Comparative Use of Biomedical Services and Traditional Healing Options by American Indian Veterans
Abstract
OBJECTIVE: This study described service use among American Indian veterans, compared use patterns across biomedical care and traditional healing options, and tested whether utilization varied as a function of need or availability. METHODS: A cross-sectional survey of 621 male combat veterans selected from tribal rolls was conducted between 1992 and 1995 in American Indian reservation communities in the Southwest and in the Northern Plains. Measures included assessments of demographic characteristics, physical and mental health conditions, and self-reports of any use during the past year of Veterans Administration (VA), Indian Health Service (IHS), and other biomedical services as well as participation in traditional ceremonies and use of indigenous healing options. RESULTS: Tribal groups were similar in sociodemographic characteristics and in number of health problems and mental and substance use problems during the past year. The same types of services from IHS were available to the two groups, and the geographic distance to these services was similar. VA facilities were more readily available in the Northern Plains than in the Southwest, where they were far from reservation boundaries. Use of IHS services was similar for the two tribal groups, but use of VA services was significantly less in the Southwest. Overall, biomedical services were used more in the Northern Plains, reflecting greater use of VA facilities. However, these differences in overall health service disappeared when traditional healing options were considered. Use of traditional healing was greater in the Southwest, offsetting lower biomedical service use. CONCLUSIONS: When the full array of options is examined, service use functions according to need for health care, but the kind of services used varies according to availability.
In the growing body of research on alternative or complementary health services, little information is available about their overlap with biomedical services (1,2,3). Furthermore, almost no information is available about how geographic availability or cultural traditions affect patterns of such service utilization (4). Yet these services are especially important among American Indians, for whom traditional healing activities are often a significant element of family, community, and spiritual life (5,6,7,8).
This paper examines patterns of service use across biomedical and traditional healing options among male American Indian veterans of the Vietnam War, a group known to experience substantial chronic physical, emotional, and alcohol problems (Beals J, Holmes T, Ashcraft M, et al, unpublished manuscript, 2000). It includes data on the combined and differential use of biomedical and traditional healing options. Our primary research question was to determine whether service use is simply a function of need or is driven primarily by availability, regardless of form.
Methods
Study design and sample
A cross-sectional survey was designed to replicate the 1987-1988 National Vietnam Veterans Readjustment Study (NVVRS) (9,10,11). NVVRS identified higher rates of posttraumatic stress disorder (PTSD) among African-American and Hispanic veterans than among white veterans. In 1990 Congress mandated an NVVRS-like investigation to collect prevalence data for other minority groups, including American Indians. The ensuing American Indian Vietnam Veterans Project (AIVVP), conducted between 1992 and 1995, followed procedures approved by institutional review and councils of participating tribes (Beals J, Holmes T, Ashcraft M, et al, unpublished manuscript, 2000).
AIVVP samples were recruited from two distinct tribal groups in the Southwest and in the Northern Plains. To protect community confidentiality these tribes are not named (12), but they can be described generally. The Southwest sample was drawn from one of the largest reservations in the United States. Although about 150,000 people live on the reservation, population density is only six people per square mile, compared with the national average of 60. Unemployment is very high (13).
The Northern Plains sample was drawn from three closely related reservation communities. These communities represent a combined geographic area of several thousand square miles and have a combined tribal enrollment of about 48,000. The area is rural and is economically disadvantaged. More than 50 percent of the population on each reservation meet poverty criteria.
Tribal rolls define the membership of a given tribe. Samples were drawn equally from these rolls from Northern Plains and Southwest groups. Veteran status was obtained from state and tribal records and verified in an interview. Only Vietnam veterans were eligible, and only those living on or within 50 miles of the reservation were selected. Samples were limited to men, since few women from these communities served in Vietnam. Only persons born between 1930 and 1958 were selected; this group encompassed over 95 percent of the men who served during the Vietnam era.
In the Southwest, this selection procedure produced a sampling frame from which potential respondents were chosen at random. In the Northern Plains reservations, it produced our study sample, which included all available veterans. A total of 316 Southwest and 305 Northern Plains veterans completed interviews. At each site, more than 90 percent of those selected were located, and more than 90 percent of those located agreed to participate. The overall response rate was 80 percent. Analyses are weighted to reflect sampling in the Southwest and to adjust for missing data in both tribal groups. Detailed weighting information is available for the authors.
Interviews were administered by trained lay staff using the same procedures for both tribal groups (14). The instrument assessed personal characteristics, physical and mental health status, and service use.
Health measures and service use measures
Health measures. Mental health status was based on DSM-III-R (15) criteria and included mental and substance use disorders. Substance use conditions were assessed using a form of the Composite International Diagnostic Interview (CIDI) adapted for use in the National Comorbidity Study (NCS) (16). We reviewed the NCS-CIDI in focus groups of veterans, families, and providers from the Southwest and the Northern Plains, making modifications only when items were incomprehensible or culturally inappropriate. Our analyses considered DSM-III-R diagnoses made within the 12 months preceding the interview.
To assess physical health, we asked veterans if they currently experienced any of 15 health conditions. The health conditions were selected because they are prevalent on these reservations and have important implications for service use.
Service use measures. The service ecology on reservations is complex and warrants description. Three main sources of care are available for biomedical care of mental and physical health problems: the Veterans Administration (VA), which offers outpatient and hospital care; the Indian Health Service (IHS), which also offers clinical and hospital care (17); and other providers, including off-reservation private facilities and tribal substance abuse programs (6). Mental health services provided by these facilities incorporate many approaches in addition to biomedical services; the term "biomedical" is meant here only to describe services offered in the context of hospital and outpatient care.
Availability, accessibility, and affordability vary among the services. VA care is limited to service-related disabilities and is priced according to disability. In the Southwest, the nearest VA outpatient clinic is 20 miles from the easternmost reservation border, but the nearest VA hospital and specialty services are located in urban areas 180 miles and 265 miles away, respectively. Trips to these facilities from the center of the reservation may take more than a day, and they are often complicated by bad weather and lack of transportation.
In the Northern Plains, reservations are smaller in land area and VA services are much closer. Still, the nearest VA facility is 90 miles from a reservation boundary, and reaching it requires a two-hour drive over poor secondary roads.
In contrast, IHS services are similarly available across the Northern Plains and the Southwest. The IHS maintains a hospital on each of the three Northern Plains reservations and several freestanding ambulatory clinics in outlying districts; the large reservation in the Southwest has four IHS hospitals, and another four are available in nearby towns at similar geographic distances (13). IHS services are also available without cost to all tribally enrolled American Indians.
Private care is available only to off-reservation communities, and costs are generally prohibitive for groups with low incomes, high unemployment, and few insurance benefits. At the time of this study, tribal health programs were inconsequential.
American Indian communities have a rich history of traditional care through consultation with medicine men and ceremonies. Costs associated with traditional care can be high, running to thousands of dollars, and no insurance policies cover this care. Although reimbursements for ceremonies are now possible through VA under special circumstances, at the time of this study such coverage was not available. Family members often contribute to the cost of ceremonies, which are likely to involve family and community members. Time is also a consideration: some ceremonies require a week to perform, and consultations may take hours.
Use of biomedical services was measured separately for VA, IHS, and other biomedical providers, including state and private hospitals, treatment centers or clinics, and private physicians. For each provider group, participants were asked whether they had been hospitalized in the provider's facility within the past 12 months and whether they had gone to the provider for outpatient or clinical care for a physical health problem within the past six months. They were then asked whether they had received help from the provider for personal problems, problems with alcohol or drugs, or emotional problems from the war. The 12-month and six-month time frames were chosen to correspond to NVVRS questions about VA service use.
Traditional healing was assessed similarly. Respondents were asked whether they had gone to a medicine man or traditional healer or had a ceremony for a physical health problem within the past six months and whether they had used these sources within the past 12 months for help with personal problems, problems with alcohol or drugs, or problems from the war.
We present analyses of current health service use, which means any hospitalization at a VA, IHS, or other inpatient facility within the past year; any VA, IHS, or other outpatient facility used within the past six months; any traditional healing option used for physical health problems within the past six months; and any traditional option used for personal or alcohol problems or problems from the war within the past year.
Analysis
Analytic aims. We had three analytic aims. The first was to examine overall levels of service use, stratified by service sector and tribal group. The second was to describe comparative patterns of use among biomedical and traditional healing systems. The third was to explore variations in patterns of use across systems of care that are differentially available to the two tribal groups.
Hypotheses. By design, veterans in our study were demographically similar and were similarly eligible for services through VA and IHS. However, VA services were more readily available to Northern Plains veterans. Accordingly, we expected differences in patterns of service use. We tested four a priori hypotheses about biomedical care.
We first hypothesized that the use of biomedical services would vary as a function of need. This premise assumed that veterans of the two tribal groups would use biomedical services similarly, given similar needs. Because the availability of VA services is lower in the Southwest, we expected Southwest veterans to make greater use of IHS services to address health care needs.
Alternatively, we hypothesized that biomedical service use would vary as a function of availability. Because the availability of biomedical services differs between the sites, we hypothesized that total biomedical service use would be less in the Southwest, where VA services are less readily available. Under this premise, we expected IHS service use to be the same, given similar health care needs.
Traditional healing options are also available among the possible health care choices. We considered that when traditional options are included, use of particular providers might vary according to availability, and overall service use would operate as a function of health care needs. Hypotheses for combined traditional and biomedical care were also specified.
Our third hypothesis was that overall service use, including use of traditional healing, would vary according to need. We predicted that overall service use would be the same across tribes, given similar needs, when traditional healing options are included among the health care choices.
The fourth hypothesis was that use of all services, including traditional options, would vary as a function of availability. This hypothesis suggests that veterans in the Southwest would make greater use of traditional healing to offset lower biomedical service availability.
Statistical analysis. All analyses were conducted with SAS and SUDAAN, a companion statistical package developed by the Research Triangle Institute to weight for sampling and response bias (18). Utilization rates were evaluated by univariate analysis. We report the percentages that responded affirmatively to service use questions, along with standard errors of the estimates. Service use patterns across systems of care were assessed by first combining all biomedical service use for physical problems, all biomedical service use for mental and substance use problems, and all traditional healing options used for these purposes, and then evaluating associations by cross-tabulation and chi square testing. Service use differences between groups were assessed by t test.
Results
The respondents' mean±SD age was 47.7±3.2 years in the Southwest sample and 46.9±3.8 years in the Northern Plains sample. The groups did not differ significantly in premilitary education or employment, length of military service, military branch, place of service in Vietnam, or postmilitary hospitalizations. They were also similar in current employment and number of children, although Southwest veterans were more likely to be married. Cultural affiliation—the measured practice of American Indian traditions, language, and ways of life—was similarly high in both groups.
Veterans in both groups reported substantial rates of health problems (Table 1), particularly hypertension, respiratory ailments, diabetes, heart trouble, and arthritis. Self-reported physical condition was generally similar for the two groups, except that Northern Plains veterans reported significantly more cirrhosis. No significant tribal differences were found in the number of health conditions or in the proportion of veterans with a health problem. On average, veterans reported three current physical health conditions.
Psychiatric disorders were evaluated for the 12 months preceding the interview and included assessments for mood and anxiety disorders and substance dependence (Table 2). Posttraumatic stress disorder (PTSD) was assessed by administration of the CIDI and several other question sets related to symptoms. A subset of the sample received a SCID interview. SCID and composite diagnoses for PTSD that combined diagnostic measures and symptom scales have been given in other published reports of the AIVVP study. We chose to limit this investigation to CIDI-based diagnoses for the purpose of comparison with other diagnoses and to make use of the full sample. No significant differences were found between tribes in the proportions of veterans with diagnoses for specific mental disorders or in the number of diagnoses.
The greatest use of services was in the biomedical sector for physical health problems (Table 3). Overall, 46 percent reported that they had used VA, IHS, or other biomedical services within the past year. Although three-quarters of the men in this sample reported having one or more mental or substance use disorders, only 16 percent used biomedical services for mental and substance use problems. The same proportion, 16 percent, had used traditional healing options in the year preceding the interview.
Veterans who used services for mental or substance use problems were also more likely to have seen biomedical providers for physical problems (rate ratio=1.63; p<.001). Veterans who saw biomedical providers for physical problems also used biomedical services for mental or substance use problems more often (rate ratio=2.48, p<.001). Chi square analysis between overall use of traditional healing and biomedical services for either physical or mental or substance use problems showed no significant associations.
Rates of service use for help with physical and mental or substance use problems were examined by provider type, stratified by tribal group (Tables 3 and 4). Utilization rates for mental or substance use problems were substantially lower than rates for help with physical problems.
The next analyses tested hypotheses about differences in use of services (Tables 3 and 4). In the first two hypotheses, we asked whether use of biomedical services varied according to need or availability. We found that Northern Plains veterans, for whom VA facilities were nearer, used significantly more VA services than their counterparts in the Southwest. IHS use was similar for the two tribal groups. The difference between the two groups in overall use of biomedical services was substantial for both physical health and mental or substance use problems. This finding supports the hypothesis that biomedical service use is related to availability rather than need.
The third and fourth hypotheses included traditional healing options in the overall array of services that varied according to need or availability. Our results indicate that traditional options were used more by veterans from the Southwest, where such options are more readily available. However, the differences in overall service use between the two groups disappeared in these analyses, because the greater use of traditional options in the Southwest offset lower VA service use there. This was true for both physical and mental or substance use problems.
Discussion
The significant association between the use of biomedical services for physical and mental or substance use problems among American Indian veterans in our sample is consistent with findings of earlier research. Several population-based and provider studies show substantial use of the general biomedical care sector for mental and substance use problems (16,19,20,21,22,23,24), particularly among those who are poor and those with less education (25).
We also found that a significantly greater proportion of veterans who used biomedical services for physical problems also used biomedical services for mental or substance use problems. This finding is consistent with other research indicating that mental health services are more widely used among people who are in poorer health, have greater functional impairment, or have comorbid physical and mental or substance use conditions (22,26,27).
Rates of use of traditional healing in these samples (16 percent) appears low compared with use of complementary medicine reported in population-based samples in the United States (34 percent) (1), Europe (20 percent to 49 percent) (3), and Australia (49 percent) (2), and a sample of patients in family practice in the U.S. (50 percent) (28). One limitation of our study is that we did not examine the use of alternative care such as acupuncture and chiropractic that was examined in the other investigations. However, concurrent ethnographic work has indicated that these alternatives were not locally available and were unfamiliar to the tribes in the sample. It is also important to note that questions were restricted to the use of traditional healing within the past year for specific physical and mental or substance use problems; we expect that estimates including lifetime use or ceremonies for other purposes would be much larger. Use of traditional healing may also be underreported because of veterans' hesitation to speak of ceremonies designed to resolve problems from the war.
Overall use of health care services may be similarly low in this sample, although 57 percent of Southwest veterans and 61 percent of Northern Plains veterans reported using some form of biomedical service, compared with 65 percent of the sample in the National Comorbidity Study (1).
We found greater use of traditional healing in the Southwest, where the transmission and practice of these methods are more prevalent. This finding is consistent with those of other studies indicating that many people choose alternative or complementary services in keeping with their social networks and belief systems (4).
In American Indian communities, traditional healing and ceremonies long predate biomedical care. Traditional healing is used to address both the physical and spiritual needs of American Indian people, as well as presumed causes of symptoms, such as breaching of taboos, possession, and "soul loss." The current service ecology on these Northern Plains and Southwest reservations incorporates both traditional and biomedical forms and has been described aptly as a "pluralistic system" (6,8).
Two aspects of this ecology are especially important. First, different systems of care are often seen to address different problems. For example, biomedicine may be thought to address physical symptoms, whereas traditional healing addresses the circumstances from which those symptoms arise, such as with taboos. Consequently, different forms of care tend to be seen as complementary to one another but not in conflict (6).
Second, in pluralistic systems, people pursue hierarchies of resort in selecting particular providers. If the first resort does not produce improvement, other systems will be tried until satisfaction is achieved. This selection process has been documented in American Indian communities with demonstrable patterns of selection (6,7,8).
Conclusions
We found that American Indian veterans in this sample used biomedical services differentially, according to availability. This finding is consistent with other research indicating that inaccessibility impedes service use in the biomedical sector (29). However, we also found that when complementary service options were considered, overall service use was similar across groups with similar health care needs, and only the kinds of services used varied according to availability. Had the scope of our inquiry been limited to biomedical service use, this insight would have been suppressed. The question of whether need or availability is the key impetus for service use can be addressed only if future studies consider the full array of health service options, including those perceived to be complementary, alternative, or supplementary to care in the biomedical sector.
Acknowledgments
The National Center for American Indian and Alaska Native Mental Health Research is supported by grant MH-42473 from the National Institute of Mental Health. Funding for the American Indian Vietnam Veterans project was provided by the Department of Veterans Affairs as a supplement to grant MH-42473-06-S1 from the National Institute of Mental Health.
Dr. Gurley and Dr. Novins are assistant professors and Dr. Beals is associate professor with the National Center for American Indian and Alaska Native Mental Health Research of the department of psychiatry at the University of Colorado Health Sciences Center (UCHSC) in Denver. Ms. Jones is an instructor with the Center for Health Services and Policy Research in Denver. Dr. Shore is chancellor of UCHSC and professor in the department of psychiatry. Dr. Manson is professor and head of the division of American Indian and Alaska Native programs in the department of psychiatry at UCHSC. Send correspondence Dr. Novins, University of Colorado Health Sciences Center, NCAIANMHR, Campus Box A011-13, 4455 East Twelfth Avenue, Denver, Colorado 80220 (e-mail, [email protected])
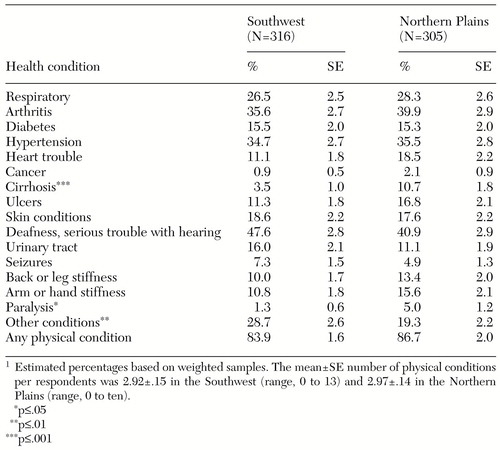 |
Table 1. Physical health conditions in the past year among 621 male Vietnam veterans from American Indian reservation communities in the Southwest and in the Northern Plains
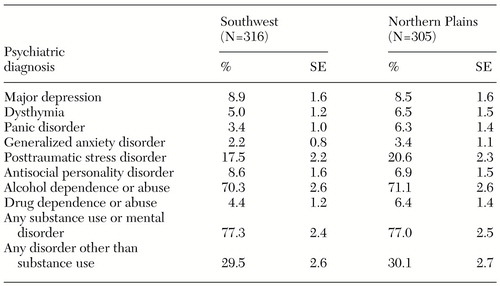 |
Table 2. Psychiatric status in the past year among 621 male Vietnam veterans from American Indian reservation communities in the Southwest and in the Northern Plains
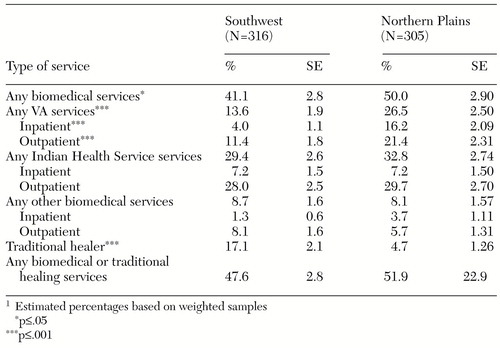 |
Table 3. Use of inpatient care in the past year and use of outpatient care and traditional healing options in the past six months for physical health problems among 621 male Vietnam veterans from American Indian reservation communities in the Southwest and in the Northern Plains
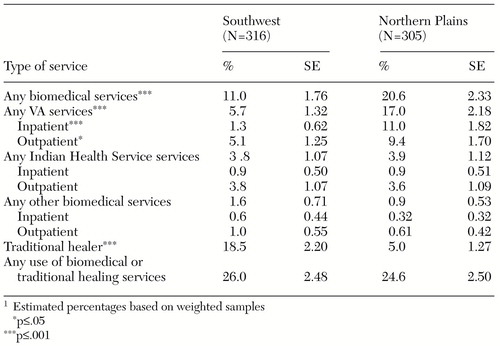 |
Table 4. Use of inpatient care in the past year and use of outpatient care and traditional healing options in the past six months for mental health problems or problems with alcohol or drugs among 621 male Vietnam veterans from American Indian reservation communities in the Southwest and in the Northern Plains
1. Eisenberg DM, Kessler RC, Foster C, et al: Unconventional medicine in the United States: prevalence, costs, and patterns of use. New England Journal of Medicine 328:246-252, 1995Crossref, Google Scholar
2. MacLennan AH, Wilson DH, Taylor AW: Prevalence and cost of alternative medicine in Australia. Lancet 347:569-573, 1996Crossref, Medline, Google Scholar
3. Fisher P, Ward A: Complementary medicine in Europe. British Journal of Medicine 309:107-110, 1994Crossref, Medline, Google Scholar
4. Furnham A, Forey J: The attitudes, behaviors, and beliefs of patients of conventional vs complementary (alternative) medicine. Journal of Clinical Psychology 50:458-469, 1994Crossref, Medline, Google Scholar
5. Harwood A: Guidelines for culturally appropriate health care, in Ethnicity and Medical Care. Edited by Harwood A. Cambridge, Mass, Harvard University Press, 1981Google Scholar
6. Csordas TJ, Garrity JF: Co-utilization of biomedicine and religious healing: a Navajo case study, in Yearbook of Cross-Cultural Medicine and Psychotherapy. Edited by Andritzky W. Berlin, Verlag fur Wissenschaft und Bildung, 1994Google Scholar
7. Guilmet GM: Health care and health care seeking strategies among Puyallup Indians. Culture, Medicine, and Psychiatry 8:349-369, 1984Crossref, Medline, Google Scholar
8. Kunitz SJ, Levy JE: Navajos, in Ethnicity and Medical Care. Edited by Harwood A. Cambridge, Mass, Harvard University Press, 1981Google Scholar
9. Kulka RA, Schlenger WE, Fairbank JE, et al (eds): Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Bruner/Mazel, 1990Google Scholar
10. Jordan BK, Schlenger WE, Hough R, et al: Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Archives of General Psychiatry 48:207-215, 1991Crossref, Medline, Google Scholar
11. Schlenger WE, Kulka RA, Fairbank JA, et al: The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. Journal of Traumatic Stress 5:333-363, 1992Crossref, Google Scholar
12. Norton IM, Manson SM: Research in American Indian and Alaska Native communities: navigating the cultural universe of values and process. Journal of Consulting and Clinical Psychology 64:856-860, 1996Crossref, Medline, Google Scholar
13. Palsano E, Greendeer-Lee J, Cowles J, et al (eds): American Indian and Alaska Native Areas, 1990. Washington, DC, Bureau of the Census, Population Division, Racial Statistics Branch, June 1991Google Scholar
14. Dohrenwend BP: The problem of validity in field studies of psychological disorder revisited, in Validity of Psychiatric Diagnosis. Edited by Robins LN. New York, Raven, 1989Google Scholar
15. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, rev. Washington, DC, American Psychiatric Association, 1987Google Scholar
16. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the US: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
17. Indian Health Care. Report OTA-H-290. Washington, DC, Office of Technology Assessment, 1986Google Scholar
18. Shah BV, Barnwell BG, Bieler GS (eds): SUDAAN. Research Triangle Park, NC, Research Triangle Institute, 1995Google Scholar
19. Olfson M, Pincus HA: Outpatient psychotherapy in the United States: II. patterns of utilization. American Journal of Psychiatry 151:1289-1294, 1994Link, Google Scholar
20. Regier DA, Narrow WE, Rae DS, et al: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry 50:85-94, 1993Crossref, Medline, Google Scholar
21. Manderscheid RW, Rae DS, Narrow WE, et al: Congruence of service utilization estimates from the Epidemiologic Catchment Area Project and other sources. Archives of General Psychiatry 50:108-114, 1993Crossref, Medline, Google Scholar
22. Hough RL, Landsverk JA, Karno M, et al: Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Archives of General Psychiatry 44:702-709, 1987Crossref, Medline, Google Scholar
23. Narrow WE, Regier DA, Rae DS, et al: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Archives of General Psychiatry 50:95-107, 1993Crossref, Medline, Google Scholar
24. Knesper DJ, Pagnucco DJ: Estimated distribution of effort by providers of mental health services to US adults in 1982 and 1983. American Journal of Psychiatry 144:883-888, 1987Link, Google Scholar
25. Alegria M, Robles R, Freeman DH, et al: Patterns of mental health utilization among island Puerto Rican poor. American Journal of Public Health 81:875-879, 1991Crossref, Medline, Google Scholar
26. Olfson M, Pincus HA: Outpatient psychotherapy in the United States: I. volume, costs, and user characteristics. American Journal of Psychiatry 51:1281-1288, 1994Google Scholar
27. Escobar JI, Golding JM, Hough RL, et al: Somatization in the community: relationship to disability and use of services. American Journal of Public Health 77:837-840, 1987Crossref, Medline, Google Scholar
28. Elder NC, Gillcrist A, Minz R: Use of alternative health care by family practice patients. Archives of Family Medicine 6:181-184, 1997Crossref, Medline, Google Scholar
29. Burgess JF, DeFiore DA: The effect of distance to VA facilities on the choice and level of utilization of VA outpatient services. Social Science and Medicine 39:95-104, 1994Crossref, Medline, Google Scholar



