Understanding Social Determinants of Brain Health During Development
Understanding how poverty, systemic racism, and structural inequities impact brain and behavioral development in children and adolescents is crucial to our efforts to prevent the development of psychopathology and to facilitate every child’s ability to thrive. It is now clear that these experiences have long-lasting impacts across the course of an individual’s life and may be carried into subsequent generations. This domain of factors that impact health and well-being in children and adults is often referred to as social determinants of health (SDOH) (1, 2). Historically, efforts to address questions about how SDOH impact child development have been hampered by a variety of factors, including studies with sample sizes too small to allow for powerful explorations of these questions, a lack of diversity and representation in study populations, and the absence of measures of SDOH as well as of brain and behavior in the same study that would allow for an integrated examination. The Adolescent Brain and Cognitive Development (ABCD) Study is providing data that address a number of these challenges, allowing for a more in-depth examination of how SDOH can shape brain development and mental health among children in the United States. The ABCD Study recruited over 11,800 children at ages 9 and 10 and is following them longitudinally for 10-plus years with extensive measures of brain structure and function, behavior, and mental health–relevant constructs. The recruitment approach for the study was designed to generate a sample that was representative of the child population of the United States in terms of gender, race, ethnicity, and socioeconomic status (3). While this goal wasn’t fully achieved, the composition of the ABCD Study is more diverse than the vast majority of studies on brain development. Although not comprehensive, the ABCD Study includes many measures of SDOH, including family income and education; financial adversity; neighborhood financial adversity, social vulnerability, and other characteristics (crime rates, perceptions of safety); exposure to environmental toxins; school characteristics; perceptions and experiences of racism; and state-level measures of gender, race, and ethnicity biases that may be a proxy for structural racism (4, 5).
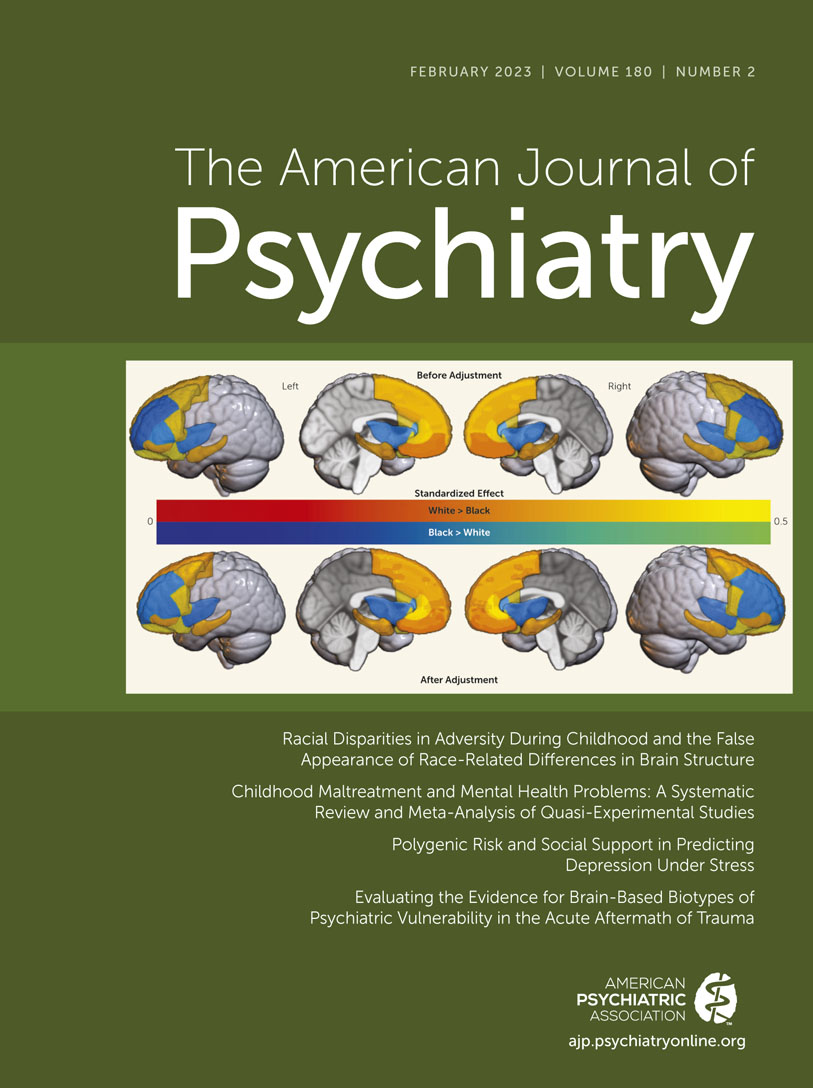
In this issue, Dumornay et al. (6) make use of this rich data set to test the hypothesis that racial disparities in adversity can explain the false appearance of race-related differences in brain structure. To do so, they compare a variety of metrics of brain volume from the baseline ABCD assessment (at ages 9 and 10) in 14 a priori brain regions of interest, primarily in the frontal cortex, cingulate, and insula as well as the hippocampus and amygdala (corrected for intracranial volume), across groups of children whose parents reported that they were White or Black. They then examined whether accounting for a range of SDOH-relevant factors could account for obtained differences in brain structure, including family income, family material hardship, caregiver education, family conflict, neighborhood adversity, estimates of exposure to particulate matter and nitrous oxide, and parent report of childhood trauma. Dumornay et al. found that SDOH metrics were related to many of the same brain regions that also demonstrated differences between the White and Black children. Further, they found that SDOH predictors accounted for up to 51% of the differences between Black and White children in the volume of some brain regions and significantly reduced the size of the race differences in a number of the brain regions, most prominently the superior frontal cortex, the caudal middle frontal cortex, and the inferior frontal gyrus. Dumornay et al. make the highly important point that this pattern of results suggests that toxic stress may account for a significant amount of what is often erroneously interpreted as race differences in brain structure, which they correctly characterize as leading to “false appearances” of race-related difference. This work uses strong analytic methods and a large sample size that allows for a well-powered examination of a range of SDOH factors, and it is grounded in strong theory about the mechanisms by which toxic stress impacts the brain. As such, it is an important step toward understanding how SDOH impact brain development in youths as a potential pathway to risk for mental health challenges.
The aims of the analysis were clearly intended to begin to elucidate and correct the long history of reporting of differences in health, behavioral, and neural outcomes attributed to race and/or ethnicity. These old models generally failed to appreciate and account for the powerful effects of the psychosocial environment on biological processes, including brain development, drawing oversimplified false conclusions about biological differences attributed to race. The negative social effects of these erroneous inferences are obvious and damaging. While Dumornay et al. begin to investigate many key social determinants of neurodevelopment and find important effects, any work framed in terms of race brings with it a high risk of misleading inferences. In particular, the analyses provided in the Dumornay et al. report do not account for numerous key and salient SDOH factors, leaving the reader with the potential impression that race continues to account for brain volume even after considering social factors. This risks the possibility that these remaining race differences could be interpreted in an essentialist framework despite the fact that race is a social construct not explained by biological differences (7). Key SDOH factors not examined by Dumornay et al. that may account for additional variance include 1) a youth’s personal experience of racism, which some have argued is a form of trauma that itself can lead to PTSD (8) and for which emergent data are documenting neural impacts (9); 2) the youth’s experience of serious life events; 3) additional Census-based measures of systemic inequities (i.e., the Child Opportunity Index, the Social Vulnerability Index) (4); 4) measures of state-level indicators of racism and other forms of bias that may also differentially impact youths as a function of their identity (10); 5) school-based factors such as school quality, support, and funding; and 6) factors that may interact with family financial circumstances to increase or decrease risk, such as the cost of living and the generosity of antipoverty programs (11). All but the last set of measures are currently available in the ABCD Study’s Data Release 4.0.
An additional point to note is that Table 3 in the Dumornay article outlines the individual associations between each SDOH metric and each brain region. This table presents results from a linear mixed-effects model, showing the beta weights of the unique contribution of each individual metric over and above the variance shared with other metrics. Given that SDOH factors tend to travel together (i.e., family income tends to be associated with material hardship, both of which are usually correlated with neighborhood disadvantage), the information presented in this table may understate the overall relationship of the SDOH factors examined with the brain metrics, which will include both the shared and the unique relationships. The Dumornay et al. analyses also do not address nonlinear effects and interactions among SDOH facets, an approach that has been used to disentangle social determinants from race showing no additional variance attributable to race beyond SDOH in several key outcomes (12).
When trying to empirically demonstrate how SDOH factors masquerade as the appearance of race differences in brain structure, or any other aspect of brain development or behavior, it is important to ensure that we have as full as possible an assessment of SDOH factors and to consider all of their complex interactions to most completely address this question. Alternatively, we can avoid framing such important work in the context of race differences in brain or behavior and focus directly on how SDOH shape brain, behavior, and mental health risk in far too many youths, while simultaneously recognizing that Black youths in our country and many others face a greater burden of SDOH. We acknowledge that research on SDOH impacts on development also has risks associated with a focus on deficits (13) that could be interpreted through a deterministic lens that does not highlight pathways for resilience and strength. We also acknowledge that because of systemic racism, the experience and impact of many SDOH may differ for individuals with identities that have been the target of inequities. Nonetheless, a more direct focus on SDOH and how these may differentially impact individuals with historically marginalized identities is likely to be a path that helps to avoid reification of what Dumornay et al. aptly term the “false appearance of race-related differences in brain structure.”
1. : Social determinants of health, structural racism, and the impact on child and adolescent mental health. J Am Acad Child Adolesc Psychiatry 2022; 61:1385–1389Crossref, Medline, Google Scholar
2. : Scoping review: national monitoring frameworks for social determinants of health and health equity. Glob Health Action 2016; 9:28831Crossref, Medline, Google Scholar
3. : Ensuring the best use of data: the Adolescent Brain Cognitive Development Study. JAMA Pediatr 2019; 173:809–810Crossref, Medline, Google Scholar
4. : Adolescent Brain Cognitive Development (ABCD) Study Linked External Data (LED): protocol and practices for geocoding and assignment of environmental data. Dev Cogn Neurosci 2021; 52:101030Crossref, Medline, Google Scholar
5. : An update on the assessment of culture and environment in the ABCD Study: emerging literature and protocol updates over three measurement waves. Dev Cogn Neurosci 2021; 52:101021Crossref, Medline, Google Scholar
6. : Racial disparities in adversity during childhood and the false appearance of race-related differences in brain structure. Am J Psychiatry 2023; 180:127–138Link, Google Scholar
7. : Using ethnicity as a classification variable in health research: perpetuating the myth of biological determinism, serving socio-political agendas, or making valuable contributions to medical sciences? Ethn Health 1999; 4:241–244Crossref, Medline, Google Scholar
8. : Racism, posttraumatic stress symptoms, and racial disparity in the US COVID-19 syndemic. Behav Med 2022; 48:85–94Crossref, Medline, Google Scholar
9. : Neural impacts of stigma, racism, and discrimination. Biol Psychiatry Cogn Neurosci Neuroimaging 2022; 7:1225–1234Medline, Google Scholar
10. : Smaller hippocampal volume among Black and Latinx youth living in high-stigma contexts. J Am Acad Child Adolesc Psychiatry 2022; 61:809–819Crossref, Medline, Google Scholar
11. : Antipoverty programs mitigate socioeconomic disparities in hippocampal volume and internalizing problems among US youths. PsyArXiv Preprints, November 30, 2021. https://psyarxiv.com/8nhej/Google Scholar
12. : Disentangling socioeconomic status and race in infant outcomes: a neural network analysis. medRxiv, 2021. https://psyarxiv.com/8nhej/Google Scholar
13. : A biosocial return to race? A cautionary view for the postgenomic era. Am J Hum Biol 2022; 34:e23742Crossref, Medline, Google Scholar