Predictors of Major Depression Six Months After Admission for Outpatient Treatment
Unremitting depression is a prevalent and insidious public health problem ( 1 , 2 ) for which an effective approach has not been identified. Recent data from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrate that algorithms using augmentation or switching medications to treat resistant depression have limited efficacy ( 3 , 4 ). This study assessed predictors of sustained major depression among adults receiving care in community outpatient settings. This study expanded on earlier research documenting the predictors of early recovery ( 5 ) to identify adults who are at risk of sustained depression at six months, after early pharmacotherapy and baseline predictors of course of depressive illness have been accounted for during the three months after admission to a mental health clinic.
More than two decades ago, Keller and colleagues ( 6 ) reported that 45% of patients admitted to academic centers for treatment of an index episode of depression continued to meet criteria for major depression six months later. Less is known about the course of depression in community-based psychiatric settings. In this study we examined the rates of persistent major depression six months after treatment had been sought at community clinics. Since Keller and colleagues' study of 1986, better-tolerated antidepressants have been developed and implemented in the field.
In an earlier study, we identified predictors of early (three-month) "recovery" from depression, which was defined as two weeks with no or only minimal symptoms of depression ( 5 ). Early recovery was independently associated with less severe depression, adequate antidepressant treatment, being female, and being married. Building on this previous work, we hypothesized that sustained major depression at six months after admission would be predicted by lack of achievement of early recovery and by depression severity at admission, duration of the index episode, and intensity of early pharmacotherapy between baseline and six months.
Methods
Outpatient mental health clinics were selected from Westchester County, New York, to maximize socioeconomic and ethnic diversity. Six clinics (an outpatient department of a teaching hospital, a voluntary-sector hospital-based clinic, three county-funded clinics, and a freestanding voluntary-sector clinic) were selected to participate in a study of the course and outcome of major depressive disorder.
Individuals 18 years and older who were admitted consecutively to participating clinics during between October 1, 1995, and December 31, 1997, were invited to participate in a two-stage screening process in the same period to identify new admissions with major depressive disorder as defined by DSM-IV. Individuals who screened positive for depression on the Center for Epidemiological Studies Depression Scale were reinterviewed with the Structured Clinical Interview for DSM-IV to establish the major depression diagnosis. Antidepressants of the selective serotonin reuptake inhibitor (SSRI) class were widely available during this period. The institutional review board of Weill Cornell Medical College approved study procedures. Written informed consent was obtained before study assessments were conducted.
A total of 166 participants who met criteria for major depressive disorder and were reinterviewed three months and six months after admission constituted the study sample. This group of participants is a subsample of the larger study ( 7 ). At admission and at the six-month follow-up, participants were administered the 17-item Hamilton Rating Scale of Depression (HAM-D) to assess depression severity; the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) to measure pain, social functioning, and physical functioning; and the Cornell Services Index ( 8 ) to catalogue recent use of medical and mental health services.
The three- and six-month assessments evaluated depressive symptom severity and treatment adequacy with scales from the Longitudinal Interval Follow-up Evaluation (LIFE) ( 9 ). The LIFE's Psychiatric Status Rating (PSR), used in the original study conducted by Keller and associates ( 6 ), offers a 6-point scale to rate depression severity from 1 to 6 relative to full major depression criteria on a weekly basis. In our study, we defined remission status as having a PSR score of 1 or 2 (having no symptoms or having no more than a mild degree of one symptom), whereas major depression was defined as having a PSR score of 3 or more for the preceding two weeks. A PSR score of 3 either indicates a partial remission from an index episode with clinically significant persistent symptoms or a recurrence of depressive symptoms that does not meet full criteria for major depression of a patient who had been in remission for depression. The two-week duration criterion for remission is shorter than the six-month period required for achieving full recovery in the longer-term observational study reported by Keller ( 10 ). However, this criterion is consistent with shorter-term treatment studies, including those assessing the impact of residual symptoms on the subsequent course of depression. The prognostic importance of being symptom free for a minimum of two weeks is supported by evidence that incomplete remission predicts a poorer course of depression ( 11 ).
As in the Collaborative Study of the National Institute of Mental Health (NIMH), antidepressant intensity was measured with the 5-point Composite Antidepressant Scale (CAD), with ratings modified to include newer classes of antidepressants ( 5 ). Adequate treatment was defined as a weekly CAD score of 3 or more for a minimum of four consecutive weeks for one or more antidepressants. The three- and six-month follow-up assessments were conducted whether or not participants had continued treatment in the clinic from which they had been recruited.
Data analyses were conducted to construct a parsimonious and clinically informative model describing the likelihood of major depression at six months after admission based on the hypothesized predictors: early treatment adequacy, remission from depression at three months as defined by a PSR score of 1 or 2, and log-transformed duration of the index episode. Before the multivariate analysis was conducted, we made bivariate comparisons to identify associations between nonremission and baseline clinical variables.
Results
The study sample represents adults who completed the three- and six-month follow-up interviews. Of the sample of adults who completed the baseline assessment, 67% (166 of 247) completed both three- and six-month follow-up assessments. The group unavailable for follow-up assessments was younger (t=-2.17, df=245, p<.05) than the particpating sample. The mean±SD age of participants was 46.8±18.0. The 166 participants had a mean level of education of 13.3±2.8 years. Sixty-nine percent of the sample (114 of 166) were female, 14% (24 of 166) were black, 12% (20 of 166) were of Hispanic descent, 74% (122 of 166) were white, and 63% (105 of 166) filled a prescription and took at least one dose of prescribed antidepressants.
Of the 166 participants, 39% (64 participants) met PSR criteria for major depression at six months. Specifically, 33% (55 participants) of the sample had depression at three months and continued to be depressed (PSR scores of 4 or 5) at six months, 13% (21 participants) had been in a partial or full remission at three months but were depressed at six months, and 15% (26 participants) were depressed at three months but in remission at six months.
Seventy-one percent of patients (117 participants) had index episodes less than 12 months at the six-month follow-up, with the mean length of episode being 13.3±16.8 months. Twenty percent (34 participants) had index episodes greater than six months but less than 12 months. The 122 participants who had a prior episode of major depression had 2.93±3.1 prior episodes.
In bivariate analyses (see Table 1 ), participants who achieved six-month remission status (both newly remitted and sustained remission) had better baseline physical functioning (t=-3.79, df=162, p<.05), had reported less pain (t=-2.52, df=162, p<.05), had fewer prior hospitalizations ( χ2 =7.21, df=1, p=.007), had shorter length of index episode of major depressive disorder (log transformed) ( χ2 =2.61, df=161, p=.010), and were married ( χ2 =7.47, df=2, p=.006). Half of the participants with depression in remission or not in remission reported continued mental health treatment at six months. As noted in Table 1 , meeting criteria for personality dysfunction did not distinguish participants whose depression was in remission versus not in remission at six months.
 |
Among participants who reported adequate antidepressant treatment therapy in the first three months, 49% (40 of 81 participants) continued to meet criteria for depression at six months compared with 73% (62 of 85) who had no pharmacotherapy or whose antidepressant treatment did not meet the threshold for adequacy. Also, among participants who reported using antidepressant therapy between three and six months, 73% (77 of 105) met criteria for an adequate dosage for four weeks. Receiving adequate pharmacotherapy between months 3 and 6 was not associated with depression outcome at six months.
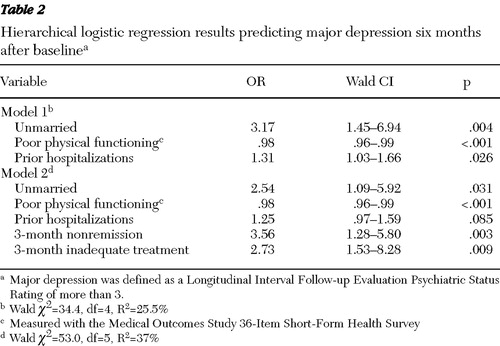
Multivariate analyses of predictors of remission included the hypothesized predictors and variables with significant bivariate relationships: marital status, physical functioning, pain, number of prior hospitalizations, HAM-D rating at admission, duration of index episode, three-month depression status (remitted or not remitted), and treatment adequacy. Of these predictors, being unmarried, having a greater number of previous hospitalizations, and having worse physical functioning were independent predictors of depression status at six months (model 1, Table 2 ). When both three-month nonremission status and three-month inadequate pharmacotherapy treatment were added to the model, the number of previous hospitalizations did not remain a significant predictor of major depression at six months.
 |
We conducted post hoc analyses to explore whether the absence of an effect in the three- to six-month period was due to either the more chronic patients' receiving persistently intense pharmacotherapy or remitted patients' discontinuing pharmacotherapy before this period. A bivariate analysis examining the relationships between baseline chronicity based on a median split of duration of index episode (median=48 months) and medication adherence during the second three months did not reveal an association (p=.646).
Discussion
Among adults seeking community mental health treatment for major depression, fewer than four out of ten had a sufficiently significant reduction in depressive symptoms to be considered in remission six months after clinic admission, whether or not antidepressant treatment had been used. The rate of remission was the same as for those assessed at three months ( 5 ). Only one in five adults who sought care achieved remission at both three and six months. Participants in remission at three months were more than three times as likely as those without a three-month remission to be in remission at six months. One-third of participants met criteria for major depression at both three and six months. These findings support the importance of early nonremission as a predictor of sustained depression for at least six months. It is likely that participants who are in the large clinical trials focusing on optimal treatment of resistant or chronic depression could be identified after the first three months of treatment.
Our findings suggest that early adequacy of pharmacotherapy and early pharmacotherapy response are important independent predictors of depression outcomes at six months. Recent findings from the STAR*D trial demonstrate that individuals who responded after only eight weeks of treatment (considered early responders) were the group of individuals who typically achieved remission. The STAR*D study supports 12 weeks as a clinically meaningful period to monitor response. Clinical trials are documenting that patients who do not respond early are at greater risk of later treatment failure, which highlights the need for continued, early aggressive monitoring of patients ( 12 ).
The data from this naturalistic community-based study underscore the potential prognostic importance of early response to pharmacotherapy. Only adequate pharmacotherapy during the first three months predicted six-month remission. Early remission independently predicted status at six months regardless of later treatment adequacy (at three and six months). Nevertheless, we cannot explain why later treatment adequacy during the three months after clinic admission was not a significant predictor of six-month remission.
Regardless of the lack of an association between adequate pharmacotherapy during the second three months and six-month outcomes, these findings are consistent with the recommendations of the American College of Neuropsychopharmacology Task Force, that monitoring and appropriately altering an individual's treatment regimen are necessary for improved chances of remission and recovery. These treatment factors combined with prior course of illness (hospitalizations) and physical health status differentiate who achieves remission within six months of seeking care. The construct of sustained depression at six months is related to the construct of chronic depression. Whereas chronicity has been used traditionally to describe the duration of a depressive episode, the syndrome of chronic depression ( 1 , 6 ) is closely tied to that of treatment resistance ( 1 , 4 , 13 ). Among participants in this study, the duration of the index episode, whether measured as a continuous variable or through a median split, did not predict persistence to six months. Our results can determine neither the extent to which participants with persistent depression at six months were treatment resistant before study entry nor the persistence of the index major depressions subsequent to the six-month assessment.
Our study has several limitations. First, we were unable to report fully on the efficacy and quality of treatment or to determine patient- and clinician-related factors that may have influenced whether antidepressants were continued. Second, we cannot ascertain the types of treatment offered beyond the antidepressant therapy dosage and duration and the number of psychotherapy visits. In the absence of data with more frequent assessment about changes in symptom severity, we cannot ascertain whether participants experienced more frequent switches into or out of major depression and whether transient fluctuations influenced depression status at six months. The fact that these data were collected over a decade ago may limit their relevance today. Nevertheless, a more recent study found that between 1987 and 1997, the number of individuals treated with antidepressant medications increased substantially, from 37% to 75%, which was primarily attributable to the introduction of SSRIs ( 14 ). Nevertheless, these data on prescription rates did not consider the duration of pharmacotherapy or classify treatment by adequacy. Weilburg and colleagues ( 15 ) conducted a secondary analysis of a pharmacy database and found an association between SSRI treatment and adequacy of antidepressant treatment; nevertheless, only 54% of the outpatients with depression treated only by psychiatrists met minimum dosage and duration criteria for adequacy. This percentage is higher than the recent finding that only 31% of 801 patients who met criteria for depression had had an adequate antidepressant trial at entry into an NIMH trial for chronic depression ( 13 ). Unfortunately, the more frequent prescription of antidepressants has not been associated with an increase in adequacy of treatment for nearly half of the patients who seek outpatient care for depression.
Conclusions
Recognizing sociodemographic and clinical characteristics that are predictive of major depression in community outpatient mental health care may help in the early identification of individuals who are particularly susceptible to sustaining poor outcomes. In addition, the importance of early adequate pharmacotherapy and response to treatment in predicting the course of depression supports an emphasis on early care as a gateway to potential prevention of persistent depressive symptoms.
Acknowledgments and disclosures
This work was supported in part by grants MH-53816 (Dr. Weinberger), MH-53816 (Dr. Meyers), P30-MH-068638, and MH-19132 from the National Institute of Mental Health. The authors thank Steve Freedman, M.A., the staff of the Westchester County Office of Mental Health, and the participants for their support of this study.
The authors report no competing interests.
1. Kocsis JH: New strategies for treating chronic depression. Journal of Clinical Psychiatry 61(suppl 11):42–45, 2000Google Scholar
2. Thase ME: Preventing relapse and recurrence of depression: a brief review of therapeutic options. CNS Spectrums 11(12 suppl 15):12–21, 2006Google Scholar
3. Nierenberg AA, Fava M, Trivedi MH, et al: A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. American Journal of Psychiatry 163:1519–1530, 2006Google Scholar
4. Trivedi MH, Fava M, Wisniewski SR, et al: Medication augmentation after the failure of SSRIs for depression. New England Journal of Medicine 354:1243–1252, 2006Google Scholar
5. Meyers BS, Sirey JA, Bruce M, et al: Predictors of early recovery from major depression among persons admitted to community-based clinics: an observational study. Archives of General Psychiatry 59:729–735, 2002Google Scholar
6. Keller MB, Lavori PW, Rice J, et al: The persistent risk of chronicity in recurrent episodes of nonbipolar major depressive disorder: a prospective follow-up. American Journal of Psychiatry 143:24–28, 1986Google Scholar
7. Sirey JA, Meyers BS, Bruce ML, et al: Predictors of antidepressant prescription and early use among depressed outpatients. American Journal of Psychiatry 156:690–696, 1999Google Scholar
8. Sirey JA, Meyers BS, Teresi JA, et al: The Cornell Service Index as a measure of health service use. Psychiatric Services 56:1564–1569, 2005Google Scholar
9. Keller MB, Lavori PW, Friedman B, et al: The Longitudinal Interview Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry 44:540–548, 1987Google Scholar
10. Keller MB: Remission versus response: the new gold standard of antidepressant care. Journal of Clinical Psychiatry 65(suppl 4):53–59, 2004Google Scholar
11. Kennedy N, Paykel ES: Residual symptoms at remission from depression: impact on long-term outcome. Journal of Affective Disorders 80:135–144, 2004Google Scholar
12. Keitner GI, Ryan CE, Miller IW, et al: Recovery and major depression: factors associated with twelve-month outcome. American Journal of Psychiatry 149:93–99, 1992Google Scholar
13. Kocsis JH, Gelenberg AJ, Rothbaum B, et al: Chronic forms of major depression are still undertreated in the 21st century: systematic assessment of 801 patients presenting for treatment. Journal of Affective Disorders 110:55–61, 2008Google Scholar
14. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Google Scholar
15. Weilburg JB, O'Leary KM, Meigs JB, et al: Evaluation of the adequacy of antidepressant treatment. Psychiatric Services 54:1233–1239, 2003Google Scholar



