Assessment and Classification of Patients With Psychiatric and Substance Abuse Syndromes
Editor's Note: The article reprinted here was first published in the October 1989 issue of Hospital and Community Psychiatry, at a time when large numbers of patients who would formerly have been institutionalized were living in the community and had much greater access to alcohol and drugs. Clinicians were increasingly encountering the diagnostic and treatment challenges presented by patients with mental illness and substance use disorders. In this paper Dr. Lehman and his colleagues describe issues that must be addressed in the assessment of patients who may have a dual diagnosis. In the early phases of treatment, two major pitfalls exist for the clinician: failure to consider that the patient may have dual disorders and presumption of the primacy of either the psychiatric or the substance use disorder. Decisions about long-term treatment depend on the clinician's hypothesis about why the patient has a dual diagnosis. The authors discuss four hypotheses about how dual disorders develop. The discussion section raises numerous questions that more than a decade later continue to be addressed by researchers on dual disorders.
Patients with both mental illness and substance abuse pose a major clinical challenge to mental health and substance abuse clinicians. The literature seems to support the hypothesis that mental illness and substance abuse occur together more frequently than chance would predict. Assessment and classification of these patients should be guided by clinicians' needs to make meaningful therapeutic judgments and to communicate effectively with each other in coordinating treatment. Different phases of treatment require different approaches to assessment and classification. In initial classification, the clinician should recognize the problem of dual diagnosis and resist premature assumptions about which diagnosis is primary. Long-term treatment and rehabilitation may require systematic evaluation of alternative clinical hypotheses about why a patient exhibits both disorders. This approach eventually may lead to better ways to assess, classify, and treat these difficult patients.
Methods of clinical assessment and classification must be guided by their clinical utility—that is, by the clinician's need to make appropriate therapeutic decisions and to communicate effectively with other care providers. The dilemma faced in developing a classification system for dual diagnosis patients is that relatively little is known about the nature of these patients' problems and what helps them. Therefore, it is not clear what must be assessed to classify them most appropriately for treatment.
This uncertainty increases the need to adopt a systematic approach to assessment and classification that will contribute to the development of more effective treatments and services. Assessment and classification may be most usefully viewed as open-ended clinical procedures for planning treatment on a case-by-case basis; accumulation of treatment results may in turn influence future classification. This iterative process linking classification and treatment outcome may lead to better systems of classification and thence to better care.
This paper is divided into three sections. First, the literature on the magnitude of the problem of persons with both mental illness and substance abuse is briefly reviewed. Second, assessment and classification issues relevant to different phases of treatment for these patients are discussed. In particular a phenomenologic approach early in treatment and a clinical hypothesis-testing approach later in treatment are stressed. Third, some of the many major questions that still must be addressed in the assessment, classification, and treatment of patients with mental illness and substance abuse are identified.
Magnitude of the problem
The National Institute of Mental Health's Epidemiologic Catchment Area (ECA) study has provided good epidemiological data on the lifetime prevalence of substance abuse disorders and psychiatric disorders in the general population. The rates range from 15 to 18 percent for substance abuse (12 to 16 percent for alcohol, 5 to 6 percent for drugs) and 19 to 30 percent for psychiatric disorders (1). Of particular relevance to this discussion is the ECA finding that substance use disorders co-occur with various mental disorders more frequently than chance alone would predict (2). These community-based epidemiologic findings of comorbidity are consistent with other studies from both the mental health and substance abuse literature, which have reported high rates of psychiatric symptoms among substance abusers (3,4,5,6,7) as well as high rates of substance abuse among psychiatric patients (8,9,10,11,12,13,14,15,16).
Such comorbid states have major clinical implications. The severity of psychiatric symptoms in persons seeking treatment for primary substance abuse is one of the best predictors of substance abuse outcome, with more severe symptoms predicting poorer outcomes (17,18). Similarly, the outcomes for psychiatric patients with a substance abuse disorder are typically poorer than outcomes for psychiatric patients without a substance abuse disorder (10,19,20,21). This relationship necessitates more effective treatment for patients with both substance abuse and mental disorders.
Phases of treatment
For the sake of discussion, treatment for the dually diagnosed patient can be divided into two phases: acute treatment and stabilization, and maintenance and rehabilitation. The assessment and classification issues relevant to these phases differ and will be discussed separately.
Acute treatment and stabilization
This initial phase of treatment begins with the first contact with the patient and can last for several weeks or months. Treatment during this phase includes observation, management of acute intoxication and withdrawal, management of acute psychiatric symptoms, and restabilization of the patient to a baseline condition.
The first assessment task from the standpoint of dual diagnosis is to evaluate the possibility that the patient has both substance abuse and psychiatric problems. Does the patient show psychiatric symptoms and evidence of substance intoxication or withdrawal? If so, do the psychiatric symptoms clear as detoxification proceeds? If the psychiatric symptoms clear completely with detoxification and the patient has no prior history of psychiatric disorder, then the patient should not receive a dual diagnosis. Conversely, if the psychiatric symptoms do not fully abate with detoxification or if the patient has a prior history of psychiatric illness, then the possibility of dual diagnosis should be considered.
One major pitfall during this initial assessment phase is the failure to adequately consider the possibility of both problems, to either overlook or misattribute the symptoms of one of the disorders to the other. DSM-III-R offers a clear and systematic framework for assessing the presence of substance abuse and psychiatric syndromes. Clinicians should be conversant with the DSM-III-R criteria for mental disorders and substance abuse disorders and apply them in a thorough initial evaluation. Lack of familiarity with this or some other well-defined set of criteria may lead to premature closure about the presence of either type of problem.
A second major pitfall during the assessment phase is to presume the primacy of either the psychiatric or the substance abuse disorder. Despite the shortage of empirical data to guide us, there seems a consensus in the literature that this phase of treatment should include concurrent treatment for both disorders (22). This approach avoids the disjointed treatment so often encountered by these patients, who are referred back and forth between psychiatric and substance abuse treatment programs that view one of the disorders as primary and argue that the other cannot be addressed until the first is stabilized. It is not clear whether patients can be effectively treated by involvement in both types of programs simultaneously or whether hybrid programs are needed (22). In any event, the key to assessment and treatment in this phase is to identify and treat all syndromes present.
At first glance it would seem a relatively easy task, given careful and thorough assessment, to decide which patients have a dual diagnosis and to establish which syndromes are present, but this is not always the case. Persons with well-documented histories of a major mental illness plus well-documented histories of alcoholism or drug dependence fall clearly into the realm of dual diagnosis. Patients experiencing transient psychiatric symptoms clearly attributable to intoxication or withdrawal would not receive a dual diagnosis. However, clinicians encounter more difficulty when considering less definitive or more chronic levels of psychiatric symptoms and substance abuse.
For example, the following types of patients are examples of less clear candidates for dual diagnosis: a person with an episode of major depression who drinks alcohol while depressed; a person with manic-depressive illness who drinks when manic; a person with schizophrenia who takes stimulants, perhaps to counteract neuroleptic side effects or the negative symptoms of schizophrenia; a person who abuses amphetamines, intermittently becomes psychotic, and is dysphoric without stimulants; and a person with alcoholism who develops persistent first-rank symptoms of schizophrenia in the postwithdrawal phase. Put more generally, when does the use of psychoactive substances constitute abuse among the mentally ill and when should psychiatric symptoms among substance abusers be considered mental illness? Currently it is not evident where to draw the line or even if the assumption of such a line is valid.
Given current concerns about the tendency to overlook the existence of dual problems, the most prudent recommendation is to attend carefully to the presence of any persistent psychiatric symptoms and any persistent substance abuse. Thus the two major recommendations for assessment of dual diagnosis patients during acute treatment and stabilization are to conduct a thorough examination for both types of disorders and to avoid premature decisions about which disorder might be primary.
Maintenance and rehabilitation
Maintenance and rehabilitation is a long-term phase of treatment that seeks to prevent recurrence of the disorders through continued medical and psychosocial interventions. Such interventions may include the broad array of services offered to persons with either substance abuse or mental illness: medications, psychotherapy, self-help, and rehabilitation. The key question during assessment and classification of what long-term treatments are necessary becomes more relevant in this phase to ascertain whether the patient's disorders have a hierarchical structure and what factors contribute to the long-term risk of recurrence. During this phase, a variety of clinical hypotheses about how the patient has come to be dually diagnosed gain relevance.
The clinician may need to address various treatment questions. Does the patient need maintenance pharmacotherapy for mental illness (neuroleptics, antidepressants, or lithium), for substance abuse (disulfiram or methadone), or for both? Would the patient benefit from psychosocial treatments, and if so, which ones? Patients with psychotic disorders may not do well in standard substance abuse self-help programs, and persons with primary substance abuse problems may not fit well into psychosocial programs for the seriously mentally ill. The vocational rehabilitation needs of persons suffering from psychotic disorders with secondary alcohol abuse may differ from those of alcoholics with intermittent psychotic symptoms associated with intoxication or withdrawal. Decisions about long-term treatment will depend on the clinician's hypothesis about why a given patient is dually diagnosed.
Following are discussions of four clinical hypotheses about how dual diagnosis conditions develop: primary mental illness with substance abuse sequelae, primary substance abuse with psychiatric sequelae, dual primary diagnosis, and common etiology. They are mutually exclusive in a given case, but different hypotheses probably account for different segments of the dually diagnosed population. The four hypotheses also are not necessarily the only possible hypotheses, but they illustrate the kinds of clinical reasoning inherent to many current discussions of the dually diagnosed. All are longitudinal hypotheses about illness, in contrast to the cross-sectional, phenomenologic diagnostic approach needed in the earlier phase of treatment. Table 1 summarizes the types of assessments that may be helpful in classifying patients according to these four clinical hypotheses.
Primary mental illness with substance abuse sequelae. In this hypothesis, the patient suffers from a primary mental illness, and the symptoms and sequelae of the illness or its treatment (for example, medication side effects) lead to addictive behavior as a way of coping with the illness. This hypothesis encompasses the concept of self-medication (23,24,25) but also covers secondary substance abuse attributable to such factors as impaired judgment and social passivity.
The literature on risk factors for addictive behavior is striking for the fact that most of the risk factors are present with mental illness (26). Risk factors for addictive behavior include negative affect states, impaired cognition, misinterpretation of internal cues, poor self-esteem, lack of a sense of self-control and self-efficacy, poor role performance, impaired social skills, restricted coping capacities, disturbances of vegetative functions, and lack of social supports.
Given this literature, it should come as no surprise that the mentally ill suffer from high rates of substance abuse. The risk of addictive behavior may be increased via multiple nonspecific symptoms and sequelae of mental illness. For example, the dysphoria, demoralization, loss of self-esteem, and loss of functioning associated with many persistent mental illnesses may lead to a nonspecific search for relief in abused substances. Such a scenario would not entail an association between specific mental disorders and specific substances of abuse.
Some of the literature supports a second, more specific self-medication hypothesis (2,25,27). Certain mental illnesses may predispose patients to abuse specific substances that in some way alleviate the immediate negative effects of that mental illness. Numerous possible examples are reported in the literature, including an increased association of psychostimulant abuse with psychotic disorders (15,27,28) and of abuse of alcohol and other central nervous system depressants with affective disorders (15,29,30). However, other reports counter these patterns (8,25,31,32), so the data on consistent associations between specific mental disorders and specific types of substance abuse are by no means conclusive.
The self-medication hypothesis may provide some intriguing clues to the underlying pathophysiology of various mental illnesses. For example, Cesarec and Nyman (33) found differential responses to amphetamines among different subgroups of schizophrenic patients; patients with only deficit symptoms of schizophrenia tended to improve on a combination of neuroleptic and amphetamine, whereas those with active psychotic symptoms worsened. Perhaps differences in substance abuse patterns among patients within a given DSM-III-R diagnosis could provide useful clues to differentiating physiologically heterogeneous subtypes.
DiSalver (30) has proposed that the substances typically abused by patients with affective disorders may provide clues to the pathophysiologies of these disorders, and he specifically proposes a connection between abuse of anticholinergic substances and the monoamine theory of affective disorders. Khantzian (25) has provided specific psychodynamic hypotheses linking the abuse of heroin and cocaine to specific psychiatric syndromes. It is not currently known whether such lines of speculation will yield useful information for future classification.
The implications of this hypothesis for maintenance and rehabilitation for such a patient are that the principal focus of treatment will be on alleviating the symptoms and sequelae of the mental illness, with the assumption that the sustained amelioration of these symptoms and sequelae will lead to resolution of the substance abuse. Most likely such a patient would be treated by the mental health care system in the long term. However, if dependency on the substance has developed, the substance abuse may need to be treated as a primary problem in its own right.
Primary substance abuse with psychiatric sequelae. This hypothesis holds that the patient suffers primarily from substance abuse and that psychiatric symptoms are a manifestation of the effects of the substance(s) abused. Examples include the rebound depression in the use of cocaine and other stimulants (34), impairments in cognitive functioning and thought processes due to alcohol (35), psychoses induced by phencyclidine, amphetamine, lysergic acid diethylamide, and other psychotomimetics (36,37). This hypothesis covers the acute psychiatric syndromes associated with intoxication and withdrawal, and such cases can usually be recognized as not true dual diagnosis as the patient becomes detoxified.
A more intriguing and elusive question is whether primary substance abuse can lead to persistent mental illness in the absence of continued substance abuse. Some evidence does support this hypothesis, including the chronic psychotic states associated with long-term abuse of stimulants (38,39,40) and persistent affective disorders related to abuse of central nervous system depressants and other agents (30,38).
Whether these patterns of persistent mental disorders following primary substance abuse are the result of a preexisting vulnerability to mental illness uncovered by the substance abuse or of persistent changes in brain physiology directly attributable to the abused substance remains an open issue. Patients fitting this hypothesis may receive maintenance and rehabilitation primarily in substance abuse programs.
Dual primary diagnosis. Under the hypothesis of dual primary diagnosis, the patient suffers from two initially unrelated disorders that may interact to exacerbate each other. The apparent increased co-occurrence of mental illness and substance abuse above that predicted by chance tends to argue against this hypothesis (2). However, this model may apply to some subgroups. For example, studies generally have not found an excess prevalence of alcoholism among patients with schizophrenia (28,41,42), although even this finding has not been entirely consistent in the literature (2). The particular relevance of this model is that even co-occurrence of primary psychiatric and substance abuse disorders may alter the presentation of either, making diagnosis and treatment more difficult.
The treatment implication for this hypothesis is that such dually diagnosed patients will need maintenance and rehabilitation for both psychiatric and substance abuse disorders. They will require either parallel treatment in both the mental health and substance abuse service sectors or treatment in a "hybrid" program (22).
Common etiology. The hypothesis of common etiology posits that common underlying factors may predispose a patient both to mental disorders and to substance abuse disorders. Certainly the most common example is the idea that alcoholism and affective disorders are familially linked (43,44,45), but there is dispute about whether this connection indicates a common underlying genetic factor (32) or other phenomena, such as assortative mating (46).
Regardless of whether a genetic link exists, some dual disorders may share a common biologic etiology. Defects in dopaminergic function may predispose patients to schizophrenia and to abuse of such dopamine agonists as amphetamine (33). Similarly, defects in cholinergic activity may predispose patients to affective disorders and to abuse of drugs affecting cholinergic pathways (30). Finally, one may postulate common psychosocial factors that predispose to mental illness and to substance abuse, such as homelessness as a risk factor for both depression and substance abuse (47).
The treatment implication of the hypothesis of common etiology is that if such a common underlying etiologic factor exists, the treatment should be aimed at this factor. Presumably, effective intervention with this factor will alleviate both the psychiatric and substance abuse disorders.
Discussion
The major implication of the existing literature and all but one of the clinical hypotheses discussed above is that dual diagnosis is not simply a statistical phenomenon of co-occurrence but rather an interactive phenomenon placing mentally ill persons at high risk for substance abuse and substance abusers at high risk for mental illness. This apparent synergism raises great concern in this era of increased freedom for the mentally ill in a culture plagued by high rates of substance abuse. Clinicians must struggle with the many unanswered questions as best they can for their patients, until those questions are addressed by systematic research.
For individual cases, some questions may provide clues to appropriate continuing treatment: What problem began first in the patient's history, substance abuse or mental illness? Do episodes of substance abuse clearly occur in subsequent temporal relation to psychiatric symptoms and sequelae, or do psychiatric symptoms tend to occur only subsequent to substance abuse? Do the symptoms of mental illness return when treatment for these symptoms is discontinued in the absence of substance abuse? Does substance abuse continue in the absence of psychiatric symptoms? Is there a family history for mental illness or substance abuse?
These questions are not always easy to answer even for a patient who manages to abstain from substance abuse. Careful history from multiple sources, close monitoring of the patient's condition during the initial treatment phase, ongoing surveillance for continued substance abuse, and trials of alternative treatments (for example, discontinuation of neuroleptic medication when the patient is asymptomatic) are all necessary to arrive at some conclusion.
With regard to the development of more effective assessment and classification systems for these patients, many questions await research: What demographic, clinical, and functional attributes distinguish mentally ill patients who abuse substances from those who do not? Do patients in different diagnostic categories truly differ in the types of substances abused and the severity of abuse? What are the most typical subgroups of mentally ill substance abusers, those who might receive high priority for more intensive assessment and intervention? How relevant is substance abuse to subsequent outcome, and what subgroups of dually diagnosed patients have especially poor outcomes and therefore are most in need of intervention? At what point does recreational use of such common substances as alcohol and marijuana begin to affect outcome?
Is substance use always tantamount to abuse among the mentally ill? Which nonabusing patients are at risk for the subsequent development of substance abuse? Are there subgroups in whom recreational use seems to enhance outcome, suggesting so-called self-medication? Do certain patterns of co-occurrence pose especially high risk for misdiagnosis? Do certain patterns of co-occurrence offer valuable clues to underlying heterogeneity within a psychiatric diagnostic category? Does the abused drug of choice provide clues to innovative pharmacotherapeutic strategies? The two goals of a classification system—treatment planning and professional communication—can only be met by a system that incorporates answers to many of these questions.
Finally, questions need to be raised about our current approach to classification as exemplified by DSM-III-R, which at times may encourage clinicians to reach premature conclusions about the hierarchical nature of a patient's dual disorder and obscure the interaction of mental disorders and substance abuse. Indeed, the idea of dual diagnosis arises from our theoretical segregation of mental disorders and substance abuse.
It is not clear whether this conceptual duality makes sense clinically. Many of these patients may suffer from multiple disorders, so dual diagnosis is a misleadingly simple notion. Clearly DSM-III-R offers an excellent means for describing the phenomena of mental disorders not associated with substance abuse and of substance abuse disorders not associated with other psychopathology. The question that we currently face is whether to take a more basic empirical look at the co-occurrence of psychiatric symptoms and substance abuse and explore alternative means of classification.
One approach to this question would be to evaluate the performance of DSM-III-R diagnoses compared with empirically derived symptom-behavior clusters for predicting the needs and treatment responses of dually diagnosed patients. Such cluster analyses have been conducted before to explore new ways to look at mental disorders (48,49,50). Such an empirically derived classification system would identify homogeneous clusters of patients, each cluster having a common pattern of symptoms and behaviors. These clusters would not necessarily correspond to DSM-III-R diagnoses; that is, a cluster might contain patients who exhibit symptoms of alcohol use, cocaine use, marijuana use, depression, and anxiety. Rather than giving such patients multiple DSM-III-R diagnoses, they would be designated as members of a group of patients with similar problems. The clinical utility of this clustering approach could then be examined in prospective studies of outcome and treatment.
Spitzer and Williams (51) recently proposed a similar procedure for maximizing the impact of psychiatric research on the evolution of psychiatric diagnostic criteria. They recommend a "multiplex research design" in which the validity of various diagnostic approaches are compared in multiple centers with multiple experts assessing multiple diagnostic criteria sets against multiple, longitudinal external validators, such as response to treatment, familial aggregation, stability over time, and laboratory tests of biological variables.
It is premature to propose the substitution of other diagnostic approaches over DSM-III-R for categorizing dually diagnosed patients. However, clustering techniques and multiple diagnostic research studies would test existing assumptions about what ails such patients and how they should be treated. This evaluation would force a harder look at the clinical complexities of these patients. Appropriate treatment of dually diagnosed patients depends on meaningful classification. If current classification systems are artificially constrained, then treatment and research on this population of patients will be greatly impeded.
Acknowledgment
Preparation of this manuscript was supported by National Institute on Drug Abuse grant RO1-DA05114.
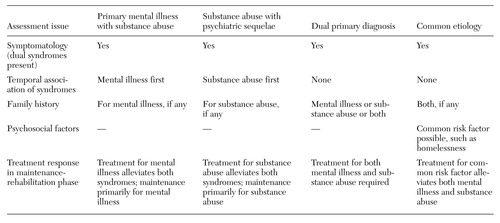 |
Table 1. Hypotheses of development and assessment findings for dual diagnosis conditions
1. Robins LN, Helzer JE, Weissman MM, et al: Lifetime prevalence of specific psychiatric disorders in three sites. Archives of General Psychiatry 41:949-958, 1984Crossref, Medline, Google Scholar
2. Boyd JH, Burke JD Jr, Gruenberg E, et al: Exclusion criteria of DSM-III: a study of co-occurrence of hierarchy-free syndromes. Archives of General Psychiatry 41:983-989, 1984Crossref, Medline, Google Scholar
3. Dorus W, Senay EC: Depression, demographic dimensions, and drug abuse. American Journal of Psychiatry 137:699-704, 1980Link, Google Scholar
4. Kosten TR, Rounsaville BJ: Psychopathology in opioid addicts. Psychiatric Clinics of North America 9:515-532, 1986Crossref, Medline, Google Scholar
5. Millman RB, Sbriglio R: Patterns of use and psychopathology in chronic marijuana users. Psychiatric Clinics of North America 9:533-545, 1986Crossref, Medline, Google Scholar
6. Mirin SM, Weiss RD: Affective illness in substance abusers. Psychiatric Clinics of North America 9:503-514, 1986Crossref, Medline, Google Scholar
7. Rounsaville BJ, Weissman MM, Rosenberger PH, et al: Detecting depressive disorders in drug abusers. Journal of Affective Disorders 1:255-267, 1979Crossref, Medline, Google Scholar
8. Alterman AI, Erdlen FR, Murphy E: Alcohol abuse in the psychiatric hospital population. Addictive Behaviors 6:69-73, 1981Crossref, Medline, Google Scholar
9. Alterman Al, Erdlen DL, LaPorte DJ, et al: Effects of illicit drug use in an inpatient psychiatric population. Addictive Behaviors 7:231-242, 1982Crossref, Medline, Google Scholar
10. Bergman HC, Harris M: Substance abuse among young adult chronic patients. Psychosocial Rehabilitation Journal 9:49-54, 1985Crossref, Google Scholar
11. Fischer DE, Halikas JA, Baker JW, et al: Frequency and patterns of drug abuse in psychiatric patients. Diseases of the Nervous System 36:550-553, 1975Medline, Google Scholar
12. Hasin D, Endicott J, Lewis C: Alcohol and drug abuse in patients with affective syndromes. Comprehensive Psychiatry 26:283-295, 1985Crossref, Medline, Google Scholar
13. McLellan AT, Druley KA: Non-random relationship between drugs of abuse and psychiatric diagnosis. Journal of Psychiatric Research 13:179-184, 1977Crossref, Medline, Google Scholar
14. Pepper B: The young adult chronic patient: population overview. Journal of Clinical Psychopharmacology 5:3S7S, 1985Crossref, Medline, Google Scholar
15. Richard ML, Liskow BI, Perry PJ: Recent psychostimulant use in hospitalized schizophrenics. Journal of Clinical Psychiatry 46:79-83, 1985Medline, Google Scholar
16. Schwartz SR, Goldfinger SM: The new chronic patient: clinical characteristics of an emerging subgroup. Hospital and Community Psychiatry 32:470-474, 1981Abstract, Google Scholar
17. LaPorte DJ, McLellan AT, O'Brien CP, et al: Treatment response in psychiatrically impaired drug abusers. Comprehensive Psychiatry 22:411-419, 1981Crossref, Medline, Google Scholar
18. McLellan AT, Luborsky L, Woody GE, et al: Predicting response to alcohol and drug abuse treatments: role of psychiatric severity. Archives of General Psychiatry 40:620-625, 1983Crossref, Medline, Google Scholar
19. McCarrick AK, Manderscheid RW, Bertolucci DE: Correlates of acting-out behaviors among young adult chronic patients. Hospital and Community Psychiatry 36:848-853, 1985Abstract, Google Scholar
20. Pepper B, Ryglewicz H: The young adult chronic patient and substance abuse. TIE Lines Quarterly Bulletin 1:1-5, 1984Google Scholar
21. Westermeyer J, Walzer V: Sociopathy and drug abuse in a young psychiatric population. Diseases of the Nervous System 36:673-677, 1975Medline, Google Scholar
22. Ridgely MS, Osher FC, Talbott JA: Chronic Mentally Ill Young Adults With Substance Abuse Problems: Treatment and Training Issues. Baltimore, University of Maryland, Mental Health Policy Studies Center, 1987Google Scholar
23. Wieder H, Kaplan EH: Drug use in adolescents: psychodynamic meaning and pharmacologic effect. Psychoanalytic Study of the Child 24:399-431, 1969Crossref, Medline, Google Scholar
24. Milkman H, Frosch WA: On the preferential abuse of heroin and amphetamine. Journal of Nervous and Mental Disease 156:242-248, 1973Crossref, Medline, Google Scholar
25. Khantzian EJ: The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. American Journal of Psychiatry 142:1259-1264, 1985Link, Google Scholar
26. Donovan DM: Assessment of addictive behaviors: implications of an emerging biopsychosocial model, in Assessment of Addictive Behaviors. Edited by Donovan DM, Marlatt GA. New York, Guilford, 1988Google Scholar
27. McLellan AT, Childress AR, Woody GE: Drug abuse and psychiatric disorders: role of drug of choice, in Substance Abuse and Psychology. Edited by Alterman AI. New York, Plenum, 1985Google Scholar
28. Schneier FR, Siris SG: A review of psychoactive substance use and abuse in schizophrenia: patterns of drug choice. Journal of Nervous and Mental Disease 175:641-652, 1987Crossref, Medline, Google Scholar
29. Bedi AR, Halikas JA: Alcoholism and affective disorder. Alcoholism: Clinical and Experimental Research 9:133-134, 1985Crossref, Medline, Google Scholar
30. DiSalver SC: The psychophysiologies of substance abuse and affective disorders: an integrative model? Journal of Clinical Psychopharmacology 7:1-10, 1987Google Scholar
31. Weiss RD, Mirin SM, Michael JL, et al: Psychopathology in chronic cocaine abusers. American Journal of Drug and Alcohol Abuse 12:17-29, 1986Crossref, Medline, Google Scholar
32. Spring GK, Rothgery JM: The link between alcoholism and affective disorders. Hospital and Community Psychiatry 35:820-823, 1984Abstract, Google Scholar
33. Cesarec Z, Nyman AK: Differential response to amphetamine in schizophrenia. Acta Psychiatrica Scandinavica 71:523-538, 1985Crossref, Medline, Google Scholar
34. Washton AM, Stone NS, Hendrickson EC: Cocaine abuse, in Assessment of Addictive Behaviors. Edited by Donovan DM, Marlart GA. New York, Guilford, 1988Google Scholar
35. Grant I, Reed R: Neuropsychology of alcohol and drug abuse, in Substance Abuse and Psychology. Edited by Alterman AI. New York, Plenum, 1985Google Scholar
36. Vardy MM, Kay SR: LSD psychosis or LSD-induced schizophrenia? A multimethod inquiry. Archives of General Psychiatry 40:877-883, 1983Crossref, Medline, Google Scholar
37. Castellani S, Petrie WM, Ellinwood E: Drug-induced psychosis: neurobiological mechanisms, in Substance Abuse and Psychology. Edited by Alterman AI. New York, Plenum, 1985Google Scholar
38. McLellan AT, Woody GE, O'Brien CP: Development of psychiatric disorders in drug abusers. New England Journal of Medicine 301:1310-1314, 1979Crossref, Medline, Google Scholar
39. Ellinwood E, Duarte-Escalante O: Chronic methamphetamine intoxication in three species of experimental animals, in Current Concepts on Amphetamine Abuse. Edited by Ellinwood E, Cohen S. Rockville, Md, National Institute of Mental Health, 1972Google Scholar
40. Bell DS: The experimental reproduction of amphetamine psychosis. Archives of General Psychiatry 30:35-40, 1973Crossref, Google Scholar
41. Alterman AI: Substance abuse in psychiatric patients, in Substance Abuse and Psychology. Edited by Alterman AL. New York, Plenum, 1985Google Scholar
42. Kendler KS: A twin study of individuals with both schizophrenia and alcoholism. British Journal of Psychiatry 147:48-53, 1985Crossref, Medline, Google Scholar
43. Hesselbrock MN, Hesselbrock VM, Tennen H, et al: Methodological considerations in the assessment of depression in alcoholics. Journal of Consulting and Clinical Psychology 51:399-405, 1983Crossref, Medline, Google Scholar
44. Himmelhoch JM, Hill S, Steunberg B, et al: Lithium, alcoholism, and psychiatric diagnosis. Journal of Psychiatric Treatment and Evaluation 5:83-88, 1983Google Scholar
45. Mayfield D: Substance abuse in the affective disorders, in Substance Abuse and Psychology. Edited by Alterman AL. New York, Plenum, 1985Google Scholar
46. Schuckit MA: The importance of family history of affective disorder in a group of young men. Journal of Nervous and Mental Disease 170:530-535, 1982Crossref, Medline, Google Scholar
47. Robertson MJ: Mental disorder among homeless persons in the United States: an overview of recent empirical literature. Administration in Mental Health 14:14-27, 1986Crossref, Google Scholar
48. Blashfield RK: Propositions regarding the use of cluster analysis in clinical research. Journal of Consulting and Clinical Psychology 48:456-459, 1980Crossref, Medline, Google Scholar
49. Blashfield RK, Morey LC: The classification of depression through cluster analysis. Comprehensive Psychiatry 20:516-527, 1979Crossref, Medline, Google Scholar
50. Overall JE, Hollister LE, Johnson M, et al: Nosology of depression and differential response to drugs. JAMA 195:946-948, 1966Crossref, Medline, Google Scholar
51. Spitzer RL, Williams JBW: Having a dream: a research study for DSM-IV. Archives of General Psychiatry 45:871-874, 1988Crossref, Medline, Google Scholar



