Family Structure and Depressive Symptoms in Men Preceding and Following the Birth of a Child
Abstract
OBJECTIVE: The prevalence and etiology of pre- and postpartum depressive symptoms in women in a variety of family forms have been well documented, but relatively little research has been conducted on the adjustment of their male partners. The authors' goals in this study were 1) to estimate rates of depression during the pregnancy and 8 weeks following the birth of a child in a large representative community sample of fathers in different family structures and 2) to explore the role of stressful life events, social and emotional support, the quality of the partner relationship, and socioeconomic circumstances. METHOD: This study describes the relations of family setting and other correlates to men's depressive symptoms during the pregnancies (18 weeks gestation, on average) and 8 weeks after the births of children for 7,018 partners of female participants in the Avon Longitudinal Study of Pregnancy and Childhood. RESULTS: Men living in stepfamilies had significantly higher levels of depressive symptoms before and after the birth than did men in more traditional families. The effect of stepfamily status on depression was mediated by education, life events, social support, social network, and level of aggression in the partnership. CONCLUSIONS: There are similarities in the patterns and correlates of depression after the birth of a child for men and women. These findings point to the importance of family and partnership ecology in the adjustment of men before and after the birth of a child.
Family dysfunction and adult psychopathology have been linked to family structure. Studies of representative samples have shown that children and adults in stepfamilies are at greater risk for psychosocial adjustment problems than children and adults in families with no divorces or similar disruptions (1–3). A link between family type and depression has been reported in women: women in stepfamilies are at greater risk for depression (4, 5). A recent community sample study of mothers preceding and following the birth of a child (6) showed that this effect of family type was due, in part, to the fact that women in stepfamilies had experienced more marital conflict and disruptions, more stressful life events, and less social support than had women in traditional families. However, little is known about the adjustment of men in these different family forms preceding and following the birth of a child.
Epidemiologic studies have shown higher rates of depression among women than men (7–9). Although the magnitude of this difference varies across studies because of differences in methodology and sample selection, the findings indicate that women are twice as likely to suffer from depression in their lifetimes (10%–20% prevalence) than are men (5%–10% prevalence). However, these studies have not explored these gender differences with respect to family type.
Antenatal and postnatal depression have been investigated because the period surrounding the birth of a child is a time of risk for depression in some, and because there is evidence linking women's postpartum emotional disturbance to their children's poorer social-emotional and cognitive outcomes (10–12). Depression is familial (13), and although genetic transmission has been implicated (14), phenotypic studies of family processes have demonstrated that a parent's depressive symptoms preceding and following a child's birth is associated with the child's long-term social-emotional and cognitive outcomes through its impact on parent-child interaction, for both mothers (15–17) and fathers (18). Having two depressed parents is associated with worse social and emotional adjustment for children than is having a depressed mother (19).
A recent meta-analysis (20) showed that 13% of women experience depression in the postnatal period, a rate that is consistent across a variety of cultural and ethnic groups (21). There is also evidence from an earlier report (22), based on the mothers in the sample studied here, that rates of depression decrease across the ante- and postnatal periods.
Fathers also need to adjust during pregnancy and after childbirth, and there is evidence that some men experience a decline in physical and psychological health after a child's birth, particularly if they are inexperienced with child care (23). Direct comparisons of mothers and fathers have shown that they have similar levels of parenting-related stress and anxiety (24). However, whether men and women show similar rates and correlates of depressive symptoms during the pre- and postpartum period remains an important question to be answered.
Even though the quality of the partner relationship is important to women's adjustment to pregnancy and motherhood (25–27), there has been little research on the psychosocial adjustment in male partners preceding and following the birth of a child. This is apparent in comparing two recent reviews of the literature on depression among women (20) and their male partners (28) during the postpartum period. O'Hara and Swain's meta-analysis (20) included nearly 13,000 women in numerous community and clinical samples. Ballard and Davies (28) reviewed the handful of studies available—only one of which was based on a community sample—that together included 466 men. In the community sample, the prevalence of depression was 10% at 6 weeks postpartum and 5% at 6 months postpartum. In all of these studies, the psychosocial adjustments of mothers and fathers in the postpartum period were linked in that depressive symptoms were more prevalent among partners of depressed women (29, 30).
There are several risk factors for depressive symptoms among men preceding and following the birth of a child. Research on the correlates of men's depressive symptoms following the birth of a child points to similarities with, rather than differences from, the findings for women. Higher rates of depression following the birth of a child have been found for those men who are unemployed, who have less satisfactory and more conflicted relationships with their partners, and who have less emotional and social support from family and friends. However, much of this research has focused on volunteer and selected samples and has not taken family type (stepfamily or traditional family) into account. The current study contributes to this literature by studying levels and correlates of depressive symptoms following the birth of a child in a large, representative community sample of men in different types of families.
Our first aim in this study was to estimate the prevalence of depression during the pregnancy and 8 weeks following the birth of a child in a large representative community sample of fathers in different family structures. Our second aim was to explore the role of several mediating factors that have been emphasized in past research, including stressful life events, social and emotional support, the quality of the partner relationship, and socioeconomic circumstances (31–33).
METHOD
Subjects
The sample included 7,018 partners of women in the Avon Longitudinal Study of Pregnancy and Childhood, an ongoing study including all of the pregnant women in Avon County (including the city of Bristol), England, who gave birth between April 1, 1991, and December 31, 1992 (34). Avon contains urban and rural areas and is representative of Britain. The majority of eligible women (85%) participated. To be included in the current study, the same male partner had to complete one of two assessments of depressive symptoms.
Procedure
Participants completed mailed questionnaires before and after the birth of their children. The current study focuses on data from two male partner questionnaires. The first—completed at 18 weeks gestation (on average)—included measures of depression, life events, social support, qualities of the partner relationship, and demographic information. The second—completed 8 weeks following the birth of the child—included another administration of the depression questionnaire. Data from the first mothers' questionnaire—completed at 14 weeks gestation, on average—included information on the household's socioeconomic circumstances. Mothers also reported their own depressive symptoms at 18 weeks gestation and 8 weeks postpartum. Participants were sent a brochure before we started the study, guaranteeing anonymity and confidentiality, and were informed that by completing the questionnaires they were granting consent to participate in the study.
Measures
Depression. Participants completed the 10-item Edinburgh Postnatal Depression Scale (35), a widely used, validated measure of depressive symptoms in the antenatal and postnatal period (36). Partners and mothers completed the Edinburgh Postnatal Depression Scale during the pregnancy (18 weeks gestation on average) and 8 weeks after the birth. For most of the analyses we used the continuous Edinburgh Postnatal Depression Scale scores (coefficient alpha=0.82), but these were also dichotomized by using a threshold score of greater than 12 (37) to estimate prevalence rates.
Family structure. Men were categorized according to four family types based on the mothers' reports of household structure: traditional families (both parents reside in the home and all the children are biologically related to the parents), stepfather families (two parents resident with stepchildren of the father, with or without biologically related children), stepmother families (two parents resident with stepchildren of the mother, with or without biologically related children), and single-mother families (a mother who has identified a nonresident partner). Families where there were stepchildren of both parents were included in the stepfather group for this study.
Demographic factors. Each male partner reported his age (years), highest education qualifications (none, some high school, high school diploma, or college degree or higher), and employment status (unemployed or employed). There were no income data, so socioeconomic circumstances were estimated from the mothers' reports on three items regarding housing conditions: type of home (room or other, apartment, row or town house, duplex, or detached house), ownership status (renting or mortgaged/owned), and crowding (less than one room per person or more than one room per person).
Life events. At 18 weeks gestation, each male partner completed an inventory of 40 stressful life events experienced since the expectant mother had become pregnant, a list of events derived from several sources (38, 39). A weighted life events score (alpha=0.72) was derived by summing the estimated impact of each event that had occurred (0=did not happen to 4=affected me a lot).
Social support and social network. Partners completed a 10-item questionnaire (summed into a composite score) regarding their perceptions of the emotional and instrumental support they received from others, using a 4-point Likert-type scale (alpha=0.69). Partners also completed a scale of 10 questions regarding the number of people in their support networks (alpha=0.75).
Quality of partnership. Each male partner completed nine items rated on a 5-point Likert-type scale (1=almost always to 5=never) regarding levels of aggression and lack of affection in his relationship with his pregnant partner. The aggression scale included three summed items (alpha=0.82), and the lack of affection scale included six items (alpha=0.84).
Relationship history. Partners reported the number of marital or cohabiting relationships they had prior to their current partnerships (none, one, or two or more).
RESULTS
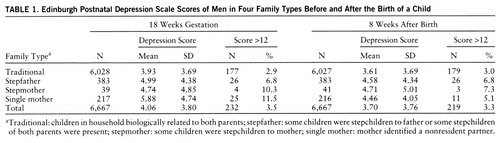
The mean scores reflecting depressive symptoms in the men before and after the birth of the child are shown in table 1. These means varied significantly by family type before the birth (F=27.59, df=3,6663, p<0.001) and after the birth (F=12.03, df=3,6663, p<0.001, linear regression). A Bonferroni multiple-comparison test revealed that there were significant differences (p<0.05) before and after the child's birth between stepfather families and traditional families as well as between single-mother families and traditional families.
Although the primary analyses focused on the statistical prediction of the continuous Edinburgh Postnatal Depression Scale scores, we explored the rates of depression using a threshold score of greater than 12. Using this as our criterion, we estimated the rates of depression before and after the birth of the child (table 1). These rates varied significantly by family type: men in stepfamilies had more than twice the rates found for men in traditional families before the birth (χ2=64.89, df=3, p<0.001, Pearson chi-square) and after the birth (χ2=21.00, df=3, p<0.01, Pearson chi-square).
Men's depressive symptoms were correlated with their partners' depressive symptoms before the birth (r=0.24, df=6223, p<0.001) and following the birth (r=0.26, df=6605, p<0.001). Including maternal depressive symptoms in the linear regression models predicting men's depressive symptoms (both before and after the birth) did not affect the significance of the family type effect. However, there was a significant interaction between maternal depression and type of family before the birth (F=3.14, df=3,6166, p<0.05) and following the birth (F=3.06, df=3,6548, p<0.01). The correlations between mothers' and partners' depressive symptoms in the stepfather families before the birth (r=0.33, df=351, p<0.001) and after the birth (r=0.39, df=377, p<0.001) were higher than for the men in other family types before the birth (traditional families, r=0.23, df=5592, p<0.001; stepmother families, r=–0.02, df=36, n.s.; single-mother families, r=0.26, df=192, p<0.001) and following the birth (traditional families, r=0.25, df=5929, p<0.001; stepmother families, r=0.35, df=40, p<0.05; single-mother families, r=0.22, df=207, p<0.01).
To test whether the effect of family type could be accounted for by other factors, further covariates were added to the regression model predicting depressive symptoms following the birth. Prior to this, we estimated the univariate associations between the covariates (F tests and correlations) and postnatal depressive symptoms. Higher levels of depressive symptoms following the birth were associated with lower educational qualifications (F=4.17, df=3,6522, p<0.01), living in rented housing (F=25.92, df=2,6640, p<0.001) and low-income housing and apartments (F=8.48, df=4,6623, p<0.001), more crowding (F=39.12, df=1,6579, p<0.001), older age (r=0.03, df=6789, p<0.05), unemployment (F=55.97, df=1,6893, p<0.001), less social support (r=–0.22, df=6791, p<0.001), smaller social networks (r=–0.13, df=6845, p<0.001), lower partnership affection (r=0.19, df=5896, p<0.001), higher partnership aggression (r=–0.20, df=5944, p<0.001), more stressful life events (r=0.28, df=6415, p<0.001), and more frequent changes in romantic relationships (F=7.03, df=2,5354, p<0.001).
The final model included only those covariates which were significant in the full regression equation: a categorical measure of educational qualifications (none, some high school, high school diploma, and college degree), age, weighted life events, social support and social network, and aggression and lack of affection in the partnership. The parameter estimates and standard errors for this model are shown in table 2.
When the selected covariates were included in the final model, family type was no longer a significant predictor of depression following the child's birth. A higher depression score was related to being older, having less education, experiencing more stressful life events, receiving less social support, having smaller social networks, and having more aggressive and less affectionate partner relationships.
The selected covariates in the final model explained the variance that was due to stepfather status. To indicate which of these selected covariates were potential mediators between stepfather status and depression, the difference in means of the selected continuous measures for the traditional and stepfather families was tested by using an unpaired t test. For the selected categorical measures, the difference in rates between the two family types was tested by using a Pearson chi-square test.
The measures that were associated with stepfather status and, therefore, were statistical mediators between stepfather status and depressive symptoms included educational qualifications (χ2=54.50, df=3, p<0.01), number of life events (t=7.79, df=6042, p<0.01), social support (t=–6.37, df=6435, p<0.01), social network (t=–8.05, df=6486, p<0.01), and aggression (t=2.31, df=5768, p=0.02). The men in traditional families had more education (21% with no qualifications and 24% with college degrees), fewer life events (mean=8.4, SD=7.5), higher social support (mean=18.1, SD=4.7), larger social networks (mean=22.5, SD=3.9), and less aggression in their partnerships (mean=10.0, SD=1.8) than men in stepfather families, who had less education (36% with no qualifications and 11% with college degrees), more life events (mean=11.7, SD=9.3), less social support (mean=16.5, SD=5.2), smaller social networks (mean=20.9, SD=4.6), and more aggression in the partnership (mean=9.7, SD=2.0). Age and lack of affection toward the partner were unrelated to stepfather status, which rules out their roles as statistical mediators of the effect of stepfather status on depressive symptoms.
DISCUSSION
Our first aim in this study was to examine the role of family structure in defining groups of men at risk for depression in a large community sample. Men in stepfamilies and partners of single mothers had higher levels of depressive symptoms than men in traditional families. Based on categorical depression scores (greater than 12 on the Edinburgh Postnatal Depression Scale), the rates of depression 8 weeks after the birth of a child among men in stepfamilies and single-mother families were similar to the 6-week-postpartum rate reported by Ballard and Davies (28).
We also found that the relation between depressive symptoms and family status was entirely mediated by six risk factors. Stepfathers' higher levels of depressive symptoms were associated with higher rates of depression among their partners, less education, more life events, less social support, smaller social networks, and more aggression within their partnerships. These correlates are consistent with those reported in the literature for women (20) and their male partners (28). Because these data are correlational and the mediators are self-reported, these links cannot be considered causal, and shared method variance could account for some of the overlapping variance.
Four issues are raised by these findings. First, level of women's depressive symptoms was the strongest correlate of men's depressive symptoms. Although we cannot draw causal inferences from these correlational data, a number of different processes might be implicated here. It could be that each partner's psychosocial state directly influences the other's—that living with a depressed person has a depressing effect. It could also be that common causal factors outside the family, such as social stresses, contribute to the depressive symptoms of both men and their partners. Interestingly, the covariates considered in this study did not mediate the relation between the partners' depressive symptoms. Maternal depressive symptoms remained a highly significant predictor of men's depressive symptoms even after the selected covariates (age, education, life events, social support, social network, and affection and aggression within the partnership) had been included in the statistical model. It could also be that men and women who are vulnerable to depression are more likely to form relationships. Whatever the causal patterns, it is clear that beyond the usual social risks for depression, having a depressed partner is an important risk as well.
A second point is that, overall, men's depressive symptoms did not increase following the birth of a child, a finding that has been shown in some of the other studies of selected samples of men (28). The constellation of events surrounding the birth did not constitute an added risk for the vast majority of these men. It should be emphasized that even in the stepfather families, the child being born was in the very great majority of cases the child of this father. It was his relationships with the older children in the household that were step-relationships.
The third issue concerns the role of socioeconomic circumstances in the etiology of depression. Consistent with findings in other studies (20, 28, 33), there were associations between socioeconomic factors and depressive symptoms in this study. However, most of the sociodemographic covariates (housing indicators and unemployment) were no longer significant once all of the variables had been considered in a single regression model. Thus, socioeconomic differences between stepfather and traditional families (the former had more disadvantaged circumstances) were not responsible for the higher level of depressive symptoms among stepfathers.
Finally, we add a note of caution. We have stressed that the correlational nature of the data precludes inferences on causal mechanisms. To that caution we should add that one cost of having depression data on such a large sample is that we do not have precise diagnostic information. We lack data on psychiatric history, and we did not have a comparison group of partners of nonpregnant women. Thus, these findings may not generalize to studies that have employed more precise measures of depression in men. In spite of these shortcomings, the findings draw attention to an important set of facts—men in stepfamilies may be at greater risk for depression than those in traditional families, and this risk is closely linked to their partners' depressive symptoms. The risk for children growing up in a family with two depressed parents is not trivial; rather, it deserves further research attention.
 |
 |
Received July 21, 1997; revisions received Oct. 20 and Dec. 15, 1997; accepted Jan. 15, 1998. From the Social, Genetic, and Developmental Psychiatry Research Centre, Institute of Psychiatry, London, and the Paediatric and Perinatal Epidemiology Unit, University of Bristol, U.K. Address correspondence to Dr. Deater-Deckard, Institute of Psychiatry, 111 Denmark Hill, London SE5 8AF, UK. Supported in part by the Medical Research Council, Wellcome Trust, Departments of Health and Environment, British Gas, and other companies. The Avon Longitudinal Study of Pregnancy and Childhood is part of the European Longitudinal Study of Pregnancy and Childhood initiated by the World Health Organization. The Avon Longitudinal Study of Pregnancy and Childhood Study Team comprises interviewers, technicians, clerical workers, research scientists, volunteers, and managers who continue to make the study possible. The authors thank the mothers who participated in the study and the midwives for their cooperation and help in recruitment.
1 Bruce ML, Kim KM: Differences in the effects of divorce on major depression in men and women. Am J Psychiatry 1992; 149:914–917Link, Google Scholar
2 Hetherington EM, Clingempeel WG: Coping With Marital Transitions: A Family Systems Perspective. Monographs of the Society for Research in Child Development (Serial 227) 1992; 57(2–3):1–242Google Scholar
3 Merikangas KR: Divorce and assortative mating among depressed patients. Am J Psychiatry 1984; 141:74–76Link, Google Scholar
4 Aseltine RH, Kessler RC: Marital disruption and depression in a community sample. J Health Soc Behav 1993; 34:237–251Crossref, Medline, Google Scholar
5 Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C: Affective disorders, in Psychiatric Disorders in America: The Epidemi~ologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 55–80Google Scholar
6 O'Connor TG, Hawkins N, Dunn J, Thorpe KJ, Golding J: Family type and maternal depression in pregnancy: factors mediating risk in a community sample. J Marriage and the Family (in press)Google Scholar
7 Anthony JC, Petronis KR: Suspected risk factors for depression among adults 18–44 years old. Epidemiology 1991; 2:123–132Crossref, Medline, Google Scholar
8 Coryell W, Endicott J, Keller MB: Major depression in a nonclinical sample: demographic and clinical risk factors for first onset. Arch Gen Psychiatry 1992; 49:117–125Crossref, Medline, Google Scholar
9 Weissman MM, Klerman GL: Sex differences and the epidemiology of depression. Arch Gen Psychiatry 1977; 34:98–111Crossref, Medline, Google Scholar
10 Hay D, Kumar R: Interpreting the effects of mothers' postnatal depression on children's intelligence: a critique and re-analysis. Child Psychiatry Hum Dev 1995; 25:165–181Crossref, Medline, Google Scholar
11 Murray L: The impact of postnatal depression on infant development. J Child Psychol Psychiatry 1992; 33:543–561Crossref, Medline, Google Scholar
12 Sharp D, Hay D, Pawlby S, Schmucker G, Allen H, Kumar R: The impact of postnatal depression on boys' intellectual development. J Child Psychol Psychiatry 1995; 36:1315–1336Crossref, Medline, Google Scholar
13 Hammen C, Burge D, Burney E, Adrian C: Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Arch Gen Psychiatry 1990; 47:1112–1117Crossref, Medline, Google Scholar
14 Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, Eaves LJ: Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiatry 1995; 152:833–842Link, Google Scholar
15 Beck CT: The effects of postpartum depression on maternal-infant interaction: a meta-analysis. Nurs Res 1995; 44:298–304Crossref, Medline, Google Scholar
16 Campbell SB, Cohn JF, Meyers T: Depression in first-time mothers: mother-infant interaction and depression chronicity. Dev Psychol 1995; 31:349–357Crossref, Google Scholar
17 Downey G, Coyne JC: Children of depressed parents: an integrative review. Psychol Bull 1990; 108:50–76Crossref, Medline, Google Scholar
18 Zaslow MJ, Pedersen FA, Cain RL, Suwalsky JT, Kramer EL: Depressed mood in new fathers: associations with parent-infant interaction. Genet Soc Gen Psychol Monogr 1985; 111:133–150Medline, Google Scholar
19 Goodman SH, Brogan D, Lynch ME, Fielding B: Social and emotional competence in children of depressed mothers. Child Dev 1993; 64:516–531Crossref, Medline, Google Scholar
20 O'Hara MW, Swain AM: Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 1996; 8:37–54Crossref, Google Scholar
21 Kumar R: Postnatal mental illness: a transcultural perspective. Soc Psychiatry Psychiatr Epidemiol 1994; 29:250–264Crossref, Medline, Google Scholar
22 Fergusson DM, Horwood LJ, Thorpe K, the ALSPAC Study Team: Changes in depression during and following pregnancy. Paediatr Perinat Epidemiol 1996; 10:279–293Crossref, Medline, Google Scholar
23 Ferketich SL, Mercer RT: Predictors of role competence for experienced and inexperienced fathers. Nurs Res 1995; 44:89–95Medline, Google Scholar
24 Deater-Deckard K: Parenting stress and child adjustment: some old hypotheses and new questions. Clin Psychol Science and Practice (in press)Google Scholar
25 O'Hara MW: Depression and marital adjustment during pregnancy and after delivery. Am J Family Therapy 1985; 13:49–55Crossref, Google Scholar
26 Sheppard M: Postnatal depression, child care and social support: a review of findings and their implications for practice. Soc Work and Soc Sciences Rev 1994; 5:24–46Google Scholar
27 Webster ML, Thompson JMD, Mitchell EA, Werry JS: Postnatal depression in a community cohort. Aust NZ J Psychiatry 1994; 28:42–49Crossref, Medline, Google Scholar
28 Ballard C, Davies R: Postnatal depression in fathers. Int Rev Psychiatry 1996; 8:65–71Crossref, Google Scholar
29 Lovestone S, Kumar R: Postnatal psychiatric illness: the impact on partners. Br J Psychiatry 1993; 163:210–216Crossref, Medline, Google Scholar
30 Zelkowitz P, Milet TH: Postpartum psychiatric disorders: their relationship to psychological adjustment and marital satisfaction. J Abnorm Psychol 1996; 105:281–285Crossref, Medline, Google Scholar
31 Brown GW, Harris T, Hepworth C: Life events and endogenous depression: a puzzle reexamined. Arch Gen Psychiatry 1994; 51:525–534Crossref, Medline, Google Scholar
32 Skodol AE, Schwartz S, Dohrenwend BP, Levav I, Shrout PE: Minor depression in a cohort of young adults in Israel. Arch Gen Psychiatry 1994; 51:542–551Crossref, Medline, Google Scholar
33 Murphy JM, Olivier DC, Monson RR, Sobol AM, Federman EB, Leighton AH: Depression and anxiety in relation to social status: a prospective epidemiological study. Arch Gen Psychiatry 1991; 48:223–229Crossref, Medline, Google Scholar
34 Golding J: Children of the nineties: a resource for assessing the magnitude of long-term effects of prenatal, perinatal and subsequent events. Contemporary Reviews in Obstetrics and Gynaecology 1996; 8:89–92Google Scholar
35 Cox JL, Holden JM, Sagovsky R: Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150:782–786Crossref, Medline, Google Scholar
36 Harris B, Huckle P, Thomas R, Johns S, Fung H: The use of rating scales to identify post-natal depression. Br J Psychiatry 1989; 154:813–817Crossref, Medline, Google Scholar
37 Murray L, Carothers A: The validation of the Edinburgh Post-Natal Depression Scale on a community sample. Br J Psychiatry 1990; 157:288–290Crossref, Medline, Google Scholar
38 Brown GW, Harris T: Social Origins of Depression: A Study of Psychiatric Disorder in Women. London, Tavistock Press, 1978Google Scholar
39 Barnett B, Hanna EW, Parker G: Life events for obstetric groups. J Psychosom Res 1983; 27:313–320Crossref, Medline, Google Scholar



