Depressive Symptoms and Health Costs in Older Medical Patients
Abstract
OBJECTIVE: The authors assessed the association between depressive symptoms and health costs for a national Veterans Administration (VA) sample. METHOD: The Rand Depression Index was administered to 1,316 medical or surgical inpatients over the age of 60 at nine VA hospitals. Scores were merged with utilization, demographic, and hospital data from national VA inpatient and outpatient files. RESULTS: Medical costs for respondents with the highest quartile of symptoms were approximately $3,200–or 50%—greater than medical costs for those in the least symptomatic quartile. Depressive symptoms were not associated with any statistically significant mental health expenditures. CONCLUSIONS: The study extends previous reports of the high medical costs associated with depressive disorders to an older, public sector population. The mechanisms underlying increased medical costs associated with depressive symptoms, while the subject of much speculation in the literature, still remain largely unknown. (Am J Psychiatry 1999; 156:477–479)
Older Americans consume a rising portion of health care resources in the United States. By 1995, per capita health care expenditures for Americans over age 65 were $7,038, almost four times that for people under 65. Approximately half of the costs for this population were for inpatient care, in contrast to younger Americans, for whom inpatient costs represented less than one-third of overall expenditures (1).
Inasmuch as health care resources are limited, it has become increasingly important to identify and address treatable causes of excess medical utilization. A growing body of literature has suggested that mental symptoms may be associated with high health care expenditures (2), particularly in primary care settings (3–5). However, authors have noted that fewer than 10% of those health care dollars are spent on specialty mental health treatment (3, 5).
For older patients, there may be an even greater potential for mental symptoms to result in increased medical, rather than mental health, expenditures. Older patients with depression frequently present with somatic complaints, rather than the typical picture seen in younger adults (6). Older patients may also be more hesitant to seek care from mental health providers when they do have symptoms (7). A recent study found that only about 1% of medical costs among elderly patients in a health maintenance organization (HMO) were related to specialty mental health expenditures (8).
We conducted this study to build on, and fill gaps in, the existing literature examining the relationship between mental health symptoms and health care costs in older populations. By examining both overall expenditures and their distribution, we sought to better understand the relationship between depressive symptoms and use of health resources for this population.
METHOD
The Unified Psychogeriatric Biopsychosocial Evaluation and Treatment program (UPBEAT) is a multisite project sponsored by the Department of Veterans Affairs to investigate the costs and outcomes of providing psychiatric case management to older medical-surgical inpatients with heretofore undetected psychiatric morbidity. UPBEAT staff administer a screening instrument to veterans over age 60 who are admitted to VA medical or surgical units and who are not already in psychiatric treatment. Subjects randomly assigned to the UPBEAT intervention receive case coordination and psychiatric evaluation and treatment, in addition to their usual medical care. To preserve the naturalistic design of this study, we examined only subjects not randomly assigned to the active intervention arm of the UPBEAT study (N=1,316).
The depression screening instrument used for UPBEAT was the depression subscale from the 38-item Rand Mental Health Index (9, 10). We compared use of services for individuals within each quartile of scores on this depression instrument.
Using Social Security numbers as identifiers, we linked UPBEAT screening data to demographic and utilization data derived from national VA administrative files. Costs were estimated by multiplying numbers of units consumed for each type of service (inpatient days or outpatient visits) by national mean unit costs for substance abuse, psychiatric, medical, and surgical services derived from the VA Cost Distribution Report.
In order to estimate the costs attributable to depressive symptoms over and above differences due to demographic and other variables, we used ordinary least squares regression to calculate least square means adjusting for those covariates. The dependent variable for each model was a measure of estimated inpatient or outpatient medical or psychiatric costs for the 6 months after discharge from the index admission. Covariates in each model included age, race, sex, income, geographic region, receipt of VA compensation payments, number of medical diagnoses, and use of VA health or mental health services in the 6 months before admission. Because of the skewed distribution of utilization and cost data, log-transformation was used in all statistical comparisons.
RESULTS
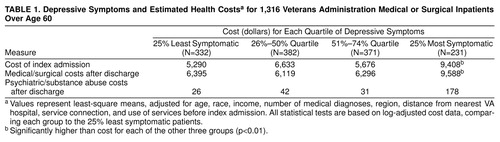
As can be seen in table 1, among individuals with the highest quartile of depressive symptoms, costs of the index admission were 77% higher than costs for patients in the least symptomatic quartile. During the first 6 months after discharge, this group’s costs were 50% higher than those of the least symptomatic group and were also significantly different from costs for the two middle quartiles. These costs were almost entirely attributable to inpatient expenditures—individuals in the most symptomatic quartile used more inpatient medical days than people in the lowest quartile (8.62 days versus 5.09 days) (t=4.28, df=1261, p=0.0008) but did not use significantly more outpatient expenditures.
Mental health costs were only 0.4% of medical costs for the group with the lowest percentile of depressive symptoms. For the most symptomatic group, these costs were still only 1.8% of medical expenses, which did not represent a significant increase over costs for individuals with the least depressive symptoms.
CONCLUSIONS
Before discussing the findings in greater detail, we should discuss the potential limits of these data for examining the relationship between depressive symptoms and health services use. First, the VA population is largely male, relatively poor, and medically sicker than the general U.S. population. However, this sample may provide a useful complement to samples drawn from HMOs, which treat populations that may be healthier and more affluent than the U.S. population as a whole. Second, by screening inpatients, we are sampling a population that uses more services than the general population or outpatient samples. However, “high utilizers” may be a particularly important group to study because they consume large amounts of resources that could otherwise be allocated to the remainder of the population (11).
The results indicate that for older patients, high levels of depressive symptoms are a strong predictor of increased medical expenditures, extending findings from previous studies of older individuals (8) to a national sample of patients treated in the public sector. The 50% increase in costs found among these patients was comparable to that found in other similar studies.
While the literature has consistently found a strong association between depressive symptoms and medical costs in different populations, it has been less successful in identifying the mechanisms underlying those costs. Understanding those mechanisms may be a crucial first step in developing interventions designed to offset those costs. If greater psychological distress is primarily a marker for greater severity of medical illness, then interventions should be targeted toward treating that underlying medical morbidity, rather than focusing on the psychological symptoms. If psychiatric comorbidity in the course of medical illness causes excess service use, then more expenditures should be targeted toward detecting and treating those psychiatric illnesses. Finally, if high service use reflects patterns of chronic illness behavior distinct from medical or psychiatric illness, then interventions should target that behavior in addition to the medical or psychological symptoms.
The causal mechanisms underlying the link between depressive symptoms and increased medical utilization still remain largely a black box. Further research should look toward unlocking that box as a first step toward improving this group’s physical and mental health and to better understand the most appropriate allocation of physical and mental resources for this population.
Received Feb. 27, 1998; revision received June 26, 1998; accepted Sept. 9, 1998. From the Northeast Program Evaluation Center, VA Healthcare System, and the Departments of Psychiatry and Public Health, Yale University, West Haven, Conn. Address reprint requests to Dr. Druss, 950 Campbell Ave./182, West Haven, CT 06516; [email protected] (e-mail). Supported in part by grants from the Donaghue Medical Research Foundation and from the National Alliance for Research on Schizophrenia and Depression. The authors thank the following individuals who designed and implemented the Unified Psychogeriatric Biopsychosocial Evaluation and Treatment program: L. Jarvik, M.D., Ph.D.; R. Andersen, Ph.D.; R. Bastani, Ph.D.; R. Gould, Ph.D.; G. Kominski, Ph.D.; A. Maxwell, Dr.P.H.; J. Rosansky, L.C.S.W.; J. Sanchez, Ph.D.; S. Morse, A.C.S.W.; A. Keskiner, M.D.; J. Moye, Ph.D.; L. Messinides, Ph.D.; A. Bagheri, M.D.; E. Olsen, M.D., M.B.A.; G. Aubel, R.N.; L. Harkness, Ph.D.; D. Coutsouridis, A.C.S.W.; and C. McDermott, M.S.W.
 |
1. Agency for Health Care Policy and Research, Center for Cost and Financing Studies: Trends in Personal Health Care Expenditures, Health Insurance, and Payment Sources, Community-Based Population, 1987–1995, March 1997. http://www.meps.ahcpr.gov/nmes/papers/trends/intnet4d.pdfGoogle Scholar
2. Druss BG, Rosenheck RA: Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatr Serv 1999; 50:214–218Link, Google Scholar
3. Simon G, Ormel J, VonKorff M, Barlow W: Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry 1995; 152:352–357Link, Google Scholar
4. Simon G, Von Korff M, Barlow W: Health care costs of primary care patients with recognized depression. Arch Gen Psychiatry 1995; 52:850–856Crossref, Medline, Google Scholar
5. Henk HJ, Katzelnick DJ, Kobak KA, Greist JH, Jefferson JW: Medical costs attributed to depression among patients with a history of high medical expenses in a health maintenance organization. Arch Gen Psychiatry 1996; 53:899–904Crossref, Medline, Google Scholar
6. Blazer DG, Hughes DC, George LK: The epidemiology of depression in an elderly community population. Gerontologist 1987; 27:281–287Crossref, Medline, Google Scholar
7. Shapiro S, Skinner EA, Kessler LG, Von Korff M, German PS, Tischler GL, Leaf PJ, Benham L, Cottler L, Regier DA: Utilization of health and mental health services: three Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1984; 41:971–978Crossref, Medline, Google Scholar
8. Unutzer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W: Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA 1997; 277:1618–1623Crossref, Medline, Google Scholar
9. Veit CT, Ware JE: The structure of psychological distress and well-being in general populations. J Consult Clin Psychol 1983; 51:730–742Crossref, Medline, Google Scholar
10. Weinstein MC, Berwick DM, Goldman PA, Murphy JM, Barsky AJ: A comparison of three psychiatric screening tests using receiver operating characteristic (ROC) analysis. Med Care 1989; 27:593–607Crossref, Medline, Google Scholar
11. Von Korff M, Ormel J, Katon W, Lin EH: Disability and depression among high utilizers of health care: a longitudinal analysis. Arch Gen Psychiatry 1992; 49:91–100Crossref, Medline, Google Scholar



