Aborted Suicide Attempts: A New Classification of Suicidal Behavior
Abstract
OBJECTIVE: With the goal of ultimately finding early suicide predictors, the authors undertook a study of aborted suicide attempts. They defined such an attempt as an event in which an individual comes close to attempting suicide but does not complete the act and thus sustains no injury. METHOD: The authors interviewed a random sample of 135 adult psychiatric inpatients concerning their past suicidal behavior. Using standardized scales, they assessed suicidal intent for aborted suicide attempts and actual suicide attempts, as well as degree of injury for actual attempts. RESULTS: Over half of the 135 subjects reported making at least one aborted suicide attempt. Aside from younger age, no demographic characteristics were associated with aborted attempts. Aborted attempts were reported more often in subjects with a diagnosis of borderline personality disorder than in subjects with other diagnoses. Intent scores for aborted attempts were comparable to those for actual suicide attempts. Subjects who had made an aborted attempt were nearly twice as likely to have made an actual suicide attempt as subjects with no aborted attempts. Among subjects with both aborted and actual attempts, the first aborted attempt preceded the first actual attempt approximately half the time. CONCLUSIONS: Aborted suicide attempts were reported commonly by psychiatric inpatients, had a similar level of intent as actual attempts, and were highly associated with actual attempts. Thus, clinicians should specifically ask patients about aborted attempts as a part of the suicide history. Further study is needed to examine the association between aborted suicide attempts and suicide.
Suicide is a significant public health problem in the United States, accounting for approximately 30,000 deaths annually (1). It does not usually occur without warning. The person who ultimately commits suicide has often attempted to communicate his or her suicidal thoughts to a friend, family member, or physician (2–4). Other activities preceding a suicide typically include preparations for death such as writing a will or a suicide note (4, 5).
Along with these presuicidal behaviors, suicide attempts themselves are an important risk factor for suicide. Because suicide represents 1% of all deaths in the United States (1), and an estimated 10% of those who attempt suicide eventually die by suicide (6–9), the risk of suicide among those with a history of suicide attempts is substantially elevated. One study found that the risk of a subsequent suicide attempt increases by about 32% for each prior attempt (10), and, by extension, it is likely that the risk of suicide would increase as well. However, the majority of people who commit suicide do so on their first attempt—75% of one sample of suicide victims studied (11). Therefore, it would be useful to identify other preparatory suicidal behaviors in order to improve suicide prevention.
In an earlier pilot study, we proposed a new category of such behaviors that we called “aborted suicide attempts” (12). The aborted suicide attempt refers to an event in which an individual is one step away from attempting suicide but does not complete the act and thus incurs no physical injury. The essential characteristics of an aborted attempt are 1) intent to kill oneself, 2) a change of mind immediately before the actual attempt, and 3) absence of injury. An example would be a person who went to a bridge and leaned over the side, thinking of jumping to her death, but then changed her mind and left the site. Another example would be the person who held a gun to his head with the intent to fatally shoot himself, then changed his mind and put the gun down.
In the range from suicidal ideation to suicide attempt to suicide, defining aborted attempts adds a new category falling between ideation and attempts. Clinicians do not routinely ask about this type of behavior, and, consequently, the suicidality of patients with aborted attempts may remain hidden.
In our pilot study, the prevalence of aborted attempts among psychiatric inpatients was estimated to be approximately 25%. In that study, however, age was restricted to less than 55 years old, and the definition of aborted attempts was not specifically operationalized to each method of injury. That study also did not explore the relationship between aborted attempts and actual suicide attempts. Therefore, we undertook a more extensive study of aborted suicide attempts in a random sample of inpatients in order to determine their frequency and the degree of suicide intent associated with them. We also sought to determine whether aborted attempts might be predictive of subsequent suicidal behavior.
We hypothesized that aborted attempts are common among inpatients, that they are associated with high suicidal intent, and that they predict future actual attempts. If aborted attempts were predictive of future suicidal behavior, they would be extremely useful to the clinician in identifying high-risk individuals before they incur an injury.
METHOD
Subjects
The study was conducted on the inpatient wards of the Payne Whitney Clinic, which is the psychiatric division of a university medical center in Manhattan. Its 64 beds include specialized units for geriatric and adolescent patients as well as for those with psychoses, mood disorders, or substance abuse. Payne Whitney admits approximately 5% of its patients involuntarily.
To be included in the study, subjects had to be at least 18 years old, English speaking, and able to consent to and complete an interview about suicidal behavior. Patients were excluded if they had severe dementia, mental retardation, profound psychosis, or severe agitation or if they did not speak English. Each patient provided written informed consent before being interviewed for the study. The study was approved by the Institutional Review Board of The New York Hospital.
Study subjects were randomly selected on a weekly basis from all consecutive inpatient admissions, through use of a computer-generated random number list. During the study period from August 1995 through March 1996, there were 416 admissions, from which we ultimately enrolled 135 subjects (32.5% of admissions). Of these 416 patients, 45 were approached by the investigator but declined to be interviewed. Thirty-two patients were not appropriate for the study because of exclusion criteria mentioned earlier. Fifty-eight patients were discharged from the hospital before they could be approached and invited to participate, and 146 were not approached because they were too low on the randomization list.
Assessments
One physician (M.E.B.) administered a structured interview to each subject. Subjects were questioned about demographics, dates and circumstances regarding past aborted and actual suicide attempts, degree of self-destructive intent, and seriousness of injuries sustained from actual attempts. The interview took an average of 30 minutes to complete.
A lifetime history of aborted suicide attempts was taken by using a questionnaire that we devised (the Aborted Attempts Inventory). In this 18-item inventory, patients were first asked a general question about whether they had come close to making a suicide attempt but then changed their mind and stopped. Regardless of a patient's response to that question, we specifically probed for aborted attempts for each of 17 common suicide methods. The following are examples of questions used to elicit a history of aborted suicide attempts.
9.1. Did you ever come close to trying to kill yourself by holding a gun, thinking of shooting yourself?
IF YES:
9.2. Was the gun loaded?
9.3. Did you hold the gun to your head or chest?
9.4. When? (Date)
12.1. Did you ever come close to trying to kill yourself by going to a bridge or rooftop, thinking of jumping off?
IF YES:
Which/where?
12.2. Did you lean over the roof or bridge?
12.3. When?
In designing the study, we sought this degree of detail because aborted suicide attempts had not yet been operationally defined for each suicide method, and we needed to be sure that the patient understood what information was being requested. In addition, without specific prompting by the interviewer, the patient might have forgotten or neglected to mention an incident that caused no injury.
Passing suicidal thoughts that occurred while the subject happened to be in close proximity to a lethal method of injury were not counted as aborted attempts, since they lack the necessary suicidal intent. An example would be the woman who thought “I wonder if I could cut my wrist?” while using a knife to cut vegetables. Suicide attempts that were stopped by another person before completion were counted not as aborted attempts but as actual suicide attempts, since these events lack the “change of mind” by the attempter. An example would be the man who was pulled back from an open window by his mother. A person who completed the use of a potentially lethal method was considered to have made an actual suicide attempt, even if no injury resulted. An example would be a woman who swallowed medications with the intent to die but incurred no physical effects.
For each occurrence of an aborted suicide attempt detected in the inventory, we administered the Beck Suicidal Intent Scale (13). This scale contains 15 items that evaluate the severity of a patient's psychological intent at the time of a suicide attempt, using questions about the objective (e.g., precautions against discovery) and subjective (e.g., desire to die) aspects of the attempt. The Beck Suicidal Intent Scale has been validated as a measure of the seriousness of intent of a suicide attempt (14).
Following the questions concerning aborted suicide attempts, each patient was asked about actual suicide attempts. An actual attempt is an event in which an individual engages in any self-destructive behavior with the intent to die. For each actual suicide attempt in a patient's history, the Beck Suicidal Intent Scale and the Lethality Scale (A.T. Beck, unpublished) were completed. The Lethality Scale measures the seriousness of physical injuries incurred by the patient for a particular method used during the suicide attempt. The scale, which has a range from 0 (no injury) to 8 (death), has clearly defined criteria for each value.
Methods with a potential for low and high lethality were defined a priori for both aborted and actual attempts. Methods with high potential lethality include shooting, jumping from a height, hanging or strangulation, drowning, jumping in front of a train or traffic, car exhaust gas, electrocution, immolation, and driving recklessly (the last two apply only to actual attempts). Methods with low potential lethality include cutting, overdose, and house gas.
Primary axis I and primary axis II diagnoses were obtained from the medical records after the patient was discharged from the hospital.
Statistical Analyses
Patient groups were compared on categorical variables through use of chi-square tests and on continuous variables with t tests. Some subjects had a history of multiple aborted and actual attempts. Thus, when we compared intent scores for methods of aborted or actual attempts with low and high potential lethality, subjects were classified into one of two groups for the purpose of statistical comparison. These groups consisted of those with methods of aborted or actual attempts with both high and low potential lethality and those with either type of method but not both. Similarly, when we compared intent scores for aborted and actual attempts themselves, subjects were separated into those with both aborted and actual attempts and those with either event but not both. Then, the appropriate t test, either paired or unpaired, was performed. A two-tailed alpha level of 0.05 was used for statistical significance for all tests.
RESULTS
Demographic and Diagnostic Characteristics
The 135 study participants were compared to the 45 available patients who met study inclusion criteria but declined the interview. Sixty-nine participants (51.1%) were female, compared to 25 nonparticipants (55.6%) (χ2=0.27, df=1, p=0.61). Among participants, 75 (55.6%) were white, 27 (20.0%) were black, 25 (18.5%) were Hispanic, and eight (5.9%) were Asian or of other race/ethnicity. For nonparticipants, 29 (64.4%) were white, 11 (24.4%) were black, four (8.9%) were Hispanic, and one (2.2%) was Asian (χ2=3.94, df=4, p=0.41). Participants (mean age=38.3 years, SD=13.5) were significantly younger than nonparticipants (mean age=45.2 years, SD=15.9) (t=2.63, df=66.3, p=0.01). Eighty-one study subjects (60.0%) were single, 22 (16.3%) were married or cohabitating, and 32 (23.7%) were divorced, separated, or widowed. Data on marital status were not available for nonparticipants.
According to the medical records, of the 135 subjects, 54 (40.0%) had a current diagnosis of unipolar depression, 37 (27.4%) had schizophrenia or related psychotic disorders, 20 (14.8%) had bipolar illness, 18 (13.3%) had substance-related disorders, and six (4.4%) had some other axis I diagnosis (adjustment disorders, somatization disorder, and posttraumatic stress disorder) as their primary axis I diagnosis. On axis II, 106 subjects (78.5%) had no diagnosis, 18 (13.3%) had borderline personality disorder, and 11 (8.2%) had another axis II disorder (other personality disorders, learning disabilities).
Aborted Attempts
In our group of 135 subjects, 71 (52.6%) had a lifetime history of at least one aborted suicide attempt. Thirty-three (24.4%) had one aborted attempt only, while 38 (28.1%) had multiple aborted attempts, to a maximum of 12 aborted suicide attempts in one case. Thus, approximately half of the subjects who had aborted attempts had one only, while the other half had more than one.
Subjects with aborted attempts (mean age=35.5 years, SD=12.0) were significantly younger than subjects with no aborted attempts (mean age=41.4 years, SD=14.4) (t=2.57, df=123, p=0.01). There were no significant differences in gender (χ2=3.2, df=1, p=0.07), race (χ2=3.9, df=4, p=0.42), or marital status (χ2=5.6, df=5, p=0.35) between subjects with and without histories of aborted attempts.
Sixteen (88.9%) of 18 subjects with borderline personality disorder reported histories of aborted attempts. This was a high frequency of aborted attempts compared to six (54.5%) of 11 subjects with other personality disorders or learning disabilities and 49 (46.2%) of 106 subjects with no axis II diagnosis (χ2=11.3, df=2, p=0.004). Five (25%) of 20 subjects with bipolar disorder reported aborted attempts. This was a lower frequency of such attempts than for subjects with depression (32 of 54 subjects, 59.3%), schizophre~nia (18 of 37 subjects, 48.6%), or other axis I diagnoses (five of six subjects, 83.3%) (χ2=10.1, df=4, p=0.04).
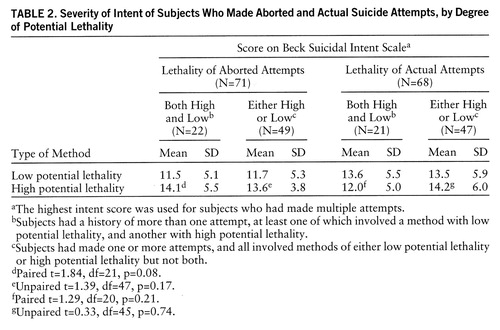
The most common methods chosen for aborted attempts were jumping from a height, overdose, and cutting (table 1). Intent scores for aborted attempts were marginally higher for attempts using more potentially lethal methods (table 2).
Actual Attempts
Sixty-eight subjects (50.4%) had a lifetime history of at least one actual suicide attempt. Twenty-nine (21.5%) had one actual attempt only, while 39 (28.9%) had multiple actual attempts, up to a maximum of eight actual suicide attempts. Thus, approximately half of the subjects with histories of actual attempts had made one only, while the other half had made multiple attempts.
There was no significant association between gender (χ2=0.00, df=1, p=1.00), race (χ2=5.8, df=4, p=0.21), age (t=1.89, df=115.0, p=0.06), or marital status (χ2=10.6, df=5, p=0.06) and actual attempts. There was also no significant association between actual attempts and psychiatric diagnosis (for axis I, χ2=6.8, df=4, p=0.15; for axis II, χ2=4.2, df=2, p=0.12). Overdose and cutting were the most common methods used in actual attempts (table 1). For actual attempts, there were no significant differences in intent scores for methods with high versus low potential lethality (table 2).
Aborted Attempts and Actual Attempts
There were nearly twice as many actual suicide attempts among subjects with aborted attempts as among those without aborted attempts. Of the 71 subjects with aborted attempts, 64.8% also had histories of actual attempts, while 34.4% of 64 subjects with no aborted attempts had made actual attempts (χ2=11.3, df=1, p<0.001).
Intent scores for aborted attempts and actual attempts were compared. For subjects with multiple aborted attempts, the highest overall intent score was used; the same was done for subjects with multiple actual attempts. In general, the mean intent scores of actual attempts and aborted attempts were similar. For subjects with both aborted and actual attempts, the mean intent score for aborted attempts was 14.6 (SD=4.5), while the mean intent score for actual attempts was 15.0 (SD=5.5) (paired t=0.48, df=45, p=0.63). For subjects with either aborted or actual attempts (but not both), the mean intent score for aborted attempts was 11.3 (SD=5.1), while the mean intent score for actual attempts was 12.1 (SD=5.5) (unpaired t=0.55, df=45, p=0.59).
Among subjects who had histories of both aborted and actual attempts (N=46), the first aborted attempt preceded the first actual attempt in 22 cases (47.8%), while the first aborted attempt followed the first actual attempt in 23 cases (50.0%). For one subject, it was not known whether the aborted attempt had preceded or followed the actual attempt.
DISCUSSION
Our study indicates that aborted attempts were quite common among this sample of psychiatric inpatients. Over half of the cohort had at least one aborted attempt. In fact, as many subjects reported aborted attempts as reported actual attempts. Aborted attempts were not associated with gender, race, or marital status; rather, they were equally common across demographic strata. Aborted attempts were also found in all diagnostic groups. Even more striking, aborted suicide attempts were strongly associated with actual suicide attempts. Subjects who had made an aborted attempt were nearly twice as likely to have a history of actual attempts as those who had never made an aborted attempt.
The finding of higher rates of aborted attempts in subjects with a diagnosis of borderline personality disorder is not surprising, since borderline personality disorder has been found to be associated with both suicide attempts (15) and suicide (16–18). It is unclear why lower rates of aborted attempts were found in subjects with bipolar disorder; this may reflect a particular characteristic of the bipolar inpatients we interviewed.
The most common method of aborted attempt was one of high potential lethality, jumping from a height. In contrast, overdose, a low-lethality method, was the most common method of actual attempt for our study group. Clearly, jumping would not be likely to be the most common method of actual attempt for our sample of live subjects precisely because of its potential lethality—few patients would have survived such an attempt. The use of methods of high potential lethality by persons in aborted attempts is alarming, since an actual attempt by the same method will likely result in death. It is unknown whether these subjects might ultimately complete a suicide attempt by using the same method as in their aborted attempts.
Average intent scores for both low- and high-potential lethality methods of aborted attempts were in the 12–14 range of the 0–30-point suicide intent scale and were not significantly different from each other. Intent scores for aborted attempts showed no significant difference from intent scores for actual attempts. A history of suicide attempts with intent scores of 11 or greater has been found to be associated with subsequent suicide in one follow-up study (19).
For subjects with both aborted and actual attempts, the aborted attempt was equally likely to occur after the actual attempt as to occur before, so we cannot conclude that aborted attempts predict subsequent actual attempts from the temporal sequence found. Nonetheless, we cannot discount aborted attempts as a possible risk factor in the subgroup of patients for whom the aborted attempt did precede the actual attempt. We have no information on the relationship between aborted suicide and the risk of suicide completion, an intriguing question that requires further study.
This study has several limitations. First, the subjects were psychiatric inpatients and are not a representative sample of either outpatients or the general population. Second, data were gathered through the subject's retrospective self-report and may involve recall bias. The possibility of poor subject recall was minimized by using a semistructured interview, which has been shown to be more accurate than clinician assessment in ascertaining history of suicide attempts in inpatients (20). Further studies of outpatient or nonpatient populations, as well as prospective studies of patients reporting aborted and actual suicide attempts, could examine the generalizability of our results and minimize recall bias. However, prospective studies of aborted attempts will not be possible until clinicians routinely gather such information from their patients.
From the vantage of predicting suicide risk, we note that in our sample of 135 subjects, half (N=68) had already made an actual suicide attempt and would have already been identified by clinicians as being at high risk for future suicide. Another third of the subjects (N=42) had no aborted attempts or actual attempts and would be considered at a relatively lower risk for future suicide. The remaining subjects (N=25) had made aborted attempts but had not made any actual attempts. Clinicians might not consider these patients to be at high risk for future suicide, although, on the basis of our data, they probably should. The clinician can, at the very least, consider patients with aborted attempts to be at a high likelihood of ending up in the group of patients with actual attempts, risking the morbidity associated with those attempts. Because previous studies have shown that people who make suicide attempts are at greater risk for future suicide, we can predict by extension that our group of subjects with aborted attempts only will also be at greater risk of future suicide. This group of at-risk patients will remain hidden to the clinician who does not inquire about aborted attempts.
We recommend that clinicians begin asking patients routinely and specifically about aborted suicide attempts, as another component of the suicide history. Further study is needed to determine the association between aborted suicide attempts and suicide.
 |
 |
Received Oct. 15, 1996; revision received Aug. 6, 1997; accepted Oct. 3, 1997. From the Payne Whitney Clinic, The New York Hospital, and the Department of Psychiatry, Cornell University Medical College, New York. Address reprint requests to Dr. Barber, Middletown Mental Health Clinic, 141 Monhagen Ave., Bldg. 54, Middletown, NY 10940; [email protected] (e-mail).
1. Kochanek KD, Hudson BL: Advance Report of Final Mortality Statistics, 1992: Monthly Vital Statistics Report, vol 43, number 6, Supplement. Hyattsville, Md, National Center for Health Statistics, 1995Google Scholar
2. Barraclough B, Bunch J, Nelson B, Sainsbury P: A hundred cases of suicide: clinical aspects. Br J Psychiatry 1974; 125:355–373Crossref, Medline, Google Scholar
3. Hawton K, Blackstock E: General practice aspects of self-poisoning and self-injury. Psychol Med 1976; 6:571–575Crossref, Medline, Google Scholar
4. Beck AT, Lester D: Components of suicidal intent in completed and attempted suicides. J Psychol 1976; 92:35–38Crossref, Medline, Google Scholar
5. Tuckman J, Youngman WF: A scale for assessing suicide risk of attempted suicides. J Clin Psychol 1968; 24:17–19Crossref, Medline, Google Scholar
6. Pokorny AD: A follow-up study of 618 suicidal patients. Am J Psychiatry 1966; 122:1109–1116Google Scholar
7. Ettlinger R: Evaluation of suicide prevention after attempted suicide. Acta Psychiatr Scand Suppl 1975; 260:1–135Medline, Google Scholar
8. Avery D, Winokur G: Suicide, attempted suicide, and relapse rates in depression: occurrence after ECT and antidepressant therapy. Arch Gen Psychiatry 1978; 35:749–753Crossref, Medline, Google Scholar
9. Fowler RC, Tsuang MT, Kronfol Z: Communication of suicidal intent and suicide in unipolar depression: a forty year follow-up. J Affect Disord 1979; 1:219–225Crossref, Medline, Google Scholar
10. Leon AC, Friedman RA, Sweeney JA, Brown RP, Mann JJ: Statistical issues in the identification of risk factors for suicidal behavior: the application of survival analysis. Psychiatry Res 1990; 31:99–108Crossref, Medline, Google Scholar
11. Maris RW: Pathways to Suicide: A Survey of Self-Destructive Behavior. Baltimore, Johns Hopkins University Press, 1981Google Scholar
12. Marzuk PM, Tardiff K, Leon AC, Portera L, Weiner C: The prevalence of aborted suicide attempts among psychiatric inpatients. Acta Psychiatr Scand 1997; 96:492–496Crossref, Medline, Google Scholar
13. Beck AT, Schuyler D, Herman I: Development of suicidal intent scales, in The Prediction of Suicide. Edited by Beck AT, Resnick HLP, Lettieri DJ. Bowie, Md, Charles Press, 1974, pp 45–56Google Scholar
14. Beck RW, Morris JB, Beck AT: Cross-validation of the suicide intent scale. Psychol Rep 1974; 34:445–446Crossref, Medline, Google Scholar
15. Friedman RC, Aronoff MS, Clarkin JF, Corn R, Hurt SW: History of suicidal behavior in depressed borderline inpatients. Am J Psychiatry 1983; 140:1023–1026Google Scholar
16. Pope HG Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG: The validity of DSM-III borderline personality disorder: a phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry 1983; 40:23–30Crossref, Medline, Google Scholar
17. Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kashgarian M, Bolinger JM: Borderline: an adjective in search of a noun. J Clin Psychiatry 1985; 46:41–48Medline, Google Scholar
18. Paris J, Brown R, Nowlis D: Long term follow-up of borderline patients in a general hospital. Compr Psychiatry 1988; 29:147–150Crossref, Medline, Google Scholar
19. Pierce DW: The predictive validation of a suicide intent scale: a five year follow-up. Br J Psychiatry 1981; 139:391–396Crossref, Medline, Google Scholar
20. Malone KM, Szanto K, Corbitt EM, Mann JJ: Clinical assessment versus research methods in the assessment of suicidal behavior. Am J Psychiatry 1995; 152:1601–1607Google Scholar



