Clozapine-Associated Elevation in Serum Triglycerides
Abstract
OBJECTIVE: This study was conducted to determine serum lipid level changes in patients who received clozapine or haloperidol. METHOD: Medical records of 222 inpatients treated with clozapine or haloperidol were reviewed. Age, weight, gender, daily antipsychotic dose, total cholesterol level, serum triglyceride level, and concurrent medications were recorded. RESULTS: Clozapine-treated men had significantly higher follow-up serum triglyceride concentrations over baseline than did haloperidol-treated men. Female patients experienced serum triglyceride level elevations regardless of antipsychotic treatment. Changes in total cholesterol levels were not significantly different between treatment groups. CONCLUSIONS: An increase in serum triglyceride levels occurred in clozapine-treated patients; screening for serum triglyceride elevations may be warranted before treatment with clozapine.
Clozapine is an atypical antipsychotic distinguished from other antipsychotics by its efficacy in some treatment-resistant patients and its low incidence of extrapyramidal side effects (1). The use of clozapine has been limited, however, by a risk of agranulocytosis (2) and other adverse effects including weight gain (3, 4) and serum lipid abnormalities (5–7). We performed a retrospective study to examine serum lipid level changes in clozapine- and haloperidol-treated patients.
METHOD
A total of 306 inpatients treated with clozapine or haloperidol at one of five Massachusetts state psychiatric hospitals were considered for inclusion. Medical records were reviewed for age, gender, current clozapine/haloperidol dose, baseline and most recent total cholesterol and triglyceride concentrations, anti-hyperlipidemic treatment, and concurrent medications known to elevate serum lipid concentrations (e.g., β-blockers, glucocorticoids, thiazide diuretics, oral contraceptives, carbamazepine, and valproate). Patients receiving haloperidol decanoate were not included because we desired to analyze oral antipsychotic dose effects exclusively.
Statistical significance was assessed by using two mixed model repeated measures analyses of variance (ANOVAs). The principal analysis was a two-by-two-by-two analysis with drug and gender as the between-group factors and change in triglyceride and total cholesterol levels over time as the dependent variables. Another similar ANOVA was performed with a lipid variable accounting for all but the triglyceride fraction. This permitted us to analyze cholesterol level changes without the influence of triglycerides. This lipid variable is calculated by subtracting one-fifth of the triglyceride level from total cholesterol level (8). Significant ANOVAs were followed up with tests of simple or main effects as appropriate. Contrasts of cell differences were not necessary because the design did not include a factor with more than two levels.
RESULTS
A total of 222 patient records contained sufficient data for study; 177 (129 men [73%] and 48 women [27%]) were receiving clozapine, and 45 (35 men [78%] and 10 women [22%]) were receiving haloperidol. There was a statistically significant difference in mean age (t=–2.80, df=220, p=0.006): the clozapine group had a mean age of 41.4 years (SD=9.8), and the haloperidol group had a mean age of 47.0 years (SD=18.0). There was no relationship between patient age and either total cholesterol or triglyceride level changes. Dose did not correlate with total cholesterol or triglyceride level changes in the clozapine group or with triglyceride level changes in the haloperidol group. A modest correlation between haloperidol dose and change in total cholesterol level was caused by one outlying value.
Three-way repeated measures ANOVAs were performed to analyze the interaction of gender with each drug and with the changes in total cholesterol level, cholesterol level less the triglyceride fraction (8), and triglyceride level at baseline and follow-up. The three-way ANOVA of triglyceride results demonstrated a significant interaction between drug and gender over time (F=5.11, df=1, 194, p<0.05). No other tested term was significant for the overall ANOVA. Tests of simple effects revealed that triglyceride concentrations changed differently (F=18.11, df=1, 194, p<0.01) for clozapine-treated than for haloperidol-treated patients. Tests of simple-simple effects showed that clozapine-treated men had significantly elevated triglyceride concentrations over baseline (F=38.32, df=1, 194, p<0.01), whereas there were no significant differences in triglyceride concentrations for haloperidol-treated patients (F=1.49, df=1, 194). An apparent trend for haloperidol-treated patients to have decreased triglyceride concentrations over time may have failed to reach significance because of low power from the smaller haloperidol group (N=30); the clozapine group had 116 subjects. Women showed a significant increase in triglyceride concentrations (F=6.12, df=1, 194, p<0.05), regardless of antipsychotic treatment.
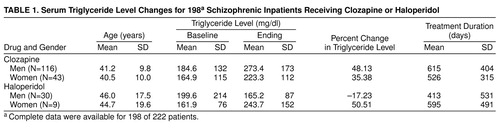
Changes in mean triglyceride concentrations observed in each group are summarized in Table 1. Triglyceride concentrations increased in clozapine-treated men (mean=88.8 mg/dl, SD=165.3; F=38.32, df=1, 194, p<0.01) and decreased in haloperidol-treated men (mean=–34.4 mg/dl, SD=171.0; n.s.). Triglyceride concentrations increased in clozapine-treated women (mean=58.4 mg/dl, SD=113.4) and in haloperidol-treated women (mean=81.8 mg/dl, SD=114.3).
The three-way repeated measures ANOVA, using total cholesterol level as the dependent variable, failed to demonstrate a significant interaction between gender, drug, and total cholesterol level changes (F=0.004, df=1, 214, p=0.95). The two-way interaction of gender and total cholesterol level change over time was also not significant (F=0.16, df=1, 214, p=0.69). Interactions between drug and total cholesterol level changes approached, but did not reach, significance (F=2.65, df=1, 214, p=0.11). This trend appears to be the result of the serum triglyceride component of total cholesterol level. A three-way ANOVA, using total serum cholesterol level less the triglyceride level component, showed no significant effects. Four-way ANOVAs of drug, gender, presence/absence of concurrent medications known to alter serum lipids, and changes in triglyceride or total cholesterol concentrations failed to demonstrate any significant effects of concurrent medications.
DISCUSSION
Our findings suggest that clozapine may be associated with serum triglyceride level elevations. The observed influence of gender on triglyceride concentration appears to be caused by greater triglyceride level changes in the clozapine-treated men than in the haloperidol-treated men. Women in both groups experienced increases in serum triglyceride levels over baseline.
While these are important findings with potential clinical significance, the results must be viewed with caution because of inherent limitations. First, we reviewed medical records in a retrospective manner. Second, only total cholesterol concentrations were obtained. Thus, we were unable to analyze for potential changes in cholesterol subfractions. Third, serum lipid concentrations were obtained before each antipsychotic medication was started and once afterward. Multiple fasting concentrations are desirable to make valid assessments about lipid changes. Last, body weight measurements were not consistently available for us to ascertain whether serum triglyceride level elevations were related to possible weight gain.
Our study results corroborate previously published findings and suggest that it may be important to monitor serum triglyceride concentrations in clozapine-treated patients.
Received Feb. 21, 1996; revisions received Nov. 6, 1996, Sept. 30, 1997, and Sept. 8 and Dec. 21, 1998; accepted Jan. 20, 1999. From the Department of Psychiatry, Worcester State Hospital; Westborough State Hospital; Medfield State Hospital; Taunton State Hospital; and Tewksbury State Hospital. Address reprint requests to Mr. Gaulin, Department of Psychiatry, Worcester State Hospital and University of Massachusetts Medical School, 305 Belmont St., Worcester, MA 01604; [email protected] (e-mail). The authors thank Donna Bartlett, R.Ph., for data collection assistance.
 |
1. Kane J, Honigfeld G, Singer J, Meltzer H: Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988; 45:789–796Crossref, Medline, Google Scholar
2. Alvir JMJ, Lieberman JA: Agranulocytosis: incidence and risk factors. J Clin Psychiatry 1994; 55:137–138Google Scholar
3. Lieberman JA, Safferman AZ: Clinical profile of clozapine: adverse reactions and agranulocytosis. Psychiatr Q 1992; 63:51–70Crossref, Medline, Google Scholar
4. Umbricht DSG, Pollack S, Kane JM: Clozapine and weight gain. J Clin Psychiatry 1994; 55:157–160Medline, Google Scholar
5. Ghaeli P, Dufresne RL: Elevated serum triglycerides on clozapine resolve with risperidone (abstract). Pharmacotherapy 1995; 15:382Google Scholar
6. Ghaeli P, Dufresne RL: Serum triglyceride levels in patients treated with clozapine. Am J Health Syst Pharm 1996; 53:2079–2081Google Scholar
7. Spivak B, Roitman S, Vered Y, Mester R, Graff E, Talmon Y, Guy N, Gonen N, Weizman A: Diminished suicidal and aggressive behavior, high plasma norepinephrine levels, and serum triglyceride levels in chronic neuroleptic-resistant schizophrenic patients maintained on clozapine. Clin Neuropharmacol 1998; 21:245–250Medline, Google Scholar
8. Goldberg AC: Lipid disorders, in Manual of Medical Therapeutics, 27th ed. Edited by Woodley M, Whelan A. Boston, Little, Brown, 1993, pp 419–424Google Scholar



