Psychological and Behavioral Functioning in Adolescent Psychiatric Inpatients Who Report Histories of Childhood Abuse
Abstract
OBJECTIVE: The purpose of this study was to examine psychological and behavioral functioning in psychiatrically hospitalized adolescents who report histories of childhood abuse. METHOD: Three hundred twenty-two subjects completed an assessment battery of psychometrically well-established instruments. Childhood abuse was assessed by using the childhood abuse scale of the Millon Adolescent Clinical Inventory. Childhood abuse scores of 30 or less and 70 or greater were used to create two study groups—no abuse (N=93) and high abuse (N=70), respectively. The two study groups were compared demographically and on the battery of instruments. RESULTS: The two groups differed substantially on most measures of psychological disturbance examined by the assessment battery. When age and depression level were controlled, the high-abuse group was characterized by significantly higher levels of dependency, suicidality, violence, impulsivity, substance use problems, and borderline tendency. Correlational analyses with the entire study group (N=322) revealed that higher levels of these psychological problems were positively associated with higher levels of childhood abuse. CONCLUSIONS: Psychiatrically hospitalized adolescents who report childhood abuse present with a constellation of symptoms that, after removing the effects of depression, are consistent with borderline personality in statu nascendi.
Childhood abuse, defined as sexual, physical, and/or emotional maltreatment, increasingly has become the focus of clinical and research attention during the past three decades. The past decade, in particular, has witnessed the growth of abuse-related research targeting children and adolescents (1, 2). Although many unanswered questions remain about childhood abuse, the emerging picture is that childhood abuse is common, is associated with many negative consequences, and represents a major public health problem (1).
Childhood abuse appears quite prevalent both in the United States and internationally (3–5). Childhood abuse is associated with increased risk for a plethora of short-term (6), intermediate-term (7), and long-term (8) sequelae. Studies have found that childhood abuse increases the risk for a variety of psychological and behavioral problems (e.g., depression, substance abuse, aggression, delinquency), cognitive and neurophysiological deficits (9), and psychiatric disorders (10–12).
The nature of the connection between childhood abuse and psychological problems remains ambiguous. The diversity of problems reported to be associated with trauma suggests that it is ubiquitous to psychological and psychiatric disorders. A review of 45 studies concluded that abused children were consistently more symptomatic than nonabused children for nearly all symptoms and behaviors examined (2). Childhood abuse was estimated to account for 15% to 45% of the variance in symptomatic behaviors, although no one symptom picture characterized the majority of abused children. Furthermore, many childhood abuse victims do not later demonstrate many or any of these sequelae (10, 13–15).
Studies comparing abused children to clinical nonabused children have also produced conflicting data (2). Except for sexual behaviors, the abused children were generally less symptomatic than their nonabused clinical comparisons. Kendall-Tackett and colleagues (2) noted two potential methodological confounds that might account, in part, for these surprising findings. First is the issue of whether abuse was identified in the clinical comparison samples. Second, they noted that the clinical comparison groups—by definition—were composed of patients referred for their symptomatic and behavioral difficulties. A third possibility is that axis II symptoms were not a part of these comparisons and that the abused children may have registered more psychopathology in this realm as opposed to axis I functioning.
These issues highlight the importance of minimizing selection, sampling, and assessment confounds (16, 17) that can influence reports of childhood abuse and its psychological correlates. These and other complex issues pertaining to validity of recall (18) notwithstanding, examination of psychological functioning in study groups of clinical patients can better inform clinical research and intervention efforts. One strategy is to compare study groups from the same overall study population by using similar recruitment procedures and measures (17). This approach lessens the degree to which any identified distinguishing characteristics are artifacts of the selection and recruitment methodology (19).
In this study, we examine psychological and behavioral correlates of childhood abuse in psychiatrically hospitalized adolescents. We compare adolescents who reported high childhood abuse to those who reported no childhood abuse by using a battery of psychometrically well-established self-report instruments. In addition to this categorical approach, contrasting two groups created to maximize differences in the self-report of childhood abuse, we aim to examine the dimensional association between reports of childhood abuse and psychological variables. Categorical analyses are selected to provide clarification of the equivocal findings in the literature. The dimensional analyses more accurately reflect the range and severity of abusive childhood experiences (i.e., greater ecological validity) and allow examination of the degree to which these experiences affect psychological functioning.
METHOD
Subjects
Subjects were a nearly consecutive series of 322 adolescent inpatients admitted to the evaluation and crisis intervention unit of a private, nonprofit psychiatric teaching hospital. These patients were hospitalized for a variety of serious psychiatric problems. Patients were admitted on the basis of need for inpatient-level intervention; no other selection processes were used.
Inclusion criteria for the study population included 1) an adequate ability to read and comprehend the psychological evaluations used (see Procedure), 2) not actively psychotic, and 3) not so cognitively impaired or agitated as to preclude testing. At admission, all subjects and their parents (or legal guardians) provided written informed consent for evaluation.
Of the 322 subjects, 137 (42.5%) were male, and 185 (57.5%) were female. Ages ranged between 13 and 19 years (mean=15.8, SD=1.5). Two hundred sixty-one (81.1%) of the subjects were Caucasian, 33 (10.2%) were African American, 26 (8.1%) were Hispanic American, and two (0.6%) were of other ethnicity. Subjects were predominately from lower- to middle-class families with 75 (23.3%) of the 322 subjects receiving public entitlements. Global Assessment of Functioning Scale ratings averaged 53.9 (SD=11.2) at the time of admission and averaged 62.5 (SD=10.3) for the year before admission.
DSM-III-R diagnoses were assigned at the time of discharge (independently of the testing described here). The most frequently assigned diagnoses were, in descending order, major depression (41%, N=133), dysthymia (39%, N=124), drug use disorders (38%, N=123), conduct disorder (24%, N=76), alcohol use disorders (22%, N=71), oppositional defiant disorder (21%, N=68), and attention deficit hyperactivity disorder (15%, N=47). These clinical consensus diagnoses were generated on the basis of a review of each patient’s history and presenting data by a multidisciplinary treatment team of experienced clinicians with faculty supervision (D.C.F.); semistructured diagnostic interviews were not employed. Medical record data and family reports/corroborations represented routine components of the diagnostic evaluations. The clinical-consensus psychiatric diagnoses are provided solely for descriptive and contextual information.
Procedure
Subjects completed a battery of self-report instruments within 1 and 4 days of admission. All of the measures were administered and scored by computer. A brief description of the measures follows.
The Millon Adolescent Clinical Inventory (20) is a 160-item, self-report inventory developed and normed with clinical samples (20, 21) and used with adolescent inpatients(21, 22). The Millon Adolescent Clinical Inventory is characterized by good psychometric properties and good theoretical-substantive, internal-structural, and external-criterion validation (20, 21). The Millon Adolescent Clinical Inventory has been validated against several measures of psychological functioning (20). Millon and colleagues (20) reported adequate test-retest reliability (correlation coefficients ranged from 0.57 to 0.92 for individual scales) and adequate internal consistency (alpha coefficients ranged from 0.73 to 0.91 for individual scales).
The Millon Adolescent Clinical Inventory contains basic validity checks (e.g., completeness, certain validity items—chosen because of their extremely low rates—that if endorsed might suggest insufficient attention to the test or carelessness). All subjects considered in this report passed the validity checks. The Millon Adolescent Clinical Inventory scoring process takes into account age, gender, and actuarial base rate data to establish scale scores. Millon Adolescent Clinical Inventory scale score cutoffs are produced so that the frequencies of the scale scores correspond to actual trait frequencies in adolescent clinical populations (see 20, 21). The Millon Adolescent Clinical Inventory also weights and adjusts scores based on test-taking attitudes (i.e., levels of disclosure, desirability, and debasement).
Two specific scales of the Millon Adolescent Clinical Inventory were used for this study: the childhood abuse scale and the borderline tendency scale.
The child abuse scale contains 24 items that assess various forms of abuse (e.g., “People did things to me sexually when I was too young to understand”). High scores on this scale reflect adolescent self-reports of shame or disgust about having experienced sexual, physical, or verbal abuse from others. The childhood abuse scale showed adequate internal consistency in two validation samples (0.83 and 0.81) and a test-retest (3–7 days) correlation of 0.81 (20). Scores on the childhood abuse scale were significantly correlated with clinician judgments (r=0.43, p<0.001) in the original concurrent validation study (20).
The borderline tendency scale contains 21 items that assess core emotional, cognitive, and behavioral aspects of the borderline personality disorder diagnosis. The borderline tendency scale showed adequate internal consistency in two validation samples (0.86 and 0.86) and a test-retest (3–7 days) correlation of 0.92 (20).
The Beck Depression Inventory, 21-item version (23, 24), is a well-established and widely used inventory of the cognitive, affective, motivational, and somatic symptoms of depression. It has been researched extensively with adolescents (25), given its fifth-grade readability level (26), and has been shown to have excellent psychometric properties with adolescent patients (25, 27). Strober et al. (27) reported an internal consistency of 0.79, a 0.67 correlation with clinical ratings of depression, and a 5-day, test-retest reliability of 0.69 for a sample of adolescent inpatients.
The Depressive Experiences Questionnaire for Adolescents (28) is a 66-item, self-report questionnaire that assesses experiences noted in the lives of depressed patients but not necessarily regarded as clinical symptoms of depression. Responses are given on a 7-point, Likert-type scale. We focused on the two main factors of the Depressive Experiences Questionnaire for Adolescents (28, 29): interpersonal (dependent) dysphoria and self-critical dysphoria. The first factor, dependency, reflects a depreciated sense of self, dependency, and helplessness. The second factor, self-criticism, reflects self-blame, guilt, and a loss of autonomy. These Depressive Experiences Questionnaire for Adolescents factors have been replicated with community samples of high school students (28–30) and have demonstrated a high level of internal consistency, good retest reliability, and convergent validity (28, 29).
The Hopelessness Scale for Children (31) is a 17-item, true/false scale for children and adolescents that taps into negative future expectations. The Hopelessness Scale for Children has been used with adolescents and has demonstrated good psychometric properties (32, 33). Internal consistency for the Hopelessness Scale for Children (0.97 alpha) is excellent, and test-retest reliability (0.52) is adequate (31).
The Suicide Risk Scale (34) is a 15-item, true/false self-report measure of feelings of hopelessness, present suicidal feelings, past suicidal behavior, and other items that have been shown to be associated with suicide risk. The Suicide Risk Scale has good internal reliability, with a coefficient alpha of 0.74 with adolescents, as well as good sensitivity and specificity (34–36). The Suicide Risk Scale has been cross validated with other inpatient samples and discriminates well between groups of patients who have and have not made suicide attempts (35).
The Past Feelings and Acts of Violence Scale (37) is a 12-item, self-report scale in which responses are coded on a 3-point continuum of frequency. The scale inquires about the frequency of feelings of anger, past acts of violence toward others, use of weapons, and history of arrests. The scale has been demonstrated to have good discriminative validity with adult psychiatric inpatients and with adolescents has been shown to have good internal consistency, item sensitivity, and specificity (38).
The Impulsivity Control Scale (35) is a 15-item, self-report scale designed to assess impulsivity that is independent of aggressive behavior; items are answered on a 3-point frequency scale. With adolescents, the Impulsivity Control Scale has good internal reliability and correlates well with other measures of suicide and violence risk (35, 38).
The Drug Abuse Screening Test—Adolescents (39) is a 27-item, self-report screening measure for substance abuse relevant for adolescent populations that has been adapted from the adult version (40). The Drug Abuse Screening Test—Adolescents has demonstrated good psychometric properties in adolescent inpatient samples. Martino and colleagues (39) reported good internal consistency (0.91 coefficient alpha), 1-week test-retest reliability of 0.89, and a positive predictive power for substance use disorders of 79%.
One hundred and sixty-three subjects comprised the two specific study groups selected for the categorical portion of this study. The 163 subjects were selected from the larger series of 322 admissions on the basis of their scores on the childhood abuse scale of the Millon Adolescent Clinical Inventory. Childhood abuse scale scores of 30 or less and 70 or greater were used to create two study groups: no abuse (N=93) and high abuse (N=70), respectively.
Childhood abuse scale scores of 30 or less did not include endorsements of items directly assessing sexual, physical, or emotional abuse, whereas scores of 70 or greater (reflecting clinically significant elevations) did include endorsements of several items directly tapping abusive experiences. For our overall study group (N=322), a childhood abuse scale score of 30 corresponded to the 30th percentile, and a score of 70 corresponded to the 79th percentile.
To estimate concurrent validity, we tested the childhood abuse scores against information about abuse recorded in the clinical medical record. The records of 45 subjects (28% of cases) were randomly selected for a blind and independent review by a trained post-master’s-degree-level research associate. Subjects were rated by the reviewer as “no abuse” if no report was contained in the medical record, whereas a rating of “high abuse” required documentation of sexual, physical, and/or emotional abuse. Thirty-six (80%) of the 45 medical records were in agreement with the classification of subjects into either the “no abuse” or “high abuse” study groups (χ2=13.75, df=1, p=0.0002, two-tailed test with Yates’s continuity correction; kappa=0.57, p=0.00005).
RESULTS
Categorical Analysis: No Abuse Versus High Abuse
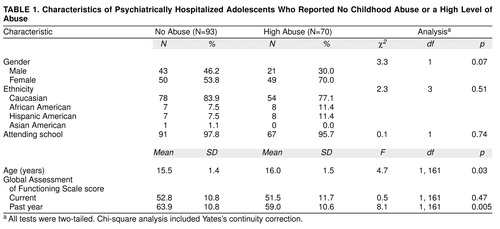
Table 1 summarizes demographic and psychiatric functioning severity data for the two study groups and the statistical tests for significant differences (Yates’s continuity-corrected chi-square analysis for categorical and one-way analyses of variance for continuous data). The no-abuse group was, on average, 0.5 years younger than the high-abuse group. The groups did not differ in regard to gender, ethnicity, or participation in school. Although the two groups did not differ in current Global Assessment of Functioning Scale scores, the no-abuse group had a higher Global Assessment of Functioning Scale score for the previous year.
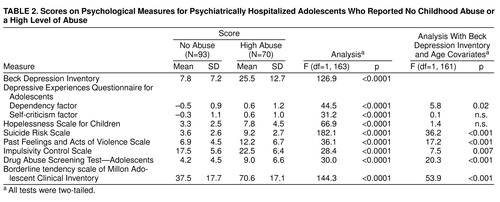
Table 2 summarizes scores on the battery of self-report instruments administered to the two study groups. The high-abuse group reported significantly higher levels of depression, dependency, self-criticalness, hopelessness, suicidality, violence risk, impulsivity, substance use problems, and borderline tendency.
Given the differences between the two study groups in age (0.5-year average difference) and depression scores as measured by the Beck inventory (24), we reanalyzed these findings by covarying for age and Beck inventory scores. Because depressed mood can potentially influence self-reports of psychological functioning, this analytic strategy seemed indicated. As summarized in table 2, the high-abuse group had significantly higher scores than did the no-abuse group on the following measures after covarying for Beck inventory and age: dependency, suicidality, violence, impulsivity, substance use problems, and borderline tendency.
Dimensional Analysis
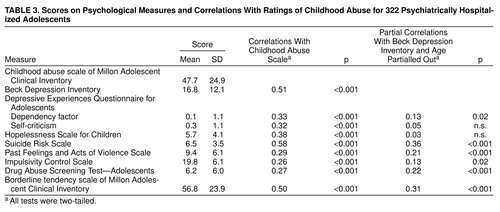
Table 3 summarizes scores for the entire subject group (N=322). Correlations between each measure and the childhood abuse scale were computed. Correlational analyses between each measure and the childhood abuse scale were performed, controlling for depressive mood (by partialling out the Beck inventory scores) and for age. Age is important to control for here because older age allows more time to develop the problematic domains of interest (e.g., substance abuse). As shown in Table 3, childhood abuse scores were significantly associated with the following after controlling for Beck inventory scores and age: dependency, suicidality, violence, impulsivity, substance use problems, and borderline tendency.
DISCUSSION
This study examined symptomatic psychological and behavioral correlates of childhood abuse in a study group of psychiatrically hospitalized adolescents. Two specific study groups (no abuse and high abuse) were created from the same inpatient group. This recruitment procedure should have eliminated some potential selection and sampling confounds (17) found in previous studies. Moreover, the two study groups did not differ in many potentially confounding demographic and severity variables (19). The no-abuse group was slightly younger (0.5 years on average) than the high-abuse group, but otherwise the two groups were comparable.
We found in our group of psychiatrically hospitalized adolescents that patients who report childhood abuse are characterized by a complex array of severe psychological, personality, and behavioral problems that distinguish them from those patients who do not report childhood abuse. Our analyses with age and depression as covariates revealed that the high-abuse group is characterized by higher levels of dependency, suicidality, violence, impulsivity, and substance use problems than is the no-abuse group. This constellation of psychological and behavioral symptoms represents key features of DSM-IV-defined borderline personality disorder. Consistent with this pattern was the finding that the high-abuse group had significantly higher scores on the Millon Adolescent Clinical Inventory borderline tendency scale than the no-abuse group.
Our findings are consistent with the hypothesized association between childhood abuse and borderline personality organization based on findings from a variety of study designs (e.g., 41, 42). Caution is indicated, however, when thinking about possible causality. The cross-sectional nature of this study precludes any such discussion. Indeed, writers have aptly noted that the complex associations between childhood abuse and psychiatric dysfunction can arise, in part, because of a variety of influences, including social, familial, genetic, and contextual factors that are associated with either or both abuse and risk for disorder (1, 3, 11, 41, 42).
The generalizability of our findings may be limited to heterogeneous inpatient populations. Our basic requirements of adequate reading and comprehension and the absence of florid psychosis or severe agitation, while resulting in few exclusions, potentially screened out the most severe spectrum of inpatient cases. Generalizability is further limited to the abuses identifying the high-abuse study group, which represented a heterogeneous collection of abusive experiences (sexual, physical, emotional). Future research can focus on whether psychological correlates vary differentially by characteristics and timing of abuse.
We relied on a self-report battery of instruments and used a computer to administer the questionnaires. These methodologies appear to be particularly useful for assessing sensitive topics (43, 44). In adolescents, this may remove some interpersonal concerns (e.g., embarrassment, distress) or barriers to accurate disclosure of sensitive or personal materials (43). Computerized assessments of self-report instruments similar to those employed here have been found to be favorable to paper-and-pen versions in terms of reliability and validity (45).
The validity of reports of abuse is a complex issue (18). Our report speaks only to the psychological profiles of adolescent inpatients who report or do not report having been abused. We can assert only that the independent review of a random sampling of complete medical records was generally concordant with our characterization of high abuse and no abuse. In our group of psychiatrically hospitalized adolescents, patients who report childhood abuse are characterized by a complex array of severe psychological, personality, and behavioral problems that distinguish them from those patients who do not report childhood abuse. The constellation of symptoms is consistent with borderline personality in statu nascendi.
Received March 10, 1998; revision received Sept. 9, 1998; accepted Oct. 9, 1998. From the Yale Psychiatric Institute and Department of Psychiatry, Yale University School of Medicine, New Haven, Conn . Address reprint requests to Dr. Grilo, Yale Psychiatric Institute, 184 Liberty St., New Haven, CT 06519.
 |
 |
 |
1. Green AH: Child sexual abuse: immediate and long-term effects and intervention. J Am Acad Child Adolesc Psychiatry 1993; 32:890–902Crossref, Medline, Google Scholar
2. Kendall-Tackett KA, Williams LM, Finkelhor D: Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychol Bull 1993; 113:164–180Crossref, Medline, Google Scholar
3. Fergusson DM, Lynskey MT, Horwood LJ: Childhood sexual abuse and psychiatric disorder in young adulthood, I: prevalence of sexual abuse and factors associated with sexual abuse. J Am Acad Child Adolesc Psychiatry 1996; 35:1355–1364Crossref, Medline, Google Scholar
4. Finkelhor D: The international epidemiology of child sexual abuse. Child Abuse Negl 1994; 18:409–417Crossref, Medline, Google Scholar
5. Finkelhor D, Hotaling G, Lewis IA, Smith C: Sexual abuse in a national survey of adult men and women: prevalence, characteristics, and risk factors. Child Abuse Negl 1990; 14:19–28Crossref, Medline, Google Scholar
6. Beitchman JH, Zucker KJ, Hood JE, daCosta GA, Akman D: A review of the short-term effects of child sexual abuse. Child Abuse Negl 1991; 15:537–556Crossref, Medline, Google Scholar
7. Tebbutt J, Swanston H, Oates RK, O’Toole BI: Five years after sexual abuse: persisting dysfunction and problems of prediction. J Am Acad Child Adolesc Psychiatry 1997; 36:330–339Crossref, Medline, Google Scholar
8. Beitchman JH, Zucker KJ, Hood JE, daCosta GA, Akman D, Cassavia E: A review of the long-term effects of child sexual abuse. Child Abuse Negl 1992; 16:101–118Crossref, Medline, Google Scholar
9. Carrey NJ, Butter HJ, Persinger MA, Bialik RJ: Physiological and cognitive correlates of child abuse. J Am Acad Child Adolesc Psychiatry 1995; 34:1067–1075Crossref, Medline, Google Scholar
10. Brown GR, Anderson B: Psychiatric morbidity in adult inpatients with childhood histories of sexual and physical abuse. Am J Psychiatry 1991; 148:55–61Link, Google Scholar
11. Fergusson DM, Horwood LJ, Lynskey MT: Childhood sexual abuse and psychiatric disorder in young adulthood, II: psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry 1996; 35:1365–1374Crossref, Medline, Google Scholar
12. Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP: Childhood sexual abuse and mental health in adult life. Br J Psychiatry 1993; 163:721–732Crossref, Medline, Google Scholar
13. Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT: The relation between methods of coping during adulthood with a history of childhood sexual abuse and current psychological adjustment. J Consult Clin Psychol 1996; 64:1090–1093Crossref, Medline, Google Scholar
14. Widom CS: The cycle of violence. Science 1989; 244:160–165Crossref, Medline, Google Scholar
15. Widom CS: Does violence beget violence? a critical examination of the literature. Psychol Bull 1989; 106:3–28Crossref, Medline, Google Scholar
16. Berkson J: Limitations of the application of four fold table analysis to hospital data. Biometrics Bull 1946; 2:47–53Crossref, Medline, Google Scholar
17. du Fort GG, Newman SC, Bland RC: Psychiatric comorbidity and treatment seeking sources of selection bias in the study of clinical populations. J Nerv Ment Dis 1993; 181:467–474Crossref, Medline, Google Scholar
18. Maughan B, Rutter M: Retrospective reporting of childhood adversity: issues in assessing long-term recall. J Personal Disord 1997; 11:19–33Crossref, Medline, Google Scholar
19. Allison DB: A note on the selection of control groups and control variables in comorbidity research. Compr Psychiatry 1993; 34:336–339Crossref, Medline, Google Scholar
20. Millon T, Millon C, Davis R: Millon Adolescent Clinical Inventory. Minneapolis, National Computer Systems Assessments, 1993Google Scholar
21. Millon T, Davis RD: The Millon Adolescent Personality Inventory and the Millon Adolescent Clinical Inventory. J Counseling and Development 1993; 71:570–574Crossref, Google Scholar
22. Grilo CM, Fehon DC, Walker M, Martino S: A comparison of adolescent inpatients with and without substance abuse using the Millon Adolescent Clinical Inventory. J Youth Adolesc 1996; 25:379–388Crossref, Google Scholar
23. Beck AT, Rush AJ, Shaw BF, Emery G: Cognitive Therapy of Depression. New York, Guilford Press, 1979Google Scholar
24. Beck AT, Steer RA: Manual for the Revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1987Google Scholar
25. Steer RA, Beck AT: Use of the Beck Depression Inventory, Hopelessness Scale, Scale for Suicidal Ideation, and Suicidal Intent Scale with adolescents. Adv Adolesc Mental Health 1988; 3:219–231Google Scholar
26. Berndt DJ, Schwartz S, Kaiser CF: Readability of self-report depression inventories. J Consult Clin Psychol 1983; 51:627–628Crossref, Medline, Google Scholar
27. Strober M, Green J, Carlson G: Utility of the Beck Depression Inventory with psychiatrically hospitalized adolescents. J Consult Clin Psychol 1981; 49:482–483Crossref, Medline, Google Scholar
28. Blatt SJ, Schaffer CE, Bers SA, Quinlan DM: Psychometric properties of the Depressive Experiences Questionnaire for Adolescents. J Pers Assess 1992; 59:82–98Crossref, Medline, Google Scholar
29. Blatt SJ, Hart B, Quinlan DM, Leadbetter B, Auerbach J: Interpersonal and self-critical dysphoria and behavioral problems in adolescents. J Youth Adolesc 1993; 22:253–269Crossref, Google Scholar
30. Luthar S, Blatt SJ: Differential vulnerability of dependency and self-criticism among disadvantaged teenagers. J Res Adolescence 1995; 5:431–449Crossref, Google Scholar
31. Kazdin AE, Rodgers A, Golbus D: The Hopelessness Scale for Children: psychometric characteristics and concurrent validity. J Consult Clin Psychol 1986; 54:241–245Crossref, Medline, Google Scholar
32. Spirito A, Williams CA, Stark LJ, Hart KJ: The Hopelessness Scale for Children: psychometric properties with normal and emotionally disturbed adolescents. J Abnorm Child Psychol 1988; 16:445–458Crossref, Medline, Google Scholar
33. Cole DA: Psychopathology of adolescent suicide: hopelessness, coping beliefs, and depression. J Abnorm Psychol 1989; 98:248–255Crossref, Medline, Google Scholar
34. Plutchik R, van Praag HM, Conte HR: Correlates of suicide and violence risk, I: the suicide risk measure. Compr Psychiatry 1989; 30:296–302Crossref, Medline, Google Scholar
35. Plutchik R, van Praag HM: The measurement of suicidality, aggressivity and impulsivity. Prog Neuropsychopharmacol Biol Psychiatry 1989; 13:523–534Crossref, Google Scholar
36. Plutchik R, van Praag HM, Conte HR: Correlates of suicide and suicide risk, III: a two-stage model of countervailing forces. Psychiatry Res 1989; 28:215–225Crossref, Medline, Google Scholar
37. Plutchik R, van Praag HM: A self-report measure of violence risk, II. Compr Psychiatry 1990; 31:450–456Crossref, Medline, Google Scholar
38. Grosz DE, Lipschitz DS, Sofia E, Finkelstein G, Blackwood N, Gerbino-Rosen G, Faedda GL, Plutchik R: Correlates of violence risk in hospitalized adolescents. Compr Psychiatry 1994; 35:296–300Crossref, Medline, Google Scholar
39. Martino S, Grilo CM, Walker M, Fehon DC: The development of the Drug Abuse Screening Test for Adolescents (DAST-A) in 29th Annual Meeting of the Association for the Advancement of Behavior Therapy. New York, Association for the Advancement of Behavior Therapy, 1995Google Scholar
40. Skinner HA: The Drug Abuse Screening Test. Addict Behav 1982; 7:363–371Crossref, Medline, Google Scholar
41. Sabo AN: Etiological significance of associations between childhood trauma and borderline personality disorder: conceptual and clinical implications. J Personal Disord 1997; 11:50–70Crossref, Medline, Google Scholar
42. Paris J: Childhood trauma as an etiological factor in the personality disorders. J Personal Disord 1997; 11:34–49Crossref, Medline, Google Scholar
43. Erdman HP, Greist JH, Gustafson DH, Taves JE, Klein MH: Suicide risk prediction by computer interview: a prospective study. J Clin Psychiatry 1987; 48:464–467Medline, Google Scholar
44. Fowler RD: Landmarks in computer-assisted psychological assessment. J Consult Clin Psychol 1985; 53:748–759Crossref, Medline, Google Scholar
45. Wilson FR, Genco KT, Yager GG: Assessing the equivalence of paper-and-pencil vs computerized tests: demonstration of a promising methodology. Computers in Human Behavior 1985; 1:265–275Crossref, Google Scholar



