Outpatient Utilization Patterns of Integrated and Split Psychotherapy and Pharmacotherapy for Depression
Abstract
OBJECTIVE: This exploratory study examined utilization and costs among depressed patients in two treatment models—integrated treatment, in which psychotherapy and pharmacotherapy were provided by a psychiatrist, and split treatment, in which pharmacotherapy was provided by a psychiatrist and psychotherapy by a nonphysician psychotherapist. METHODS: A quasi-experimental retrospective design was used to compare claims data from a national managed mental health care organization for 191 patients in integrated treatment and 1,326 in split treatment. RESULTS: During the 18-month study, patients receiving integrated treatment used significantly fewer outpatient sessions and had significantly lower treatment costs, on average, than those in split treatment. Integrated treatment appeared to be associated with a pattern of utilization characterized by frequent treatment episodes in contrast to that of split treatment, which was characterized by more sessions with fewer breaks of 90 days or more. CONCLUSIONS: The results do not support the prevailing assumption that integrated treatment is more costly than split treatment in a managed care network. Despite limitations in the study methods, the strength of these preliminary findings poses a powerful challenge and invites further study.
Over the past 25 years, the role of psychiatrists in the public and nonprofit sector has become limited to writing prescriptions in state and county institutions, community mental health centers, and other organized service settings, with most nonprofit health maintenance organizations following suit. In the past decade, psychiatrists in the expanding managed private for-profit sector have been increasingly used as pharmacotherapists, while psychotherapy services have been provided by nonphysician mental health specialists.
The new carve-out managed behavioral health systems have usually adopted the practice of using psychiatrists for pharmacotherapy and other providers for psychotherapy. They have assumed that this approach is prima facie a more cost-effective use of resources because of the limited availability of psychiatrists within provider networks and the higher unit cost for their services. No empirical data have been published to support or refute this practice. As a result, psychiatrists have found it increasingly difficult to continue providing psychotherapy at the same level as in the past (1).
Parallel to the evolution of new organized delivery systems have been rapid advances in pharmacotherapy and increased clinical research on the effectiveness of psychotropic medications in the treatment of a growing number of mental disorders. These advances have promoted a shift toward biological models of treatment and for different reasons have reinforced the primacy for some psychiatrists of their role as pharmacotherapist. One result of these factors is that integrated treatment, in which a single clinician provides both psychotherapy and pharmacotherapy, appears to be less prevalent in most systems of care than split treatment, in which the pharmacotherapy is provided by a psychiatrist or a nonpsychiatrist physician and the psychotherapy by a nonphysician mental health specialist (2-4).
Chiles and associates (5) found that 63 percent of psychiatrists reported seeing during the past month at least one pharmacotherapy patient who was involved in psychotherapy with someone else. In the same survey 79 percent of psychologists reported providing psychotherapy for patients who were receiving psychoactive drugs. Likewise, a survey of psychiatrists in Connecticut found that two-thirds were currently providing medication backup, the majority of whom did so for more than one psychotherapist (6).
Although some observers have commented on the psychodynamics and therapeutic particulars of integrated versus split treatment, as well as on the associated ethical and legal questions (7-10), no analysis has tested the basic economic assumption that underlies the shift to split treatment. Only a little research has been done on the impact of the two models on service utilization and clinical outcomes (3,5,11,12).
In particular, with regard to depression, several studies have reported some level of benefit associated with the use of psychotherapy and pharmacotherapy treatment by one or two therapists (3,12–31). Yet no study has systematically assessed the impact of different combinations of providers of these treatments on health care utilization patterns and costs.
This retrospective study examined differences in the utilization patterns of depressed patients in integrated and split treatment. It did not attempt to determine the effectiveness of the various treatment combinations or examine the quality of care provided or the quality of life experienced by the patients. An additional purpose of the study was to test the prevailing assumption that split treatment is less costly than integrated treatment.
Methods
Design
Differences in the use and cost of behavioral health services were examined using a quasi-experimental design that compared patients in integrated treatment with those in split treatment. All patients (N=1,517) began care between January 1, 1995, and December 31, 1995. Information about utilization and costs of behavioral health services was extracted from the claims records for all treatment episodes occurring in the subsequent 18 months. The care was managed by U.S. Behavioral Health (USBH), a national specialty managed behavioral health company headquartered in San Francisco. The name of the company was changed to United Behavioral Health in January 1997.
Patients were between the ages of 18 and 65 and were diagnosed as having a depressive disorder—major depression, dysthymia, depressive disorder not otherwise specified, or mood disorder not otherwise specified—by the treating clinician sometime during their index treatment episode. If bipolar disorder, schizophrenia, or a psychotic disorder was also documented, the patient was excluded from the study under the assumption that depression was a phase of the disorder rather than a concomitant condition.
Data source
The study is based on data on use and costs recorded in the USBH claims data system for all members in the company's behavioral health carve-out plans offered by private and public employers nationwide. Excluded were members whose only benefits were services provided by employee assistance programs. All care was reimbursed on a fee-for-service basis.
Patients in the study followed the same referral pattern as other USBH patients. Patients request services via telephone, and they are referred to a network clinician based on clinical need and geographic accessibility, as well as the patient's personal and cultural preferences. Clinical needs are addressed by matching patients' presenting problems and symptoms with clinicians' specialties and availability. Clinicians are credentialed by USBH for specific specialties only if their education, training, and experience in the area are sufficiently documented.
Unlike other managed care organizations, USBH tries to directly refer to psychiatrists for both psychotherapy and pharmacotherapy. In 1996 the USBH network had approximately 35,000 mental health specialists; 19 percent were psychiatrists, 36 percent were doctoral-level clinical psychologists, 30 percent were clinical social workers, and 15 percent were master's-level counselors. Data from a recent survey of 5,000 USBH network psychiatrists and their practice patterns were compared with data from members of the American Psychiatric Association (APA) in clinical practice (Goldman W, Penner S, Matevia M, unpublished manuscript, 1997). The USBH network is similar in gender distribution to the APA membership, but psychiatrists in the network are younger; psychiatrists are overrepresented in the California network and underrepresented in New York and the mid-Atlantic states.
For the study reported here, utilization of services was computed as the number of medication management sessions and psychotherapy sessions. Utilization was also computed as the number of separate treatment episodes; an episode of treatment was defined as a period of continuous treatment without a break longer than 90 days.
The cost of services was estimated as all payments made by USBH for a patient with a diagnosis of depression, as well as the copayments made by the patient for behavioral health services. Costs were broken down in several ways: total costs, costs for psychotherapy sessions, costs for medication management visits, and costs for intensive services, which included inpatient, residential, and day treatment. USBH claims data do not include the use and cost of pharmaceuticals because they are covered under the patient's medical benefit. Therefore, costs of medications are not included in this study.
Additional diagnoses for a patient that suggested comorbidity were also noted for each episode of care. Comorbidity, utilization of intensive services (inpatient, residential, and day treatment), and the presence of suicidal ideation at the time patients first requested services were also included as indicators of severity of illness. Demographic information included patients' sex and age, as well as their relationship to the subscriber covered by the employer's benefit plan.
Integrated and split treatment
Patients were retrospectively classified into two cohorts—integrated treatment or split treatment—based solely on the services they received. Patients who saw only a psychiatrist for both psychotherapy and medication sessions were identified as having received integrated treatment (N=191). Patients who saw a psychiatrist for medication sessions and a nonphysician mental health specialist for psychotherapy were identified as having received split treatment (N= 1,326). Some patients (N=179) fit neither treatment pattern because they received treatment from a psychiatrist and a psychotherapist sequentially and not simultaneously. This group was excluded from the study.
Statistical analysis
Ordinary least-squares regression was used to compare the integrated- and split-treatment cohorts on units of service and treatment costs, controlling for demographic characteristics and comorbid diagnostic conditions. Group membership was dummy coded 1 for integrated treatment and 0 for split treatment. Comorbid conditions such as anxiety disorders, substance use disorders, suicidal ideation, and major depression with psychotic features were similarly dummy coded.
Preliminary examination indicated a nonnormal distribution of costs and units of service. Therefore, costs and units of service were modeled as a function of their natural log-transformed values. Examination of residual plots suggested normal distribution of errors and homogeneity of variance across predicted values (df=10, 1,461 for the regression models). Tests were based on a two-tailed t test that the beta coefficient for integrated treatment was different from zero. A .05 significance level was used for all statistical tests.
All estimates presented here on the use and costs of integrated and split treatment were computed as the mean value for each group adjusted for differences in patients' characteristics. Adjusted means were transformed from a log scale using a nonparametric transformation method known as the smearing estimate (32).
Results
Demographic characteristics
Characteristics of patients in both the integrated- and the split-treatment cohorts are presented in Table 1. The distribution of gender within the two cohorts differed, with females accounting for a higher percentage of the split-treatment cohort. The split-treatment cohort also had a higher percentage of younger patients. The distribution of employees and dependents was similar in both cohorts, with employees accounting for more than two-thirds of the sample. The integrated-treatment cohort had a somewhat larger proportion of individuals with a comorbid diagnosis of major depression with psychotic features.
Treatment characteristics
Table 2 presents the treatment characteristics of the two groups. In the split-treatment cohort, the adjusted mean number of sessions for both medication sessions and psychotherapy sessions was significantly higher than for the integrated cohort.
In the 18-month study period, no difference was found between cohorts in the mean length of a treatment episode (defined as the time between the first date of service and a break in services of 90 days or more). However, we detected differences between groups in the pattern in which sessions were used. A total of 129 patients in the integrated-treatment group (68 percent) had breaks in treatment of 90 days or more, compared with 754 patients in the split-treatment group (57 percent; c2= 7.82, df=1, p<.005). Thus the integrated-treatment cohort had a larger mean number of episodes per patient (2.22 episodes versus 1.55).
At 18 months after the first date of service, a higher percentage of patients in the integrated-treatment cohort were still in active treatment compared with the split-treatment group (107 patients, or 56 percent, versus 490 patients, or 37 percent; c2=25.43, df=1, p<.001). These findings suggest that patients in integrated treatment received treatment intermittently over a longer period than did patients in the split cohort.
Costs
Costs of outpatient services are a function of the number of sessions and the type of clinician providing services because USBH pays its network clinicians using a national rate based on the clinician's license type. The contracted rate for psychiatrists is $95 per 50-minute session and $47.50 for a 20- to 25-minute medication monitoring session, while the contracted rates for nonphysician clinicians (clinical psychologists, social workers, and master's-level clinicians) average $68 for a 50-minute session. The patient's copayment or coinsurance per session depends on the benefit design and may increase with the number of sessions. It is not dependent on the type of provider seen.
The adjusted mean cost of outpatient services was significantly lower in the integrated-treatment cohort, $868 versus $1,465. Despite a higher adjusted mean cost of intensive services in the integrated-treatment cohort ($447 versus $220), the adjusted mean cost for all services was still significantly lower in the integrated-treatment cohort ($1,336 versus $1,854).
Discussion
The prevailing assumption in public and private organized care systems is that split treatment is less costly than integrated treatment in which prescribing psychiatrists also deliver psychotherapy. This assumption was contradicted in our analyses of more than 1,500 providers seeing patients with a diagnosis of depression in a carve-out managed behavioral health care setting. Instead, data indicated that costs were lower when medication management and psychotherapy were delivered by a single psychiatrist and that the lower cost was primarily due to the reduced number of sessions used by patients in integrated treatment. Furthermore, integrated treatment appeared to be associated with a pattern of utilization characterized by frequent treatment episodes in contrast to that of split treatment, which was characterized by more sessions with fewer breaks of 90 days or more.
Numerous possible explanations can be offered for the findings that individuals with depression who received integrated treatment differed in their treatment utilization patterns. For instance, differences could exist in how efficiently these services are provided. If patients in the integrated treatment group regularly received medication and psychotherapy services during the same visit, the treatment regimen could have the desired effect with fewer total sessions.
Specifically, psychiatrists providing integrated treatment might initiate medication earlier in treatment than those providing split treatment. For example, in integrated treatment the psychiatrist may not require several sessions to convince the patient of the potential efficacy of medication, whereas in split treatment several sessions may be required to convince the patient or the other therapist, or both, of efficacy. Also, in integrated treatment the psychiatrist may rely more on the unfolding effect of the medication and therefore space sessions further apart. In such cases, integrated treatment could result in fewer sessions and thus lower costs even if both treatment modalities are equally effective therapeutically.
If an integrated-treatment strategy is inherently more efficient so that patients stop treatment within a shorter time, they will have fewer outpatient visits. The observed difference in the treatment cohorts could also be due to a lack of coordination of care between the two providers in the split-treatment group, which could result in higher resource utilization (more sessions) and thus more costly episodes of care. Even if under ideal collaborative conditions, the separate medication and psychotherapy interventions are just as effective as those provided in integrated treatment, efficiency with one provider may be greater as indicated by the cost data.
Although this study attempted to adjust for known indicators of illness severity, other characteristics that were not measured, such as psychosocial support and treatment and medical history, may have confounded the comparison of the integrated and split cohorts.
Furthermore, specific characteristics of providers in this setting could help explain the lower number of sessions in the integrated-treatment cohort. A survey by Chiles and associates (5) of mental health providers who saw patients in both integrated and split treatment found that psychiatrists who reported treating patients who were in psychotherapy with someone else were younger, had been in practice fewer years, and were less likely to characterize themselves as psychoanalysts than those who provided integrated treatment. Likewise, psychologists who reported seeing patients in split treatment tended to be younger, to have received their degrees more recently, and to have relatively more extensive clinical practices. However, in the study reported here, characteristics of providers were not measured. Differences in these characteristics might have influenced the results.
Because the study was not randomized, it is likely that a variety of factors led to the differential assignment of patients to integrated and split treatment. Patient preference is one such factor. For example, individuals who are more inclined to use medication might be more likely to request or accept an initial referral to a psychiatrist. Thus they might more easily start on a medication earlier in treatment, if it was clinically appropriate, and several sessions may not be required to convince them or their psychotherapist of the potential efficacy of this approach. This patient group could achieve benefits in fewer sessions. It is also possible that a variety of demographic or other clinical factors, such as marital discord or neurovegetative signs in older patients, could have influenced the assignment process in a way that was not measured.
Censoring of data is also a possibility in this study. Censoring occurs when a clinician withholds diagnostic information from the payer. Also, some individuals might have not been correctly classified by treatment cohort because of a lack of medication treatment information in the database. For example, individuals who were classified as receiving psychotherapy only, based on claims data, might have been receiving medication from a physician outside the health care system, and thereby be receiving split treatment. Similarly, if a psychiatrist conducted integrated treatment but billed only for psychotherapy sessions, those episodes of care could not be identified as integrated treatment and were not included in this analysis. It is not clear how the inclusion of such individuals would have affected the results.
Finally, given the nature of the data source, an administrative claims database, it was not possible to validate the diagnosis of depression. Thus we were unable to assess whether systematic differences existed in how patients in each treatment group were diagnosed.
Although this study examined the effects of integrated psychotherapy and pharmacotherapy versus split treatment on health care utilization, ultimately the more important question is the effectiveness of different models of treatment for different groups of patients. Research should address the questions of which patients benefit most from which treatment models, including the broadly conceptualized models of integrated versus split treatment. A better understanding of the qualitative differences between the two models of treatment and how the two models are structured might help explain the observed differences. Some evidence exists for the suggestion that subtypes of patients with depression might benefit selectively from different treatment strategies (33), and given the controlled nature of managed care settings, different factors related to health systems must be taken into account. We see no barrier to a randomized research design to further study these issues.
The long-standing debate over long-term intermittent psychotherapy versus long-term continuous psychotherapy, with or without pharmacotherapy, might be usefully informed by further study. Are psychiatrists continuing to do effective psychotherapy during brief medication monitoring sessions? Research has investigated the usefulness of cognitive-behavioral and interpersonal psychotherapy in the treatment of depression. What psychiatrists are actually practicing, however, is not known. The question of dose-response also remains unanswered. Is the finding of fewer sessions provided to the integrated therapy cohort due to efficiency or undertreatment in some cases? Further research needs to be done on how to distinguish enough treatment from undertreatment or overtreatment.
Conclusions
This study was undertaken to discover if there is any economic validity to the common practice in organized care settings of splitting psychotherapy and pharmacotherapy. We wanted to test whether it was practical to see one clinician for certain problems instead of two. That was and remains the central point of this analysis.
The results offer economic evidence supporting our clinical belief that having some patients see one therapist for consolidated treatment is more efficient. However, only 13 percent of the USBH patients in this study received such integrated treatment. Even at USBH, where using psychiatrists for both psychotherapy and pharmacotherapy of depression is encouraged, we found that many factors may conspire to continue to split treatment.
It remains to be seen why split treatment remains the prevalent form of care. How much is it due to patient expectations or preferences? To what extent are assumptions in the current professional culture about the cost-effectiveness of split treatment embedded in the beliefs of in-house intake counselors and care managers, who themselves are clinical professionals? To what extent do psychiatrists' practice patterns, which often restrict their availability, affect prevailing forms of care? Have the economics of the new health care delivery systems created differential practice patterns wherein psychiatrists provide pharmacotherapy for managed care referrals only and psychotherapy for other patients? How many psychiatrists prefer not to do psychotherapy—or pharmacotherapy—because of their age, inclinations, training, or practice setting? If some of these factors are verified to be pertinent, are they modifiable through education or incentives?
Because medication and psychotherapy play central roles in the scientifically based treatment of depression, these preliminary findings, while not definitive, are suggestive and should be followed up. Splitting psychotherapy and pharmacotherapy is a practice and a point of view that has in effect been legislated without evidence. For all its limitations, this study contradicts the pervasively held belief that split treatment is more cost-effective. The strength of the preliminary findings poses a powerful challenge and invites serious investigation and further study. We hope that this study is only one in a series of long-awaited benefits to be realized by the development of unprecedentedly comprehensive data sets by the new national managed care industry that can be used to help us learn to take better and more cost-effective care of our patients.
Acknowledgments
The authors acknowledge the excellent consultations provided by Robert Michels, M.D., James Sabin, M.D., Herbert Schlesinger, Ph.D., Richard Smith, M.D., Roland Sturm, Ph.D., and Kenneth Wells, M.D.
Dr. Goldman, Ms. McCulloch, and Dr. Cuffel are with United Behavioral Health, 425 Market Street, 27th Floor, San Francisco, California 94105-2426 (e-mail, [email protected]). Dr. Zarin and Ms. Suarez are with the office of research of the American Psychiatric Association; however, the views expressed in this article do not necessarily represent those of the association. Dr. Burns is with Duke University Medical Center in Durham, North Carolina.
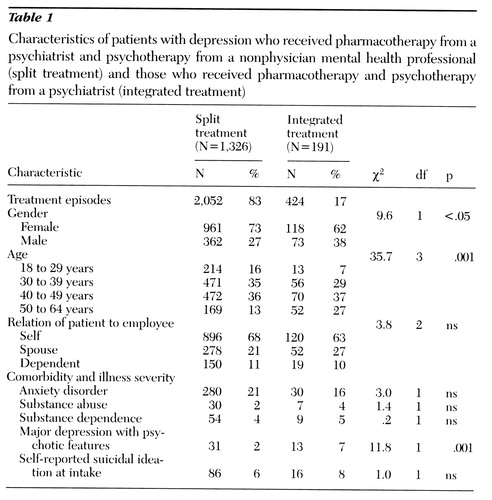 |
Table 1. Characteristics of patients with depression who received pharmacotherapy from a psychiatrist and psychotherapy from a nonphysician mental health professional (split treatment) and those who received pharmacotherapy and psychotherapy from a psychiatrist (integrated treatment)
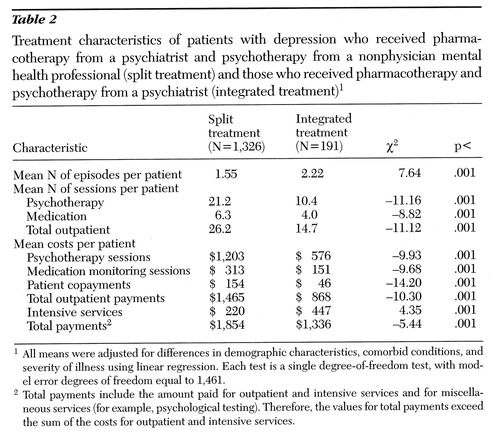 |
Table 2. Treatment characteristics of patients with depression who received pharmacotherapy from a psychiatrist and psychotherapy from a nonphysician mental health professional (split treatment) and those who received pharmacotherapy and psychotherapy from a psychiatrist (integrated treatment)
1. Racy J: Combined therapy. Harvard Mental Health Letter 13(2):5-6, 1996Google Scholar
2. Pilette WL: The rise of the three-party treatment relationship. Psychotherapy 25:420-423, 1988Crossref, Google Scholar
3. Bradley SS: Nonphysician psychotherapist-physician pharmacotherapist: a new model for concurrent treatment. Psychiatric Clinics of North America 12:307-323, 1990Google Scholar
4. Sullivan M, Verhulst J, Russo J, et al: Psychotherapy vs pharmacotherapy: are psychiatrists polarized? A survey of academic and clinical faculty. American Journal of Psychotherapy 47:411-423, 1993Crossref, Medline, Google Scholar
5. Chiles JA, Carlin AS, Benjamin GA, et al: A physician, a nonmedical psychotherapist, and a patient: the pharmacotherapy-psychotherapy triangle, in Integrating Pharmacotherapy and Psychotherapy. Edited by Beitman BD, Klerman GL. Washington, DC, American Psychiatric Press, 1991 Google Scholar
6. Goldberg RS, Riba M, Tasman A: Psychiatrists' attitudes toward prescribing medication for patients treated by nonmedical psychotherapists. Hospital and Community Psychiatry 42:276-280, 1991Abstract, Google Scholar
7. Appelbaum PS: General guidelines for psychiatrists who prescribe medication for patients treated by nonmedical psychotherapists. Hospital and Community Psychiatry 42:281-282, 1991Abstract, Google Scholar
8. Goodman A: Psychodynamics in pharmacotherapy: practical application. Psychiatric Times, Nov 1995, pp 54-55Google Scholar
9. Lazarus J, Macbeth J, Wheeler N: Divided treatment in the managed care arena: legal and ethical risks. Psychiatric Practice and Managed Care 3(2):3-10, 1997Google Scholar
10. Sederer LI: The four questions, in Acute Care Psychiatry: Diagnosis and Treatment. Edited by Sederer LI, Rothschild AJ. Baltimore, Williams & Wilkins, 1997Google Scholar
11. Busch FN, Gould E: Treatment by a psychotherapist and a psychopharmacologist: transference and countertransference issues. Hospital and Community Psychiatry 44:772-774, 1993Abstract, Google Scholar
12. Rush AJ, Hollon SD: Depression, in Integrating Pharmacotherapy and Psychotherapy. Edited by Beitman BD, Klerman GL. Washington DC, American Psychiatric Press, 1991Google Scholar
13. Blackburn IM, Bishop S, Glen AIM, et al: The efficacy of cognitive therapy in depression: a treatment trial using cognitive therapy and pharmacotherapy, each alone and in combination. British Journal of Psychiatry 139:181-189, 1981Crossref, Medline, Google Scholar
14. Blackburn IM, Eunson KM, Bishop S: A two-year naturalistic follow-up of depressed patients treated with cognitive therapy, pharmacotherapy, and a combination of both. Journal of Affective Disorders 10:67-75, 1986Crossref, Medline, Google Scholar
15. Frank E, Kupfer DJ: Efficacy of combined imipramine and interpersonal psychotherapy. Psychopharmacology Bulletin 23:4-7, 1987Medline, Google Scholar
16. Frank E, Kupfer DJ, Perel JM, et al: Three-year outcomes for maintenance therapies in recurrent depression. Archives of General Psychiatry 47:1093-1099, 1990Crossref, Medline, Google Scholar
17. Friedman AS: Interaction of drug therapy with marital therapy in depressed patients. Archives of General Psychiatry 32:619-637, 1975Crossref, Medline, Google Scholar
18. Friedman ES: Combined therapy for depression. Journal of Practical Psychiatry and Behavioral Health 3:211-222, 1997Google Scholar
19. Hollon SD, Shelton RC, Loosen PT: Cognitive therapy in relation to pharmacotherapy for depression. Journal of Consulting and Clinical Psychology 59:88-99, 1991Crossref, Medline, Google Scholar
20. Kelly KV: Parallel treatment: therapy with one clinician and medication with another. Hospital and Community Psychiatry 43:778-780, 1992Medline, Google Scholar
21. Klerman GL, DiMascio A, Weissman MM, et al: Treatment of depression by drugs and psychotherapy. American Journal of Psychiatry 148:345-350, 1991Link, Google Scholar
22. Klerman GL, Weissman MM: Interpersonal psychotherapy (IPT) and drugs in the treatment of depression. Pharmacopsychiatry 20:3-7, 1987Crossref, Medline, Google Scholar
23. Manning DW, Frances AJ: Combined therapy for depression: critical review of the literature, in Combined Pharmacotherapy and Psychotherapy for Depression. Edited by Manning DW, Frances AJ. Washington, DC, American Psychiatric Press, 1990Google Scholar
24. Munoz RF, Hollon SD, McGrath E, et al: On the AHCPR depression in primary care guidelines. American Psychologist 49:42- 61, 1994Crossref, Medline, Google Scholar
25. Weiner HK, Riba MB: Medication backup: attitudes and practices of psychiatrists and residents. Psychiatric Services 48:536-538, 1997Link, Google Scholar
26. Weissman MM, Prusoff BA, DiMascio A, et al: The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. American Journal of Psychiatry 136:555-558, 1979Medline, Google Scholar
27. Weissmann MM, Klerman GL, Prusoff BA, et al: Depressed outpatients: results one year after treatment with drugs and/or interpersonal psychotherapy. Archives of General Psychiatry 38:51-55, 1981Crossref, Medline, Google Scholar
28. Wells KB, Sturm R, Sherbourne C, et al: Caring for Depression. Cambridge, Harvard University Press, 1996Google Scholar
29. Wexler BE, Cicchetti DV: The outpatient treatment of depression; implication of outcome research for clinical practice. Journal of Nervous and Mental Disease 180:277- 286, 1992Crossref, Medline, Google Scholar
30. Woodward B, Duckworth GS, Gutheil TG: The pharmacotherapist-psychotherapist collaboration, in American Psychiatric Press Review of Psychiatry. Edited by Oldham JM, Riba MG, Tasman A. Washington, DC, American Psychiatric Press, 1994Google Scholar
31. Conte HR, Plutchik R, Wild KV, et al: Combined psychotherapy and pharmacotherapy for depression. Archives of General Psychiatry 43:471-479, 1986Crossref, Medline, Google Scholar
32. Duan N: Smearing estimate: a nonparametric retransformation method. Journal of the American Statistical Association 78:605- 610, 1983Crossref, Google Scholar
33. Current status of psychosocial treatment research, in Psychosocial Treatment Research in Psychiatry: A Task Force Report of the APA. Washington, DC, American Psychiatric Association, 1993Google Scholar



