melatonin treatment of winter depression: a pilot study. Psychiatry Res 1998; 77:57–61Crossref, Medline, Google Scholar



