Posttraumatic Stress Disorder Following an Air Disaster: A Prospective Study
Abstract
OBJECTIVE: The purpose of this study was to determine predictors of posttraumatic stress disorder (PTSD) in health care workers exposed to a disaster, in order to facilitate early case identification and prevention of subsequent morbidity. METHOD: Following an air disaster, 355 military medical health care workers were studied over an 18-month follow-up period. Measures included assessment of peritraumatic reactions associated with the disaster, the frequency of other stressful events after the disaster, and standard PTSD rating scales at 6, 12, and 18 months. RESULTS: Multivariate logistic regression of data on health care workers who cared for victims of the air disaster showed that PTSD was more likely to develop in those who had not completed college, those who had worked with burn victims, those who had experienced more stressful life events in a period of approximately 6 months following the disaster, and those who experienced emotional numbness immediately after the disaster. CONCLUSIONS: Results suggest that lower levels of education, exposure to grotesque burn injuries, stressful life events following exposure, and feelings of numbness following exposure are useful predictors of subsequent development of PTSD. (Am J Psychiatry 1998; 155:934–938)
Studying the effects of disastrous events on groups of exposed individuals provides an opportunity to facilitate case detection and treatment. Although early case identification is particularly important for organizations whose employees have a high likelihood of traumatic exposure, sporadic and unexpected common disasters can occur in almost any industry, community, or organization where large numbers of people are exposed to serious trauma. Identification of individuals most at risk for posttraumatic stress disorder (PTSD) following a mass disaster would be very useful for organizations wishing to prevent the enormous human and economic cost of this disease and would enable them to focus limited resources toward providing early treatment and morbidity prevention.
Risk factors for PTSD identified in previous research include the duration and degree of exposure to the trauma (1, 2), the presence of physical injury and threat to life (3), the additive effect of other stressful life events on the index trauma (4), level of social support (5), the individual's initial psychological reaction to the trauma (6–9), genetic inheritance (10), gender (11, 12), level of education (1, 8), intelligence (13), and preexisting mental traits or disorders (11, 14).
Unfortunately, most previous research seeking to identify risk factors for PTSD has been based primarily on retrospective or cross-sectional analysis. These methods rely heavily on subjects' reports of conditions and events occurring in the relatively distant past. Since PTSD frequently follows a relapsing and remitting course, a more reliable and useful screening method should be based on prospective research. Findings from cross-sectional and retrospective studies are limited by the fact that affected individuals whose symptom levels fail to meet clinical triggers at one time might later meet classification criteria for PTSD. In addition, the avoid~ant component of PTSD frequently leads to disturbances of recall (15).
As part of our overall effort to develop reliable criteria for screening large groups following mass trauma, we present here the results of a prospective study of 355 military health care workers who experienced varying levels of involvement with victims of the Ramstein air disaster in August 1988. Although we studied a number of other factors pertinent to stress response, this report will focus on those measurements which are of substantial clinical importance and could be readily adapted by organizations wishing to screen for PTSD those workers exposed to a common traumatic event. These clinically practical variables include the nature of the traumatic exposure, subjects' demographic characteristics, life stress from other events following the index trauma, and subjects' reported initial emotional response to the trauma.
METHOD
A midair collision occurred at the annual Ramstein Air Force Base air show on Aug. 28, 1988. Before the crash, spectators were enjoying an outdoor air show that featured booths and refreshments in a festive family atmosphere. After the collision, burning debris from the crash was suddenly scattered over a wide area, killing 70 of the approximately 300,000 spectators and injuring 500. The extent of death and injury created pandemonium at the scene. Victims were lying on the ground everywhere. Most of the wounded suffered burns. As the result of heroic efforts, all injured were evacuated within 90 minutes to area hospitals. In some instances, family members were unable to locate victims for several days because the severity of their burns delayed identification.
A first cohort of medical care workers from two military bases, Ramstein Air Force Base and Landstuhl Army Regional Medical Center (N=254), were surveyed approximately 2 months after the Ramstein Air Force Base disaster (October–November 1988) and again at approximately 6 months (March–April 1989), 12 months (September 1989), and 18 months (April 1990). A second cohort of health care workers at Ramstein Air Force Base and Landstuhl Army Regional Medical Center (N=101) were surveyed only at 6, 12, and 18 months. This study will examine assessments of PTSD that were made at 6, 12, and 18 months (combined group of both cohorts, N=355).
Recruiting methods differed somewhat at the two locations. Workers at the health clinic dispensary at Ramstein Air Force Base were contacted through the mail. At Landstuhl Army Hospital, a more comprehensive medical facility, health workers were contacted on a day when all were required to come for their flu shots. Because of its importance as a military evacuation hospital, personnel at Landstuhl were more likely to have had previous experience with victims from other disasters than those at Ramstein. Follow-up surveys at 6, 12, and 18 months were distributed and returned by mail. All subjects participating in this study were provided a description of the study and responsibilities involved in participation, after which written informed consent was obtained.
Probable PTSD cases were identified by using a multimethod approach with self-administered scales that have shown an acceptable level of sensitivity and specificity (16, 17). More recently, we have validated the multimethod scales (18) in a population of motor vehicle accident victims whose PTSD diagnoses were also tested with the clinician-administered Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP) (19). The multimethod scales predicted PTSD as diagnosed by the SCID-NP with a very high sensitivity, specificity, and overall percent correct. The multimethod scales employ scores from the SCL-90-R (20), augmented by 13 additional items created to cover all DSM-III-R symptoms of PTSD, and from the total Impact of Event Scale (21). Subjects were classified as having probable PTSD if they met DSM-III-R PTSD symptom distribution criteria on the augmented SCL-90-R and scored greater than 19 on the Impact of Event Scale (17).
Subjects were asked open-ended questions regarding their emotional reactions to the disaster and its aftermath. Written answers were classified into five categories of emotional response that included feeling depressed/sad, anxious/frightened, guilty, numb/zombie-like, and disbelief/confusion. Disagreements on classification were resolved by consensus among four clinician researchers who were highly knowledgeable about posttraumatic symptoms, in general, and who were blind to respondents' PTSD diagnoses.
In order to assess the effects on outcome of postdisaster stressful life events (22), apart from exposure to the focal trauma of the air disaster and its aftermath, we surveyed subjects about stressful life events they might have experienced during the 6-month period after the disaster. Subjects were queried about their health care work with disaster victims including child patients, burn patients, emergency room work, dead bodies, and patients who later died. Other questions surveyed the subjects' proximity to the actual disaster scene, worry about family members, and whether they had an opportunity for debriefing.
Statistical analysis employed SAS, version 6.1 (23). Analyses were conducted by using chi-squares under PROC FREQ, tests for difference of means under PROC ANOVA, and univariate or multivariate logistical regression through use of PROC LOGISTIC. Multivariate logistical modeling of PTSD based on independent variables was conducted according to the model building strategies recommended by Hosmer and Lemeshow (24).
RESULTS
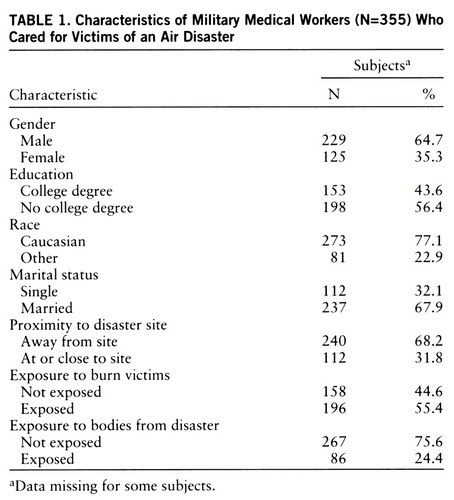
A total of 355 respondents returned valid surveys. Respondents' average age was 31.9 years (SD=8.2), with a range from 19 to 59 years. Of the total group, 35.3% were women, 67.9% were married, 43.6% had completed a college degree, 77.1% were Caucasian, and 55.4% were exposed to burn victims (table 1).
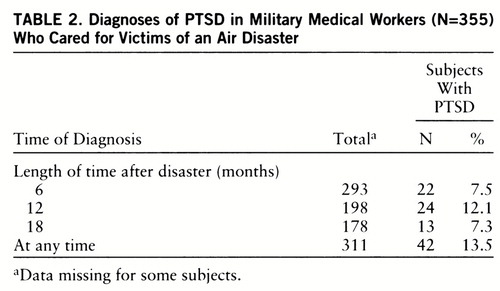
Forty-two (13.5%) of 311 individuals with nonmissing data for the variable were found to have PTSD at 6, 12, or 18 months. Numbers and percentages of subjects with PTSD identified at any of the three follow-up times are summarized in table 2. Longitudinal assessment of our respondents revealed that the frequency of cases of PTSD peaked at 12 months (12.1%). By 18 months, case frequency had diminished to 7.3%. Stress symptoms, as measured by Impact of Event Scale scores, were also higher at 12 months but did not diminish quite as rapidly by 18 months as would have been expected by PTSD case frequency alone.
Of those subjects studied at 6 months, 29% did not complete the assessment at 12 months. Similarly, of those studied at 6 months, 31% failed to complete assessments at 18 months. Subjects older than 39 were significantly less likely than younger subjects to fail to complete their assessments at either 12 months (failure rate=15.3%, N=355) (χ2=8.43, df=2, p=0.02) or 18 months (failure rate=19.4%, N=355) (χ2=6.03, df=2, p=0.05). Women were significantly more likely than men not to complete their assessments at 12 months (failure rate=38.4%, N=354) (χ2=8.14, df=1, p=0.004) but were not significantly different from men in their completion rate at 18 months (failure rate=36.8%, N=354) (χ2=2.96, df=1, p=0.09). Failure to complete the survey assessment at either 12 or 18 months was not significantly associated with marital status, race, the presence of PTSD, or any of the variables that were significantly associated with PTSD on either univariate or multivariate analysis.
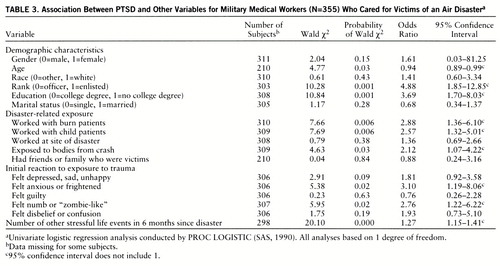
Univariate logistic regressions for demographic variables showed that subjects who developed PTSD at 6, 12, or 18 months were likely to be younger, were more likely to be of enlisted rank, to have less education, to have worked with burn victims, to have worked with child victims, to have been exposed to bodies from the disaster, to have been anxious or frightened after the disaster, and to have felt numb or “zombie-like” and were likely to have experienced more frequent stressful life events in the 6 months after the disaster. These findings, along with the 95% confidence intervals and odds ratios for all variables, are summarized in table 3.
Overall, 17.1% of women and 11.3% of men met criteria for PTSD at some point during the assessment period. The higher prevalence of women who developed PTSD did not reach statistical significance (odds ratio=1.61, 95% confidence interval=0.03–81.25). Of 298 respondents who provided complete data on the number of other stressful life events following the disaster, there was an average of 3.3 (SD=2.9, range=0–17) such events. Individuals who developed PTSD at 6, 12, or 18 months experienced, on average, a significantly higher number of other stressful life events (mean=5.4, SD=3.4) during the first 6 months after the disaster than subjects without PTSD (mean=3.0, SD=2.7) (F=26.39, df=1,296, p<0.0001) (table 3).
Multivariate logistical regression analyses were conducted to control for the association between independ~ent variables and to identify the best predictors of PTSD. A preliminary stepwise model included all variables with a univariate Wald chi-square probability value of 0.25 or less (table 3), in order to avoid excluding variables that might be weakly associated with PTSD on univariate analysis but that might contribute collectively with other variables as important predictors of outcome in the logistic equation. Variables meeting this entry criterion for the preliminary stepwise regression included demographic variables (female gender, age, rank, education), disaster-related exposure variables (working with burn victims, working with child victims, exposure to bodies from the disaster), initial emotional reaction variables “felt anxious or frightened” and “felt numb or zombie-like,” and number of other stressful life events 6 months after the disaster. Five variables were selected into the logistic model by the preliminary stepwise procedure. These included female gender, having an educational level with less than a bachelor's degree, having worked with burn victims from the disaster, having experienced a higher frequency of other stressful life events 6 months following the disaster, and having felt numb or zombie-like in reaction to the disaster. When these five variables alone were fitted into a logistic model, we found that the Wald chi-square statistic for female gender had an unacceptably high probability value (p=0.41, odds ratio=1.37, 95% confidence interval=0.65–2.85), and, therefore, we decided to remove this variable from the final model. The four remaining variables in our final model (N=290 with nonmissing data for all variables) included education below a bachelor's degree (Wald χ2=7.63, p=0.006, odds ratio=3.19, 95% confidence interval=1.40–7.26), having worked with burn patients from the disaster (Wald χ2=5.11, p=0.02, odds ratio=2.63, 95% confidence interval=1.14–6.09), number of stressful events within 6 months after the disaster (Wald χ2=13.50, p=0.0002, odds ratio=1.23, 95% confidence interval=1.10–1.37), and having felt numb or zombie-like after the disaster (Wald χ2=2.74, p=0.10, odds ratio=2.15, 95% confidence interval=0.87–5.32). The Hosmer-Lemeshow goodness-of-fit statistic indicated a satisfactory model (goodness-of-fit=4.04, df=8, p=0.85).
Although the variable “felt numb or zombie-like” had an odds ratio whose 95% confidence interval included 1.0, we decided to retain it in the final logistic model because of substantial evidence from other studies indicating that peritraumatic numbness is a clinically important predictor of PTSD (8, 25), the high skew of its confidence interval beyond unity, and its statistically significant univariate 95% confidence interval.
DISCUSSION
Multivariate logistic regression revealed that lower educational level, exposure to burn victims, a greater number of stressful life events after the trauma, and feeling numb at the time of exposure independently predicted PTSD outcome. These findings are consistent with previous research (1, 8). An individual's level of education is a multidetermined characteristic that is likely to be related to other factors known to modulate adaptability to stress, such as intelligence, level of experience, level of authority, and sense of environmental mastery. Although exposure to bodies and child victims significantly correlated with PTSD outcome on univariate analysis, multivariate analysis showed that caring for victims with grotesque burn injuries was the best exposure predictor of PTSD in our group. This finding corroborates previous work (17).
The finding that postdisaster stressful life events predict PTSD in the logistic model suggests that life events after a disaster play an important role in an individual's ability to metabolize trauma (26), rather than sensitizing individuals to new trauma. Yehuda and colleagues (4), studying Holocaust victims, found that other lifetime trauma and recent stressful events had an additive effect on the severity of PTSD symptoms (primarily avoidant) over and above effects of having survived the Holocaust itself. The finding that recent life events are likely to affect PTSD outcome has important clinical ramifications, since it may be possible to shelter trauma victims and help them to stabilize their lives.
Feeling numb shortly after the disaster was reported more than twice as frequently in individuals who subsequently developed PTSD. Although our measure, based on clinician ratings of responses, needs further psychometric assessment, this finding is consistent with the basic clinical underpinnings of the posttraumatic syndrome. Numb and zombie-like feelings are particularly important because they are an indication of a dissociative response to trauma, which has been shown to predict negative outcome (25, 27). Shalev and colleagues (8) found that peritraumatic dissociation was strongly correlated with development of PTSD after 6 months and predicted 29.4% of the variance of symptom intensity. They suggested that dissociative symptoms were evidence of defensive operations learned from previous life experiences and, therefore, could be seen both as a marker of greater vulnerability and as a maladaptive defense that could interfere with healthy mental processing of traumatic experiences.
It is important to note that all respondents in our study were military personnel previously screened for good health and achievement of at least a high school education. This factor may limit the generalizability of our findings to other populations; however, there are also many similarities between a relatively young workforce and other populations that may be at special risk for traumatization, such as police, firefighters, emergency medical personnel, and employees in certain industries. The use of a categorical measure for PTSD has some advantages but also some psychometric limitations. Further efforts are needed to test and employ predictive paradigms such as the one we have developed in this report and to examine the components of PTSD (intrusive, avoidance, and arousal) separately. Future research and replications of our findings are needed to identify health care workers at risk for PTSD and its associated morbidity.
 |
 |
 |
Received July 17, 1996; revisions received Oct. 14 and Dec. 22, 1997; accepted Jan. 15, 1998. From the Department of Psychiatry, Uniformed Services University of the Health Sciences. Address reprint requests to Dr. Ursano, Department of Psychiatry, Uniformed Services University of the Health Sciences, 4301 Jones Bridge Rd., Bethesda, MD 20814.
1 Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
2 Shore JH, Tatum EL, Vollmer WM: Psychiatric reactions to disaster: the Mount St Helen's experience. Am J Psychiatry 1986; 143:590–595Link, Google Scholar
3 Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984–991Crossref, Medline, Google Scholar
4 Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL: Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in Holocaust survivors. Am J Psychiatry 1995; 152:1815–1818Link, Google Scholar
5 Green BL, Grace MC, Lindy JD, Gleser GC, Leonard A: Risk factors for PTSD and other diagnoses in a general sample of Vietnam Veterans. Am J Psychiatry 1990; 147:729–733Link, Google Scholar
6 Feinstein A, Dolan R: Predictors of post-traumatic stress disorder following physical trauma: an examination of the stressor criterion. Psychol Med 1991; 21:85–91Crossref, Medline, Google Scholar
7 Mayou R, Bryant B, Duthie R: Psychiatric consequences of road traffic accidents. BMJ 1993; 307:647–651Crossref, Medline, Google Scholar
8 Shalev AY, Peri T, Canetti L, Schreiber S: Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996; 153:219–225Link, Google Scholar
9 McFarlane AC: Posttraumatic phenomena in a longitudinal study of children following a natural disaster. J Am Acad Child Adolesc Psychiatry 1987; 26:764–769Crossref, Medline, Google Scholar
10 True WR, Rice J, Eisen SA, Heath AC, Goldberg J, Lyons MJ, Nowak J: A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry 1993; 50:257–264Crossref, Medline, Google Scholar
11 Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
12 Breslau N, Davis GC: Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. Am J Psychiatry 1992; 149:671–675Link, Google Scholar
13 McNally RJ, Shin LM: Association of intelligence with severity of posttraumatic stress disorder in Vietnam combat veterans. Am J Psychiatry 1995; 152:936–938Link, Google Scholar
14 Roca RP, Spence RJ, Munster AM: Posttraumatic adaptation and distress among adult burn survivors. Am J Psychiatry 1992; 149:1234–1238Link, Google Scholar
15 Epstein RS: Avoidant symptoms cloaking the diagnosis of PTSD in patients with severe accidental injury. J Trauma Stress 1993; 6:451–458Crossref, Google Scholar
16 Ursano RJ, Fullerton CS, Kao TC, Bhartiya VR, Dinneen MP: PTSD in community samples: development of a self-report instrument, in Proceedings of the International Society of Traumatic Stress Studies. World Conference, Amsterdam. Chicago, International Society for Traumatic Stress Studies, 1992, p 54Google Scholar
17 Ursano RJ, Fullerton CS, Kao TC, Bhartiya VR: Longitudinal assessment of posttraumatic stress disorder and depression after exposure to traumatic death. J Nerv Ment Dis 1995; 183:36–42Crossref, Medline, Google Scholar
18 Fullerton CS, Crowley B, Ursano RJ, Epstein RS, Craig KJ, Baum AS: PTSD in community samples: a measurement problem, in 1997 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1997, p 202Google Scholar
19 Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
20 Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
21 Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209–218Crossref, Medline, Google Scholar
22 Holmes TH, Rahe RH: The Social Readjustment Rating Scale. J Psychosom Res 1967; 11:213–218Crossref, Medline, Google Scholar
23 SAS/STAT User's Guide, version 6.01. Cary, NC, SAS Institute, 1990Google Scholar
24 Hosmer DW, Lemeshow S: Model-building strategies and methods for logistic regression, in Applied Logistic Regression. New York, John Wiley & Sons, 1989, pp 82–134Google Scholar
25 Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902–907Link, Google Scholar
26 Ursano RJ, Fullerton CS, McCaughey BG: Trauma and disaster, in Individual and Community Responses to Trauma and Disaster: The Structure of Human Chaos. Edited by Ursano RJ, Mc~Caughey BG, Fullerton CS. London, Cambridge University Press, 1994, pp 3–30Google Scholar
27 Spiegel D, Cardena E: Disintegrated experience: the dissociative disorders revisited. J Abnorm Psychol 1991; 100:366–378Crossref, Medline, Google Scholar



