Early Adversity and Development: Parsing Heterogeneity and Identifying Pathways of Risk and Resilience
Abstract
Adversity early in life is common and is a major risk factor for the onset of psychopathology. Delineating the neurodevelopmental pathways by which early adversity affects mental health is critical for early risk identification and targeted treatment approaches. A rapidly growing cross-species literature has facilitated advances in identifying the mechanisms linking adversity with psychopathology, specific dimensions of adversity and timing-related factors that differentially relate to outcomes, and protective factors that buffer against the effects of adversity. Yet, vast complexity and heterogeneity in early environments and neurodevelopmental trajectories contribute to the challenges of understanding risk and resilience in the context of early adversity. In this overview, the author highlights progress in four major areas—mechanisms, heterogeneity, developmental timing, and protective factors; synthesizes key challenges; and provides recommendations for future research that can facilitate progress in the field. Translation across species and ongoing refinement of conceptual models have strong potential to inform prevention and intervention strategies that can reduce the immense burden of psychopathology associated with early adversity.
Adversities that occur early in life, such as maltreatment, exposure to violence, and poverty, are common and can have profound and lasting influences on mental health. Between one-half and two-thirds of youths experience at least one form of adversity or traumatic event prior to adulthood (1–4), and childhood adversity is estimated to play a role in one in three psychiatric disorders in adulthood (4). Youths exposed to adversity are at increased risk for a broad range of internalizing and externalizing problems, including anxiety, depression, posttraumatic stress disorder (PTSD), disruptive behavior disorders, and substance use disorders (2, 4–7). Moreover, early adversity is experienced at higher rates by minoritized communities (8), contributing to mental health disparities (9). Delineating the neurobiological pathways by which early adversity leads to psychopathology is critical for targeted treatment approaches and early risk identification. While research to date in both animals and humans has provided major scientific advances in delineating these pathways, the current state of the science lacks the specificity and mechanistic insight that is essential for reducing the immense burden of psychopathology. In this overview, I review progress and gaps in four promising areas of research, highlight key challenges, and provide recommendations for future directions to advance the field.
MECHANISMS: IDENTIFYING PATHWAYS LINKING EARLY ADVERSITY WITH MENTAL HEALTH
A growing body of research has examined behavioral, cognitive, and neurobiological processes that may explain the robust association between early adversity and risk for psychiatric disorders. Cross-species evidence has demonstrated that early adversity has particularly strong effects on stress physiology (10–12) and corticolimbic neural circuity (13–15) involved in learning about salient aspects of the environment and regulating emotion (16). Indeed, youths exposed to early adversity show alterations in hypothalamic-pituitary-adrenal (HPA) axis function (10, 11, 17, 18) and in both the structure and function of the medial prefrontal cortex (mPFC), amygdala, and hippocampus and their connections (13, 19–23). Connections between these regions may be especially affected by adversity because of their dense expression of glucocorticoid receptors (14, 24–27) and the developmental timing of circuit maturation (14, 15, 28). Whereas prefrontal regions and their connections with limbic structures undergo protracted development, the amygdala matures relatively earlier and may be particularly sensitive to the early social environment (29, 30). Environmental influences on corticolimbic circuitry in early life may play an active role in shaping longer-term neural and behavioral phenotypes, including future responding to adversity. In addition to increasing risk for psychopathology during development, early adversity increases risk of psychopathology following subsequent adversity exposure (31, 32). Emerging evidence suggests that alterations in hippocampal-fronto-amygdala circuitry also underlie effects of stress sensitization (33, 34). Collectively, these studies highlight a central role of corticolimbic circuitry in mediating the effects of early adversity on risk for psychopathology.
Early adversity is also associated with alterations in large-scale brain networks that support cognitive and affective functions (19, 20, 35), such as the salience network involved in detection of behaviorally relevant stimuli (36–40), the frontoparietal network involved in cognitive control (41–46), and the frontostriatal network involved in reward processing (47–53). Paralleling these neural differences, youths exposed to adversity show alterations across a range of domains, including emotion regulation, reward processing, social information processing, and associative learning (20, 54, 55). Despite the potential for resilience and change during development, the effects of adversity can persist long after the adversity ends, and some of the same behavioral and neural alterations have been observed in adults who report exposure to early adversity (21, 56, 57). Given the transdiagnostic nature of disruptions in cognitive control and affective functions, these alterations provide plausible pathways from early adversity to a range of internalizing and externalizing disorders.
Stress Acceleration
While a wealth of studies have demonstrated the effects of early adversity on the brain and stress response systems, a growing literature suggests that early adversity affects the timing or pace of neurobiological development itself (58–61). Life history theory posits that early experiences shape developmental trajectories to meet the environmental demands that individuals are likely to encounter—in the context of a harsh early environment, accelerated pubertal development could be adaptive to prioritize opportunities for reproduction (62, 63). Building on work on life history strategies, predictive adaptive response models suggest that early adversity accelerates biological aging across multiple domains (64, 65). Supporting these ideas, there is cross-species evidence of acceleration in pubertal tempo (66–71), which may be triggered by alterations in endocrine function (17, 66, 72), and cellular aging (73–77) following adversity.
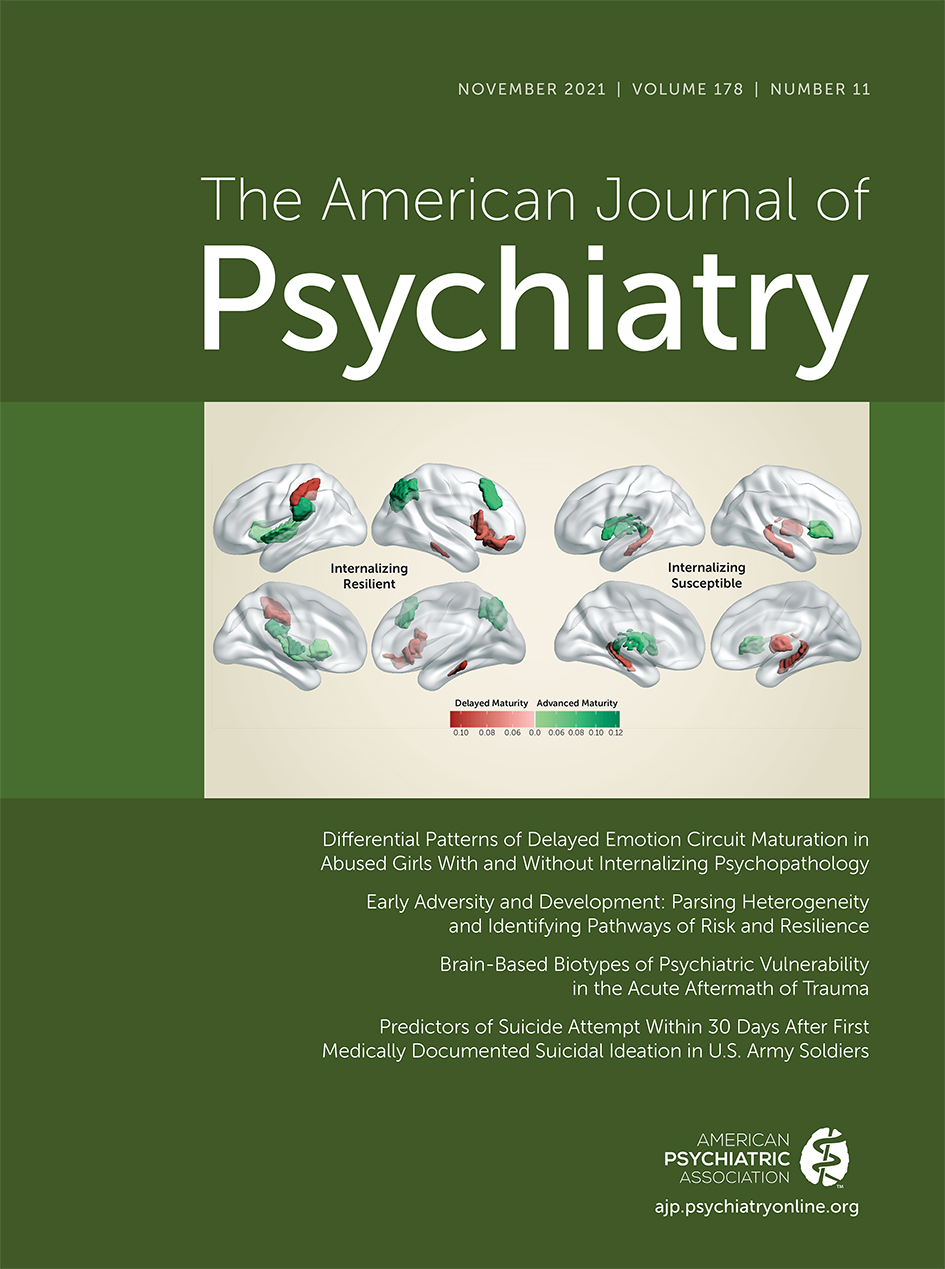
In terms of neurodevelopment, the stress acceleration hypothesis suggests that early adversity leads to precocious maturation of corticolimbic circuitry and behaviors governed by this circuitry, fostering greater capacity for independent regulation of stress and emotion in the absence of a stable, nurturing environment (58). Early adversity has been associated with accelerated maturation of corticolimbic circuitry in both rodents (78–80) and humans (81–86). However, other studies have found evidence of delay or a lack of differences in developmental timing following adversity (59). Recent evidence suggests that some acceleration effects may be specific to corticolimbic circuitry and not to other brain networks (83) and may vary as a function of adversity-related factors. Indeed, a study from Keding and colleagues in this issue of the Journal (87) found that exposure to abuse was associated with delayed structural maturation that was specific to emotion-related neural circuitry, whereas neglect was associated with a more distributed pattern of accelerated structural maturation in female youths.
Although much remains unknown about the function and long-term correlates of shifts in developmental timing, earlier maturation may represent an ontogenetic adaptation (58, 62, 82, 88). Recent work demonstrating acceleration of ventromedial prefrontal cortex (vmPFC)–amygdala connectivity following early adversity found that the more mature pattern of connectivity was associated with slower telomere shortening and slower pubertal tempo (84), suggesting protective neural system effects in the context of accelerated cellular aging following early adversity. Paralleling these findings, children exposed to caregiver deprivation who showed a more mature pattern of vmPFC-amygdala connectivity displayed lower separation anxiety (82), consistent with evidence that stronger inverse amygdala-mPFC functional connectivity is associated with lower internalizing symptoms among youths exposed to early adversity (89). At the same time, there are likely to be long-term consequences of precocious maturation. Future research that examines longer-term effects of accelerated development, tests whether neural findings of acceleration are specific to corticolimbic circuitry, and further examines how developmental timing may converge or diverge across different biological domains will help to provide a more comprehensive understanding of the influences of early adversity on the timing of maturation.
HETEROGENEITY: DIMENSIONAL MODELS OF EARLY ADVERSITY
Despite vast heterogeneity in the nature of early adversity and in developmental outcomes, existing studies have often taken one of several approaches that may obscure meaningful variability. A common study design compares an adversity-exposed group to a non-adversity-exposed group, with the adversity-exposed group comprising individuals exposed to a broad range of adverse experiences (90), or comprising individuals exposed to a single type of adversity (91, 92) without comparison to other types of adversity (13). Another dominant approach has conceptualized adversity in terms of cumulative risk, modeling a continuous measure of adversity exposure as the number of categories of adversity to which an individual has been exposed (93). While such research has contributed foundational knowledge to the field, approaches that focus on specific elements of adversity exposure have the potential to identify key factors that moderate the effects of adversity and to more precisely parse variability in outcomes (13, 88, 94–98). Parsing such variability may be essential for identifying mechanisms and facilitating targeted intervention approaches.
Unpredictability
A robust cross-species literature demonstrates that unpredictability is one important dimension of adversity (88, 99–101), particularly in the context of caregivers’ behaviors. Early caregiving cues, such as the contingency of caregiver responsivity to infants, form the basis of children’s expectations of the environment and are foundational to cognitive and affective development (102, 103) and the development of secure attachment relationships (104). In studies of rodents that manipulate the degree of predictability in maternal care via fragmented care models, rodent pups exposed to unpredictable care show disruption in cognitive and affective processes (99, 101, 105). Alterations in corticolimbic circuitry may underlie these disruptions, as rodents exposed to unpredictable maternal signals exhibit altered amygdala-mPFC connectivity (106), greater amygdala activity (56), and altered corticolimbic interactions that have been associated with anhedonia (107–110).
In humans, unpredictability in parental cues—such as during play with 12-month-old infants (111)—and synchrony in infant-caregiver behavior (112) have similarly been associated with children’s development. Greater unpredictability in broader environmental contexts, such as variability in housing, parental jobs, and parental involvement in care, is associated with risk-taking behavior in adolescence (100). One potential pathway by which broader environmental unpredictability (e.g., variable access to food resources) affects developmental outcomes is through alterations in caregiving behavior (100, 113, 114). Although neural correlates of unpredictability are harder to isolate and have been less explored in humans, recent evidence from a longitudinal study of parent-child dyads demonstrated that higher unpredictability of parental sensory signals at 6 and 12 months of age was associated with greater structural integrity of the uncinate fasciculus at ages 9–11 years, which was associated with episodic memory (115). Future research will be important to better understand the neurobiological correlates of unpredictability in humans and to continue to refine conceptual definitions and facilitate more precise measurement of environmental unpredictability (116).
Threat and Deprivation
Another influential approach draws a distinction between threat (i.e., adversity that involves significant potential for harm, such as abuse or violence) and deprivation (i.e., adversity characterized by the absence of an expected environmental input, such as cognitive or social stimulation, as in neglect or caregiver deprivation) (117, 118). Exposure to threat is associated with alterations in corticolimbic circuitry that include heightened amygdala activation to threat and lower amygdala, mPFC, and hippocampal volumes, with corresponding alterations in aversive learning and emotion processing (35, 119–125). By contrast, some evidence suggests that deprivation is more consistently associated with lower gray matter volumes and altered function in frontoparietal regions (41, 126), and with difficulties in executive functioning and language (127–131). However, deprivation in the form of previous institutionalization has also been associated with alterations in corticolimbic circuitry, including altered amygdala volume, amygdala-mPFC connectivity, and amygdala reactivity (82, 91, 132, 133), as well as alterations in aversive learning and emotion processing (86, 134, 135). In light of some inconsistent findings and challenges in modeling threat and deprivation (136, 137), ongoing research will be helpful to continue to inform how these elements may differentially influence development, including research that examines threat or deprivation while controlling for the other in the same study (130, 138–141). Taken together, various empirical and theoretical contributions to the field (13, 88, 94–97, 100, 137) highlight the value of delineating specific elements of early adversity to further advance knowledge of mechanisms and developmental trajectories.
TIMING: SENSITIVE PERIODS AND DEVELOPMENTAL EFFECTS
Given changes in neuroplasticity, and given that the neural circuitry sensitive to adversity undergoes dynamic changes from the prenatal period through young adulthood, the effects of adversity are likely to vary as a function of the developmental stage at which adversity occurs (13–15, 28, 142). Across species, evidence demonstrates that adversity that occurs early in life has particularly strong effects on neurobiological and psychiatric outcomes relative to adversity that occurs in adulthood (14, 143). Even during development, effects are likely to differ as a function of the specific timing of adversity exposure (e.g., infancy, early versus late childhood, early versus late adolescence, etc.). Animal work that allows for manipulating the timing of exposure shows that the effects of adversity differ as a function of developmental timing (14, 144). Manipulating adversity exposure is challenging in humans; however, naturalistic human studies of adversity provide converging evidence that outcomes depend on the timing of adversity (11, 21, 28, 94, 145–148).
Sensitive Periods
One important way in which the timing of adversity relates to developmental trajectories is through sensitive periods of heightened neuroplasticity, when a specific species-expected environmental input has a particularly strong influence on a specific brain circuit (149, 150). While sensitive-period phenomena are challenging to study in humans, the unique study design of the Bucharest Early Intervention Project (151) has provided insight into a potential sensitive period related to caregiving and socioemotional development during the first 2 years of life. Findings suggest that youths exposed to caregiver deprivation via institutionalized care show more secure attachment, more normative stress responses, and more normative neurodevelopmental trajectories following placement into a foster care intervention prior to 24 months of age, relative to peers who were placed after 24 months of age (11, 152, 153). However, it remains unclear whether earlier placement into foster care is associated with more favorable outcomes because of a shorter duration of stress or because the stress may interact with plasticity, or both.
Consistent evidence has shown that the absence of stable, nurturing caregiving in the postnatal and infancy period disrupts corticolimbic development. Across species, early caregiver deprivation is associated with altered connectivity between the amygdala and mPFC in mice (154), rats (155), nonhuman primates (156), and humans (82). These findings may reflect a sensitive period driven by experience-expectant mechanisms. Consistent with criteria for a sensitive period (150, 157), it is likely that this period is marked by heightened neuroplasticity, and infancy is a time of rapid and substantial change in corticolimbic circuitry (158). There is also some specificity to the nature of the experience and the timing of the window during which caregiver deprivation seems to have particularly strong effects (14), although ongoing research will be important to test all relevant criteria (157, 159, 160). Future work will also provide critical insight into precisely what becomes biologically embedded during this period and how missed opportunities during this window may have cascading effects later in development (161).
Timing-Related Effects of Adversity
Although considerable evidence indicates that adversity has the strongest effects when experienced earlier in life (10, 11, 14), risk could instead be highest when adversity occurs during specific windows of heightened plasticity that occur later in development. For example, corticolimbic circuitry undergoes substantial changes across childhood and adolescence (60, 162, 163). Particularly in the context of maltreatment, some studies have suggested pronounced effects of adversity on corticolimbic structure or function during childhood or adolescence (148, 164–166). These findings also highlight the complexity of interactions between developmental timing and the type of adversity exposure, sex, and regional specificity in the brain. For example, exposure to maltreatment at ages 10–11 was related to amygdala volume in adulthood, relative to exposure at other ages during development (148), whereas sexual abuse at ages 3–5 and 11–13 was associated with hippocampal volume in adulthood (164). In the functional domain, physical maltreatment during childhood (ages 3–6) was associated with blunted amygdala reactivity in adulthood, whereas peer emotional abuse during adolescence (ages 13 and 15) was linked with increased amygdala response in adulthood (166). While these studies in adulthood provide insight into nonlinear peaks in risk throughout development, future studies conducted during childhood and adolescence will be important for understanding more proximal changes in corticolimbic circuitry and psychopathology that may unfold during development.
PROTECTIVE FACTORS: CAREGIVER SUPPORT AND OPPORTUNITIES FOR RECALIBRATION
Despite the strong association between early adversity and mental health, not all youths exposed to adversity go on to develop psychiatric disorders. Delineating factors that promote resilience in the face of adversity and interactions between these resilience factors (167) is critical for identifying mechanistic targets for intervention, as well as for identifying youths at elevated risk. Stable, supportive caregiving is one of the strongest protective factors against psychopathology in the context of early adversity (168). Youths exposed to adversity who experience higher levels of caregiver support develop lower levels of symptomatology (169–171), and parenting behaviors are associated with children’s symptoms of PTSD (172, 173).
A growing literature has provided increasing insight into the behavioral and neurobiological processes by which caregivers promote healthy development and resilience (174). For example, during childhood, caregiver sensitivity (i.e., the extent to which a caregiver is attuned and responsive to their child) is associated with amygdala volume and microstructure of the amygdala and hippocampus (175), and negative caregiving behavior is associated with amygdala activation and functional connectivity (176). In addition, caregiver control experienced during childhood is associated with amygdala activation and structural integrity of the uncinate fasciculus during young adulthood (177). In the context of adversity exposure, several studies have shown that caregiving support can buffer the effect of adversity on HPA axis function and corticolimbic networks involved in emotion regulation and executive control (178–180). Importantly, supportive caregiving is a modifiable target that can be strengthened through intervention. A randomized controlled trial of a supportive parenting intervention for families living in poverty showed that a longer duration of living in poverty during adolescence was associated with reduced amygdala and hippocampal volumes among young adults in the control condition (informational brochures), but not among young adults whose families participated in the Strong African American Families Program (181). Taken together, these findings indicate that supportive caregiving may buffer the risk of psychopathology following adversity by modulating corticolimbic circuitry, which can be targeted effectively through psychosocial intervention.
Caregiver Buffering
Caregivers play a central role in helping to regulate children’s emotions and stress reactivity in the context of adversity (182–185). Recent research provides insight into the neurobiological mechanisms that may underlie these effects. Paralleling evidence in rodents and macaques (186, 187), caregiver presence can buffer children’s responses to stress by dampening cortisol reactivity (188) and amygdala reactivity (189). These findings suggest that caregivers may serve an external regulatory function while corticolimbic circuitry is still developing. Early biological embedding of safe and predictable caregiver-related cues during infancy may set the stage for caregivers, and eventually other attachment figures, to support regulation later in development (161, 190). Consistent with the idea that early experiences with caregivers may shape subsequent experiences of social buffering, early caregiving adversity is associated with weaker effects of caregiver buffering later in development across species (191–194). Although caregiver buffering of amygdala reactivity is weaker on average among youths previously exposed to caregiver deprivation, there is substantial variability in caregiver buffering following adversity. Among youths who experienced caregiving adversity, 40% show reduced amygdala reactivity to parental cues, and these youths exhibit lower anxiety up to 3 years later (191). These findings suggest that caregiver buffering of amygdala reactivity may promote resilience among youths at elevated risk of psychopathology following adversity.
Opportunities for Recalibration
Just as periods of heightened plasticity can be associated with vulnerability, they also present opportunities for resilience. Recent evidence highlights the potential for adolescence to confer unique opportunities for recalibration of the HPA axis among youths exposed to early adversity who are later living in more favorable conditions. Children who were previously exposed to early caregiver deprivation via institutionalized care and later adopted into stable, supportive family environments show blunted cortisol reactivity to psychosocial stressors, and this effect can persist even years after adoption (10). However, they show increasing cortisol reactivity with pubertal development, such that their stress response did not differ from that of never-institutionalized youths following puberty (195, 196). These findings suggest that puberty may confer greater plasticity in the HPA axis, which facilitates recalibration to the current environment and the potential for heightened influences of supportive caregiving environments during this time. Future research that further examines the nature of an adolescent environment that facilitates recalibration, as well as the potential neural and behavioral consequences of pubertal recalibration (197), will be critical to inform translation to promote resilience.
CHALLENGES AND FUTURE DIRECTIONS IN THE STUDY OF EARLY ADVERSITY
Key Challenges
Research on early adversity has made considerable progress in delineating neurodevelopmental mechanisms underlying risk for psychiatric disorders, key timing and experiential factors that contribute to heterogeneity in exposure and outcomes, and protective factors that promote resilience. However, the field must confront several major barriers to continue advancing empirical knowledge and theory of early adversity.
One fascinating but challenging reality is the vast intricacy of the environment, the developing brain, and human behavior; there is much complexity and heterogeneity in adversity exposure itself and in neurodevelopmental and behavioral trajectories among youths exposed to adversity. Conceptual models have struggled to integrate burgeoning findings on the effects of early adversity on brain development and mental health. At the same time, in practice, empirically testing key predictions from complex conceptual models presents significant challenges. Because it would be unethical and infeasible to experimentally manipulate the nature or timing of adversity exposure in humans, the observational design of most studies in humans limits mechanistic insights and causal interpretations. Moreover, there is substantial chronicity and co-occurrence of adversities, and dimensions of adversity, in youths (2, 4, 198, 199), and such adversities occur in the context of an ever-shifting broader ecosystem (96, 200–202). Many studies have lacked the statistical power to examine complex higher-order interactions (e.g., of the timing and type of adversity) or to model risk factors that may be highly collinear (93, 137).
Measurement issues further hinder advances in the study of early adversity. Studies of early adversity often rely on retrospective self-report (203) of early experiences that are linked with measures of brain and behavioral functioning that are collected in adulthood (165). While recent evidence highlights the predictive validity and utility of self-reported measures of adversity, even when retrospective (204), this study design still precludes a developmental understanding of risk and resilience. In addition, most studies lack precise information about the developmental timing of adversity exposure or the depth of phenotyping that would be needed to test predictions from dominant conceptual models. Lastly, given that development and key processes relevant to adversity and mental health can unfold on the order of years, but also on a moment-to-moment basis, the optimal time frame for sampling to accurately model development may be practically impossible in humans.
Here, I highlight key themes for future research that will be essential to overcoming these challenges and fostering mechanistic insights and more precise prediction of mental health outcomes in the field.
Cross-Species Translation
Consistent with the foundational contributions of cross-species research to our current knowledge of early adversity (14, 56, 78, 205, 206), translational insights from research in animals will continue to be essential to mechanistic understanding of the links between early adversity and mental health. The ability to manipulate the type and timing of risk and protective factors in animal models provides opportunities to test key predictions about development and the environment (207, 208). In particular, research in rodents and nonhuman primates can inform questions about sensitive periods of neuroplasticity and the neurobiological mechanisms that link adversity with developmental outcomes. Robust evidence across species has shown that neural and behavioral phenotypes following adversity result from a complex interplay between environmental, genetic, and epigenetic factors (209–212). Genetic predisposition plays an important role in developmental outcomes, with evidence that the effects of adversity depend in part on one’s genotype. However, given the co-occurrence of early adversity with numerous genetic and environmental factors that affect children, caregivers, and family functioning, dissociating the contributions of heritable factors that co-occur with early adversity, relative to early adversity itself, presents a significant challenge (123). As one example, there is shared genetic vulnerability between children and parents, and the same heritable factors that contribute to a child’s susceptibility to stress may contribute to their caregiver’s behavior. While animal studies employing experimental designs have shown that adversity per se does play a causal role in developmental outcomes (123, 156, 213), much remains unknown about how a combination of adversity, genetic risk, and gene-environment interplay contributes to risk and resilience. Cross-species research has also increasingly demonstrated the role of epigenetic effects, such as regulation of gene expression, in linking early experiences with alterations in corticolimbic circuitry and behavior and will be central to mechanistic insights in this realm (214–218).
Cross-species translation in research on early adversity benefits from a relatively high degree of conservation of corticolimbic circuitry that is sensitive to adversity across species (219–221) and ongoing refinement of translational models of the early environment (56, 111, 222, 223). Progress will be greatly facilitated by meaningful cross-talk between researchers studying early adversity in humans and in animals (213, 224), including dialogues that inform translation both from animals to humans and from humans to animals, as well as direct collaborations (56, 111, 225–227).
Longitudinal Developmental Investigations
Some of the field’s most pressing questions—including about the effects of adversity on the pace of brain development (e.g., stress acceleration) and about sensitive periods that may confer vulnerability but also offer opportunities for resilience (e.g., for pubertal recalibration)—involve developmental timing and trajectories. While cross-sectional designs require fewer resources and time, longitudinal designs that facilitate examination of within-person change over time (228) among youths exposed to adversity are necessary to more rigorously address these questions. Moreover, for many areas of inquiry, such longitudinal data need to be collected prior to adulthood and during specific windows of development in order to facilitate knowledge about how development unfolds. It would be impractical to draw inferences about the timing of a developmental process from neural and behavioral data collected in adulthood. As one example of the need for longitudinal developmental studies, much of the research providing evidence of acceleration of corticolimbic circuitry following adversity has been conducted cross-sectionally (81–83, 85, 86, 229). Longitudinal examinations will be important to reconcile inconsistent findings in this area (59), examine convergence or divergence in effects across different biological levels (e.g., corticolimbic circuitry, epigenetic aging, pubertal timing), and evaluate the extent to which acceleration may facilitate adaptation in the short term but be associated with consequences in the longer term.
“Big Data” and Collaboration
The inherent complexity of shifting environments and co-occurrence of different types of adversity (e.g., adversity characterized by varying degrees of threat, deprivation, or unpredictability) necessitate large sample sizes to ensure sufficient statistical power for complex modeling of higher-order interactions and change over time. Depending on the nature of adversity being studied, large sample sizes can also be required for adequately sampling youths with specific exposures. A growing number of large, collaborative cross-sectional or longitudinal big data studies exist that employ neuroimaging and assessments of the early environment and mental health among youths (230–242). These data sets can be orders of magnitude larger than traditional studies in human neuroscience (243) and increase the likelihood of identifying robust and reproducible findings related to the effects of early adversity, particularly with regard to phenotypic associations with brain development (244). At the same time, big data studies will not be able to address all important questions in this realm. The prevalence of some adversities will be too low in studies that did not ascertain youths based on exposure to adversity, and large-scale efforts are unlikely to have the capacity to collect in-depth assessments of adversity exposure at the level of precise developmental timing and dimensionality that can be prioritized in smaller-scale studies focused specifically on adversity. Thus, more general big data studies and studies that sample from specific populations (e.g., children who experienced maltreatment) or employ deeper phenotyping will provide complementary insights. In order to enhance statistical power for investigations with deeper phenotyping of early adversity, meta-analytic efforts focused on early adversity (e.g., via the Enhancing Neuro-Imaging Genetics Through Meta-Analysis consortium [245]) and multisite collaborations among researchers who have collected overlapping or harmonized measures of early adversity (19) will be essential to advancing knowledge. Leveraging large longitudinal studies to test and expand on existing hypotheses and age-related findings derived from smaller cross-sectional studies and, in turn, applying insights gained from big data to more intensively investigate a specific phenomenon in smaller, investigator-led studies represent promising strategies for maximizing the value of complementary efforts in the field of early adversity and development.
Advanced Computational Approaches
Ongoing methodological advances will facilitate discovery about the mechanisms underlying the links between early adversity and mental health and the prediction of outcomes following adversity. Various conceptual approaches to early adversity have converged on the importance of parsing heterogeneity in the nature, timing, and experiential elements of adversity exposure and developmental outcomes to accelerate progress in identifying risk and mechanistic targets (13, 15, 21, 28, 88, 94, 95, 100, 117, 136). In addition to more traditional approaches that have been used to test predictions about a priori dimensions or timing of adversity, data-driven computational approaches may be particularly useful for identifying specific developmental windows associated with heightened risk or resilience (165, 166, 246) or for examining variability in exposure or outcomes to empirically derive key features of adversity exposure (247–249). As one example, a recent study applied similarity network fusion to large-scale environmental and brain imaging data from the Adolescent Brain Cognitive Development Study with the aim of decomposing heterogeneous associations between brain structure and specific aspects of the childhood environment (248). The findings identified subgroups of youths who displayed more homogeneous brain-environment associations, and this subtyping approach enhanced prediction of mental health symptoms (which was not possible without the subtyping). These findings suggest that it is possible to meaningfully parse heterogeneity in associations between the early environment and brain structure during development, and that doing so may enhance risk identification and facilitate mechanistic insights.
Advanced computational approaches will also provide novel insight into questions around developmental timing and plasticity. Recent years have witnessed transformative discoveries of the molecular triggers (e.g., excitatory-inhibitory balance) and brakes (e.g., perineuronal nets, myelin) that control the onset and closure of sensitive periods, as well as the insight that sensitive-period processes are themselves malleable (150). However, studying these processes in humans has been infeasible. A recent study (250) used a GABAergic benzodiazepine challenge to empirically generate a model of excitatory-inhibitory ratio based on multivariate patterns of functional connectivity in humans. The researchers then applied that model to a developmental sample of youths ages 8–22 and showed that the model predicted reductions in excitatory-inhibitory ratio during adolescence, which were specific to the association cortex and were related to psychopathology. The gradual reduction in the ratio of excitatory to inhibitory patterns with age that was observed in this study aligns with previous animal work on neurobiological mechanisms of sensitive periods (157, 251–253). These findings are consistent with the idea that adolescence is a sensitive period for the association cortex and represent a significant advance in the capacity to interrogate plasticity-related processes during human development.
Another significant analytic advance is the use of machine learning models of brain development to examine deviations from typical maturation. In this issue of the Journal, Keding and colleagues (87) leveraged a large multisite data set to examine maturational timing of gray matter volume related to adversity exposure and psychopathology among adolescent girls. They trained stacked generalizer machine learning models with gray matter volume estimates from whole-brain, emotion-related, and language-related circuit parcellations to predict chronological age in typically developing girls. These models generated brain age gap estimates (BrainAGEs) from gray matter volume of girls exposed to abuse or neglect and with internalizing disorders. Subsequent feature influence analyses interrogated which neural features contributed to adversity- and psychopathology-related differences in BrainAGE. Collectively, these studies highlight significant advances that have great promise in facilitating novel insights into the mechanisms underlying risk for adversity-related psychopathology in humans.
Refining Conceptual Models
Progress in understanding the effects of early adversity and mechanisms associated with risk and resilience, with the eventual goal of clinical translation, will rely on continual refinement of conceptual models. Theoretical approaches must grapple with the immense complexity of the developing brain, the environment, and behavior (254). A useful model of early adversity and neurodevelopment must account for the vast heterogeneity in outcomes and key concepts of equifinality (i.e., distinct early experiences leading to similar outcomes) and multifinality (i.e., similar early experiences leading to distinct outcomes) from developmental psychopathology (255, 256). In addition, while adversity is often conceptualized as influencing the brain and behavior (i.e., a unidirectional pathway), nuanced conceptualizations that facilitate empirical advances must account for the transactional nature of development. Developing youths are embedded within broader social contexts (96, 201, 202), and neural and behavioral alterations that follow adversity are not simply outcomes but also factors that reciprocally shape these contexts (212) and can alter the course of development (257).
While refinements and innovation in conceptual models could take many directions, several areas may be particularly fruitful for ongoing interplay between empirical research and conceptual refinement given the current state of the literature. First, dimensional models of adversity can flexibly allow for the incorporation of additional dimensions (13, 97) and will benefit from increased emphasis on the child’s own perception and experience of any given event (136, 204, 258, 259). As one example, in addition to threat, deprivation, and unpredictability (88, 98, 99), Cohodes and colleagues (13) have proposed a framework in which the effects of adversity on corticolimbic circuitry and mental health vary depending on the extent to which adversity is characterized by perceived controllability and caregiver involvement. Critically, building on a robust literature on the developmental timing of adversity (14, 15, 21, 28, 94), this framework emphasizes the importance of interactions between key experiential elements of adversity and the developmental timing of adversity exposure. Delineating when specific experiential elements of adversity differentially impact outcomes, and how those effects differ by developmental stage, could inform efforts to optimize risk identification based on developmental stage or the nature of adversity exposure (13, 260).
Second, despite converging evidence that the effects of adversity can differ as a function of developmental timing of exposure, evaluation of which developmental differences fit the criteria for a sensitive period is rare (159, 261). Elucidating the experience-related mechanisms (262) underlying timing-related effects, as well as precisely what is biologically embedded during a given sensitive period, is essential to understanding the mechanisms by which early experiences shape neurobehavioral development (160, 161). Bridging insights from formal modeling (261) and empirical studies across species (263) may facilitate meaningful refinement of conceptual models of early adversity.
Lastly, while adversity-related alterations in neurobiology or behavior are often framed as detrimental, alternative perspectives highlight the adaptive nature of some phenotypes following adversity (58, 82, 264–267). That is, such ontogenetic adaptations may bolster the ability to cope with or survive in a harsh and unpredictable environment (62, 262, 266, 268). A more nuanced understanding of the neurobiological and behavioral effects of adversity during development is critical to a more comprehensive conceptualization of early adversity, as well as to promoting resilience and adaptive behavior in the face of future adversity. Reevaluating “deficit models” and carefully considering frameworks that emphasize adaptation and even areas of increased strength following adversity (e.g., “hidden talents”) (269, 270) could both stimulate important scientific discoveries and shift the often dominant narrative of deficits that can contribute to stigma of youths exposed to adversity (29, 271).
Translation to Intervention
Building on progress in identifying mechanisms linking early adversity with mental health, translating such knowledge to inform intervention and prevention strategies for youths exposed to adversity is a critical goal for the field. Although existing evidence-based treatments can be highly effective for youths who develop psychopathology following adversity (272–276), a substantial proportion of youths do not sufficiently benefit from existing treatments (277). Moreover, there is great need to enhance prevention strategies that can be employed following adversity and prior to the development of psychopathology. Even with similar clinical presentations, some evidence suggests that individuals exposed to early adversity differ in important ways from individuals not exposed to early adversity (278–280), further highlighting the importance of efforts to optimize treatments for youths exposed to adversity.
Continual advances in research on early adversity can inform prevention and intervention strategies in several key ways. First, cross-species research can specifically delineate the timing of sensitive periods, which may render the developing brain more vulnerable to the effects of adversity but also provide enhanced opportunities for positive change through intervention (28). Corticolimbic circuitry and related functions such as fear learning and emotion regulation, which are altered following adversity, undergo dynamic changes across development (281–285). Thus, youths with adversity-related psychopathology may benefit from interventions that are specifically optimized based on the biological state of the developing brain (260, 286, 287). Second, building on conceptual models that emphasize key experiential elements of adversity exposure, as well as their interaction with developmental timing, may represent a powerful approach to optimizing interventions for a given individual based on factors such as the individual’s developmental stage or a profile of adversity exposure (13). Third, knowledge of the mechanisms underlying risk for psychopathology following early adversity will be important for identifying modifiable processes that can be targeted in treatment. As one example, consistent evidence has linked early adversity with alterations in threat-related social information processing biases, heightened emotional reactivity and difficulties with emotion regulation, and disruptions in reward processing, all of which are associated with specific targets for intervention (288). By contrast, less is known about adversity-related alterations in emotional learning (86, 121, 122, 289). Given that emotional learning undergoes marked changes during development (60, 290–292) and is the target of many well-established interventions (293, 294), ongoing research on learning-related processes following adversity may be particularly useful for fostering progress in clinical translation (288). Lastly, enhancing caregiver support, a well-established protective factor in the context of adversity, provides another important target for intervention and is already a central component of many interventions (295, 296). Future investigations of the specific mechanisms by which interventions can facilitate the recovery of caregiver capacities for regulation following missed opportunities for predictable, safe caregiver cues during an early sensitive period may be particularly helpful for informing intervention strategies for youths exposed to early adversity (161). Taken together, these areas for future research highlight the need to enhance the efficacy of interventions for youths exposed to adversity and the potential for precision medicine approaches that tailor interventions based on the developmental timing or specific features of adversity exposure.
CONCLUSIONS
Exposure to early adversity is a potent risk factor for psychopathology. Cross-species investigations have facilitated substantial progress in delineating neurodevelopmental mechanisms associated with risk and resilience following early adversity. However, the vast complexity and heterogeneity in early environments and in developmental trajectories following adversity present challenges to achieving mechanistic insight and effective clinical translation. An overview of the current state of the field points to the importance of longitudinal investigation in large developmental samples, coupled with deeper phenotyping of the early environment in youths exposed to adversity, and the potential for advanced computational approaches to parse heterogeneity and provide novel insight into sensitive periods. Ongoing refinement of conceptual models that incorporates insights from cross-species research and developmental psychopathology will be essential to future progress and translation to enhance risk identification and optimize interventions for youths exposed to adversity.
1 : Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry 2007; 64:577–584Crossref, Medline, Google Scholar
2 : Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry 2010; 67:113–123Crossref, Medline, Google Scholar
3 : Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry 2010; 197:378–385Crossref, Medline, Google Scholar
4 : Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry 2012; 69:1151–1160Crossref, Medline, Google Scholar
5 : The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006; 256:174–186Crossref, Medline, Google Scholar
6 : Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open 2018; 1:e184493Crossref, Medline, Google Scholar
7 : The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2017; 2:e356–e366Crossref, Medline, Google Scholar
8 : Prevalence of adverse childhood experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatr 2018; 172:1038–1044Crossref, Medline, Google Scholar
9 : Early childhood adversity, toxic stress, and the impacts of racism on the foundations of health. Annu Rev Public Health 2021; 42:115–134Crossref, Medline, Google Scholar
10 : Moderate versus severe early life stress: associations with stress reactivity and regulation in 10-12-year-old children. Psychoneuroendocrinology 2009; 34:62–75Crossref, Medline, Google Scholar
11 : Causal effects of the early caregiving environment on development of stress response systems in children. Proc Natl Acad Sci USA 2015; 112:5637–5642Crossref, Medline, Google Scholar
12 : Early-life stress disrupts attachment learning: the role of amygdala corticosterone, locus ceruleus corticotropin releasing hormone, and olfactory bulb norepinephrine. J Neurosci 2009; 29:15745–15755Crossref, Medline, Google Scholar
13 : Influences of early-life stress on frontolimbic circuitry: harnessing a dimensional approach to elucidate the effects of heterogeneity in stress exposure. Dev Psychobiol 2021; 63:153–172Crossref, Medline, Google Scholar
14 : Effects of stress throughout the lifespan on the brain, behaviour, and cognition. Nat Rev Neurosci 2009; 10:434–445Crossref, Medline, Google Scholar
15 : A review of adversity, the amygdala, and the hippocampus: a consideration of developmental timing. Front Hum Neurosci 2010; 3:68Medline, Google Scholar
16 : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology. Am J Psychiatry 2019; 176:987–999Link, Google Scholar
17 : Neuroendocrine coupling across adolescence and the longitudinal influence of early life stress. Dev Psychobiol 2015; 57:688–704Crossref, Medline, Google Scholar
18 : Longitudinal changes in amygdala, hippocampus, and cortisol development following early caregiving adversity. Dev Cogn Neurosci 2021; 48:100916Crossref, Medline, Google Scholar
19 : Childhood adversity and neural development: a systematic review. Annu Rev Dev Psychol 2019; 1:277–312Crossref, Medline, Google Scholar
20 : Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl) 2011; 214:55–70Crossref, Medline, Google Scholar
21 : The effects of childhood maltreatment on brain structure, function, and connectivity. Nat Rev Neurosci 2016; 17:652–666Crossref, Medline, Google Scholar
22 : Developmental pathways to amygdala-prefrontal function and internalizing symptoms in adolescence. Nat Neurosci 2012; 15:1736–1741Crossref, Medline, Google Scholar
23 : Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc Natl Acad Sci USA 2013; 110:19119–19124Crossref, Medline, Google Scholar
24 : Brain corticosteroid receptor balance in health and disease. Endocr Rev 1998; 19:269–301Crossref, Medline, Google Scholar
25 : Colocalization of peptide and glucocorticoid receptor immunoreactivities in rat central amygdaloid nucleus. Neuroendocrinology 1992; 55:451–459Crossref, Medline, Google Scholar
26 : Long-term consequences of neonatal rearing on central corticotropin-releasing factor systems in adult male rat offspring. Neuropsychopharmacology 2005; 30:2192–2204Crossref, Medline, Google Scholar
27 : Exposure to excess glucocorticoids alters dendritic morphology of adult hippocampal pyramidal neurons. Brain Res 1990; 531:225–231Crossref, Medline, Google Scholar
28 : The impact of developmental timing for stress and recovery. Neurobiol Stress 2015; 1:184–194Crossref, Medline, Google Scholar
29 : Amygdala allostasis and early life adversity: considering excitotoxicity and inescapability in the sequelae of stress. Front Hum Neurosci 2021; 15:624705Crossref, Medline, Google Scholar
30 : During infant maltreatment, stress targets hippocampus, but stress with mother present targets amygdala and social behavior. Proc Natl Acad Sci USA 2019; 116:22821–22832Crossref, Medline, Google Scholar
31 : Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med 2010; 40:1647–1658Crossref, Medline, Google Scholar
32 : Stress sensitization among severely neglected children and protection by social enrichment. Nat Commun 2019; 10:5771Crossref, Medline, Google Scholar
33 : Lower structural integrity of the uncinate fasciculus is associated with a history of child maltreatment and future psychological vulnerability to stress. Dev Psychopathol 2015; 27:1611–1619Crossref, Medline, Google Scholar
34 : Reduced hippocampal and amygdala volume as a mechanism underlying stress sensitization to depression following childhood trauma. Depress Anxiety 2020; 37:916–925Crossref, Medline, Google Scholar
35 : Research review: neural response to threat in children, adolescents, and adults after child maltreatment: a quantitative meta-analysis. J Child Psychol Psychiatry 2017; 58:222–230Crossref, Medline, Google Scholar
36 : Differential roles of the salience network during prediction error encoding and facial emotion processing among female adolescent assault victims. Biol Psychiatry Cogn Neurosci Neuroimaging 2019; 4:371–380Crossref, Medline, Google Scholar
37 : Disrupted insula-based neural circuit organization and conflict interference in trauma-exposed youth. Neuroimage Clin 2015; 8:516–525Crossref, Medline, Google Scholar
38 : Heightened neural reactivity to threat in child victims of family violence. Curr Biol 2011; 21:R947–R948Crossref, Medline, Google Scholar
39 : Child maltreatment and neural systems underlying emotion regulation. J Am Acad Child Adolesc Psychiatry 2015; 54:753–762Crossref, Medline, Google Scholar
40 : Salience processing and insular cortical function and dysfunction. Nat Rev Neurosci 2015; 16:55–61Crossref, Medline, Google Scholar
41 : Corticostriatal-limbic gray matter morphology in adolescents with self-reported exposure to childhood maltreatment. Arch Pediatr Adolesc Med 2011; 165:1069–1077Crossref, Medline, Google Scholar
42 : Risk taking, decision-making, and brain volume in youth adopted internationally from institutional care. Neuropsychologia 2018; 119:262–270Crossref, Medline, Google Scholar
43 : Cortical thickness, surface area, and gyrification abnormalities in children exposed to maltreatment: neural markers of vulnerability? Biol Psychiatry 2013; 74:845–852Crossref, Medline, Google Scholar
44 : The frontoparietal network: function, electrophysiology, and importance of individual precision mapping. Dialogues Clin Neurosci 2018; 20:133–140Crossref, Medline, Google Scholar
45 : Widespread reductions in cortical thickness following severe early-life deprivation: a neurodevelopmental pathway to attention-deficit/hyperactivity disorder. Biol Psychiatry 2014; 76:629–638Crossref, Medline, Google Scholar
46 : Early-life stress is associated with impairment in cognitive control in adolescence: an fMRI study. Neuropsychologia 2010; 48:3037–3044Crossref, Medline, Google Scholar
47 : Differential associations of distinct forms of childhood adversity with neurobehavioral measures of reward processing: a developmental pathway to depression. Child Dev 2019; 90:e96–e113Crossref, Medline, Google Scholar
48 : Altered ventral striatal-medial prefrontal cortex resting-state connectivity mediates adolescent social problems after early institutional care. Dev Psychopathol 2017; 29:1865–1876Crossref, Medline, Google Scholar
49 : Reduced nucleus accumbens reactivity and adolescent depression following early-life stress. Neuroscience 2013; 249:129–138Crossref, Medline, Google Scholar
50 : The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology 2010; 35:4–26Crossref, Medline, Google Scholar
51 : Cumulative stress in childhood is associated with blunted reward-related brain activity in adulthood. Soc Cogn Affect Neurosci 2016; 11:405–412Crossref, Medline, Google Scholar
52 : Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biol Psychiatry 2015; 78:598–605Crossref, Medline, Google Scholar
53 : Hyporesponsive reward anticipation in the basal ganglia following severe institutional deprivation early in life. J Cogn Neurosci 2010; 22:2316–2325Crossref, Medline, Google Scholar
54 : Mechanisms linking childhood trauma exposure and psychopathology: a transdiagnostic model of risk and resilience. BMC Med 2020; 18:96Crossref, Medline, Google Scholar
55 : Neurobiological programming of early life stress: functional development of amygdala-prefrontal circuitry and vulnerability for stress-related psychopathology. Curr Top Behav Neurosci 2018; 38:117–136Crossref, Medline, Google Scholar
56 : Early-life stress has persistent effects on amygdala function and development in mice and humans. Proc Natl Acad Sci USA 2013; 110:18274–18278Crossref, Medline, Google Scholar
57 : Human amygdala development in the absence of species-expected caregiving. Dev Psychobiol 2012; 54:598–611Crossref, Medline, Google Scholar
58 : The stress acceleration hypothesis: effects of early-life adversity on emotion circuits and behavior. Curr Opin Behav Sci 2016; 7:76–81Crossref, Medline, Google Scholar
59 : Biological aging in childhood and adolescence following experiences of threat and deprivation: a systematic review and meta-analysis. Psychol Bull 2020; 146:721–764Crossref, Medline, Google Scholar
60 : Neurocognitive development of motivated behavior: dynamic changes across childhood and adolescence. J Neurosci 2018; 38:9433–9445Crossref, Medline, Google Scholar
61 : Environmental influences on the pace of brain development. Nat Rev Neurosci 2021; 22:372–384Crossref, Medline, Google Scholar
62 : Early-life adversity accelerates child and adolescent development. Curr Dir Psychol Sci 2019; 28:241–246Crossref, Google Scholar
63 : Childhood experience, interpersonal development, and reproductive strategy: and evolutionary theory of socialization. Child Dev 1991; 62:647–670Crossref, Medline, Google Scholar
64 : The evolution of predictive adaptive responses in human life history. Proc Biol Sci 2013; 280:20131343Medline, Google Scholar
65 : Why are childhood family factors associated with timing of maturation? A role for internal prediction. Perspect Psychol Sci 2014; 9:3–15Crossref, Medline, Google Scholar
66 : Early adversity, elevated stress physiology, accelerated sexual maturation, and poor health in females. Dev Psychol 2015; 51:816–822Crossref, Medline, Google Scholar
67 : Earlier age at menarche as a transdiagnostic mechanism linking childhood trauma with multiple forms of psychopathology in adolescent girls. Psychol Med 2020; 50:1090–1098Crossref, Medline, Google Scholar
68 : Early-life stress leads to sex-dependent changes in pubertal timing in rats that are reversed by a probiotic formulation. Dev Psychobiol 2019; 61:679–687Crossref, Medline, Google Scholar
69 : Psychosocial antecedents of variation in girls’ pubertal timing: maternal depression, stepfather presence, and marital and family stress. Child Dev 2000; 71:485–501Crossref, Medline, Google Scholar
70 : Associations between early life stress, child maltreatment, and pubertal development among girls in foster care. J Res Adolesc 2011; 21:871–880Crossref, Medline, Google Scholar
71 : Pubertal development mediates the association between family environment and brain structure and function in childhood. Dev Psychopathol 2020; 32:687–702Crossref, Medline, Google Scholar
72 : Attenuated hypothalamic-pituitary-adrenal axis functioning predicts accelerated pubertal development in girls 1 year later. Dev Psychopathol 2015; 27:819–828Crossref, Medline, Google Scholar
73 : Accelerated telomere shortening: tracking the lasting impact of early institutional care at the cellular level. Psychiatry Res 2016; 246:95–100Crossref, Medline, Google Scholar
74 : Exposure to violence accelerates epigenetic aging in children. Sci Rep 2017; 7:8962Crossref, Medline, Google Scholar
75 : Adversity exposure during sensitive periods predicts accelerated epigenetic aging in children. Psychoneuroendocrinology 2020; 113:104484Crossref, Medline, Google Scholar
76 : Early experiences of threat, but not deprivation, are associated with accelerated biological aging in children and adolescents. Biol Psychiatry 2019; 85:268–278Crossref, Medline, Google Scholar
77 : Traumatic stress and accelerated DNA methylation age: a meta-analysis. Psychoneuroendocrinology 2018; 92:123–134Crossref, Medline, Google Scholar
78 : Early life stress accelerates behavioral and neural maturation of the hippocampus in male mice. Horm Behav 2016; 82:64–71Crossref, Medline, Google Scholar
79 : Altered corticolimbic connectivity reveals sex-specific adolescent outcomes in a rat model of early life adversity. eLife 2020; 9:e52651Crossref, Medline, Google Scholar
80 : Early life adversity decreases pre-adolescent fear expression by accelerating amygdala PV cell development. eLife 2020; 9:e55263Crossref, Medline, Google Scholar
81 : The association between early life stress and prefrontal cortex activation during implicit emotion regulation is moderated by sex in early adolescence. Dev Psychopathol 2017; 29:1851–1864Crossref, Medline, Google Scholar
82 : Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proc Natl Acad Sci USA 2013; 110:15638–15643Crossref, Medline, Google Scholar
83 : Accelerated maturation in functional connectivity following early life stress: circuit specific or broadly distributed? Dev Cogn Neurosci 2021; 48:100922Crossref, Medline, Google Scholar
84 : Early life stress, frontoamygdala connectivity, and biological aging in adolescence: a longitudinal investigation. Cereb Cortex 2020; 30:4269–4280Crossref, Medline, Google Scholar
85 : Associations between amygdala-prefrontal functional connectivity and age depend on neighborhood socioeconomic status. Cereb Cortex Commun (Online ahead of print, July 23, 2020) Google Scholar
86 : Previous institutionalization is followed by broader amygdala-hippocampal-PFC network connectivity during aversive learning in human development. J Neurosci 2016; 36:6420–6430Crossref, Medline, Google Scholar
87 : Differential patterns of delayed emotion circuit maturation in abused girls with and without internalizing psychopathology. Am J Psychiatry 2021; 178:1026–1036Link, Google Scholar
88 : Fundamental dimensions of environmental risk: the impact of harsh versus unpredictable environments on the evolution and development of life history strategies. Hum Nat 2009; 20:204–268Crossref, Medline, Google Scholar
89 : Enhanced prefrontal-amygdala connectivity following childhood adversity as a protective mechanism against internalizing in adolescence. Biol Psychiatry Cogn Neurosci Neuroimaging 2016; 1:326–334Crossref, Medline, Google Scholar
90 : Developmental traumatology, part II: brain development. Biol Psychiatry 1999; 45:1271–1284Crossref, Medline, Google Scholar
91 : Prolonged institutional rearing is associated with atypically large amygdala volume and difficulties in emotion regulation. Dev Sci 2010; 13:46–61Crossref, Medline, Google Scholar
92 : Designing research to study the effects of institutionalization on brain and behavioral development: the Bucharest Early Intervention Project. Dev Psychopathol 2003; 15:885–907Crossref, Medline, Google Scholar
93 : Cumulative risk and child development. Psychol Bull 2013; 139:1342–1396Crossref, Medline, Google Scholar
94 : How the timing and quality of early experiences influence the development of brain architecture. Child Dev 2010; 81:28–40Crossref, Medline, Google Scholar
95 : Dimensions of child maltreatment and children’s adjustment: contributions of developmental timing and subtype. Dev Psychopathol 2001; 13:759–782Crossref, Medline, Google Scholar
96 : Early violence exposure and self-regulatory development: a bioecological systems perspective. Hum Development 2013; 56:254–273Crossref, Google Scholar
97 : The value of dimensional models of early experience: thinking clearly about concepts and categories. Perspect Psychol Sci (Online ahead of print, September 7, 2021) Google Scholar
98 : Dimensions of early experience and neural development: deprivation and threat. Trends Cogn Sci 2014; 18:580–585Crossref, Medline, Google Scholar
99 : Fragmentation and unpredictability of early-life experience in mental disorders. Am J Psychiatry 2012; 169:907–915Link, Google Scholar
100 : Beyond cumulative risk: distinguishing harshness and unpredictability as determinants of parenting and early life history strategy. Dev Psychol 2012; 48:662–673Crossref, Medline, Google Scholar
101 : The influence of unpredictable, fragmented parental signals on the developing brain. Front Neuroendocrinol 2019; 53:100736Crossref, Medline, Google Scholar
102 : Infants may use contingency analysis to estimate environmental states: an evolutionary, life-history perspective. Child Dev Perspect 2013; 7:115–120Crossref, Google Scholar
103 :
104 : Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev 2005; 7:349–367Crossref, Medline, Google Scholar
105 : Mechanisms of late-onset cognitive decline after early-life stress. J Neurosci 2005; 25:9328–9338Crossref, Medline, Google Scholar
106 : Reduced resting-state functional connectivity of the basolateral amygdala to the medial prefrontal cortex in preweaning rats exposed to chronic early-life stress. Brain Struct Funct 2018; 223:3711–3729Crossref, Medline, Google Scholar
107 : Anhedonia following early-life adversity involves aberrant interaction of reward and anxiety circuits and is reversed by partial silencing of amygdala corticotropin-releasing hormone gene. Biol Psychiatry 2018; 83:137–147Crossref, Medline, Google Scholar
108 : Early-life adversity facilitates acquisition of cocaine self-administration and induces persistent anhedonia. Neurobiol Stress 2018; 8:57–67Crossref, Medline, Google Scholar
109 : Fragmentation and high entropy of neonatal experience predict adolescent emotional outcome. Transl Psychiatry 2016; 6:e702Crossref, Medline, Google Scholar
110 : Does anhedonia presage increased risk of posttraumatic stress disorder? Adolescent anhedonia and posttraumatic disorders. Curr Top Behav Neurosci 2018; 38:249–265Crossref, Medline, Google Scholar
111 : Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proc Natl Acad Sci USA 2017; 114:10390–10395Crossref, Medline, Google Scholar
112 : Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J Child Psychol Psychiatry 2007; 48:329–354Crossref, Medline, Google Scholar
113 : Influences of environmental demand on maternal behavior and infant development. Acta Paediatr Suppl 1994; 397:57–63Crossref, Medline, Google Scholar
114 : The effects of varying environmental demands on maternal and infant behavior. Child Dev 1984; 55:305–314Crossref, Medline, Google Scholar
115 : Aberrant maturation of the uncinate fasciculus follows exposure to unpredictable patterns of maternal signals. J Neurosci 2021; 41:1242–1250Crossref, Medline, Google Scholar
116 : Theory and measurement of environmental unpredictability. Evolution and Human Behavior 2020; 41:550–556Google Scholar
117 : Beyond cumulative risk: a dimensional approach to childhood adversity. Curr Dir Psychol Sci 2016; 25:239–245Crossref, Medline, Google Scholar
118 : Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev 2014; 47:578–591Crossref, Medline, Google Scholar
119 : Behavioral problems after early life stress: contributions of the hippocampus and amygdala. Biol Psychiatry 2015; 77:314–323Crossref, Medline, Google Scholar
120 : Childhood maltreatment exposure and disruptions in emotion regulation: a transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognit Ther Res 2016; 40:394–415Crossref, Medline, Google Scholar
121 : Alterations in fear extinction neural circuitry and fear-related behavior linked to trauma exposure in children. Behav Brain Res 2021; 398:112958Crossref, Medline, Google Scholar
122 : Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacology 2016; 41:1956–1964Crossref, Medline, Google Scholar
123 : Mechanisms linking early experience and the emergence of emotions: illustrations from the study of maltreated children. Curr Dir Psychol Sci 2008; 17:370–375Crossref, Medline, Google Scholar
124 : Selective attention to facial emotion in physically abused children. J Abnorm Psychol 2003; 112:323–338Crossref, Medline, Google Scholar
125 : Altered neural processing of threat-related information in children and adolescents exposed to violence: a transdiagnostic mechanism contributing to the emergence of psychopathology. J Am Acad Child Adolesc Psychiatry 2020; 59:1274–1284Crossref, Medline, Google Scholar
126 : Early neglect is associated with alterations in white matter integrity and cognitive functioning. Child Dev 2013; 84:1566–1578Crossref, Medline, Google Scholar
127 : Associations of early-life threat and deprivation with executive functioning in childhood and adolescence: a systematic review and meta-analysis. JAMA Pediatr (Online ahead of print, July 26, 2021) Google Scholar
128 : Childhood maltreatment predicts poorer executive functioning in adulthood beyond symptoms of internalizing psychopathology. Child Abuse Negl 2021; 118:105140Crossref, Medline, Google Scholar
129 : Neurocognitive correlates of socioeconomic status in kindergarten children. Dev Sci 2005; 8:74–87Crossref, Medline, Google Scholar
130 : Dimensions of childhood adversity have distinct associations with neural systems underlying executive functioning. Dev Psychopathol 2017; 29:1777–1794Crossref, Medline, Google Scholar
131 : The effects of early neglect on cognitive, language, and behavioral functioning in childhood. Psychology (Irvine) 2012; 3:175–182Crossref, Medline, Google Scholar
132 : Elevated amygdala response to faces following early deprivation. Dev Sci 2011; 14:190–204Crossref, Medline, Google Scholar
133 : Amygdala, hippocampal, and corpus callosum size following severe early institutional deprivation: the English and Romanian Adoptees study pilot. J Child Psychol Psychiatry 2009; 50:943–951Crossref, Medline, Google Scholar
134 : Effects of early institutionalization on emotion processing in 12-year-old youth. Dev Psychopathol 2017; 29:1749–1761Crossref, Medline, Google Scholar
135 ;
136 : Thinking clearly about biology and childhood adversity: next steps for continued progress. Perspect Psychol Sci (Online ahead of print, September 7, 2021) Google Scholar
137 : Rethinking concepts and categories for understanding the neurodevelopmental effects of childhood adversity. Perspect Psychol Sci 2021; 16:67–93Crossref, Medline, Google Scholar
138 : Characterizing the impact of adversity, abuse, and neglect on adolescent amygdala resting-state functional connectivity. Dev Cogn Neurosci 2021; 47:100894Crossref, Medline, Google Scholar
139 : Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Dev Psychopathol 2017; 29:929–940Crossref, Medline, Google Scholar
140 : Differential associations of deprivation and threat with cognitive control and fear conditioning in early childhood. Front Behav Neurosci 2019; 13:80Crossref, Medline, Google Scholar
141 : Dimensions of deprivation and threat, psychopathology, and potential mediators: a multi-year longitudinal analysis. J Abnorm Psychol 2018; 127:160–170Crossref, Medline, Google Scholar
142 : A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biol Psychiatry 1999; 46:1542–1554Crossref, Medline, Google Scholar
143 : The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012; 129:e232–e246Crossref, Medline, Google Scholar
144 : Environmental programming of susceptibility and resilience to stress in adulthood in male mice. Front Behav Neurosci 2019; 13:40Crossref, Medline, Google Scholar
145 : Childhood maltreatment and its effect on neurocognitive functioning: timing and chronicity matter. Dev Psychopathol 2015; 27:521–533Crossref, Medline, Google Scholar
146 : Beyond family-level adversities: exploring the developmental timing of neighborhood disadvantage effects on the brain. Dev Sci 2021; 24:e12985Crossref, Medline, Google Scholar
147 : Evidence for a sensitive period in the effects of early life stress on hippocampal volume. Dev Sci 2019; 22:e12775Crossref, Medline, Google Scholar
148 : Sensitive periods of amygdala development: the role of maltreatment in preadolescence. Neuroimage 2014; 97:236–244Crossref, Medline, Google Scholar
149 : Sensitive periods in the development of the brain and behavior. J Cogn Neurosci 2004; 16:1412–1425Crossref, Medline, Google Scholar
150 : Critical periods in speech perception: new directions. Annu Rev Psychol 2015; 66:173–196Crossref, Medline, Google Scholar
151 : A neurobiological perspective on early human deprivation. Child Dev Perspect 2007; 1:13–18Crossref, Google Scholar
152 : Adverse rearing environments and neural development in children: the development of frontal electroencephalogram asymmetry. Biol Psychiatry 2011; 70:1008–1015Crossref, Medline, Google Scholar
153 : Normalization of EEG activity among previously institutionalized children placed into foster care: a 12-year follow-up of the Bucharest Early Intervention Project. Dev Cogn Neurosci 2016; 17:68–75Crossref, Medline, Google Scholar
154 : Amygdala hyper-connectivity in a mouse model of unpredictable early life stress. Transl Psychiatry 2018; 8:49Crossref, Medline, Google Scholar
155 : Aberrant development of intrinsic brain activity in a rat model of caregiver maltreatment of offspring. Transl Psychiatry 2017; 7:e1005Crossref, Medline, Google Scholar
156 : Disentangling the effects of early caregiving experience and heritable factors on brain white matter development in rhesus monkeys. Neuroimage 2019; 197:625–642Crossref, Medline, Google Scholar
157 : Balancing plasticity/stability across brain development. Prog Brain Res 2013; 207:3–34Crossref, Medline, Google Scholar
158 : Maturation of the hippocampal formation and amygdala in Macaca mulatta: a volumetric magnetic resonance imaging study. Hippocampus 2010; 20:922–935Crossref, Medline, Google Scholar
159 : Do sensitive periods exist for exposure to adversity? Biol Psychiatry 2019; 85:789–791Crossref, Medline, Google Scholar
160 : Caregiving influences on emotional learning and regulation: applying a sensitive period model. Curr Opin Behav Sci 2020; 36:177–184Crossref, Medline, Google Scholar
161 : Influences of caregiving on development: a sensitive period for biological embedding of predictability and safety cues. Curr Dir Psychol Sci (Online ahead of print, August 6, 2021)Google Scholar
162 : Beyond simple models of adolescence to an integrated circuit-based account: a commentary. Dev Cogn Neurosci 2016; 17:128–130Crossref, Medline, Google Scholar
163 : Development of the emotional brain. Neurosci Lett 2019; 693:29–34Crossref, Medline, Google Scholar
164 : Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. J Neuropsychiatry Clin Neurosci 2008; 20:292–301Crossref, Medline, Google Scholar
165 : Differential effects of childhood neglect and abuse during sensitive exposure periods on male and female hippocampus. Neuroimage 2018; 169:443–452Crossref, Medline, Google Scholar
166 : Association of prepubertal and postpubertal exposure to childhood maltreatment with adult amygdala function. JAMA Psychiatry 2019; 76:843–853Crossref, Medline, Google Scholar
167 : A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry 2018; 9:230Crossref, Medline, Google Scholar
168 : Understanding and promoting resilience in children and youth. Curr Opin Psychiatry 2011; 24:267–273Crossref, Medline, Google Scholar
169 : Responsive parenting buffers the impact of maternal PTSD on young children. Parent Sci Pract 2020; 20:141–165Crossref, Medline, Google Scholar
170 : Caregiver support buffers posttraumatic stress disorder symptoms following a natural disaster in relation to binge drinking. Psychol Trauma (Online ahead of print, March 5, 2020)Google Scholar
171 : A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev 2012; 32:122–138Crossref, Medline, Google Scholar
172 : Parenting behaviors and posttraumatic symptoms in relation to children’s symptomatology following a traumatic event. J Trauma Stress 2010; 23:403–407Crossref, Medline, Google Scholar
173 : The role of parenting behaviors in childhood post-traumatic stress disorder: a meta-analytic review. Clin Psychol Rev 2017; 53:1–13Crossref, Medline, Google Scholar
174 : Normative range parenting and the developing brain: a scoping review and recommendations for future research. Eur J Neurosci (Online ahead of print, October 14, 2020) Google Scholar
175 : Maternal care in infancy and the course of limbic development. Dev Cogn Neurosci 2019; 40:100714Crossref, Medline, Google Scholar
176 : The influence of maternal parenting style on the neural correlates of emotion processing in children. J Am Acad Child Adolesc Psychiatry 2020; 59:274–282Crossref, Medline, Google Scholar
177 : Maternal overprotection in childhood is associated with amygdala reactivity and structural connectivity in adulthood. Dev Cogn Neurosci 2019; 40:100711Crossref, Medline, Google Scholar
178 : Parental buffering in the context of poverty: positive parenting behaviors differentiate young children’s stress reactivity profiles. Dev Psychopathol 2020; 32:1778–1787Crossref, Medline, Google Scholar
179 : Role of positive parenting in the association between neighborhood social disadvantage and brain development across adolescence. JAMA Psychiatry 2017; 74:824–832Crossref, Medline, Google Scholar
180 : The protective effects of supportive parenting on the relationship between adolescent poverty and resting-state functional brain connectivity during adulthood. Psychol Sci 2019; 30:1040–1049Crossref, Medline, Google Scholar
181 : Protective prevention effects on the association of poverty with brain development. JAMA Pediatr 2017; 171:46–52Crossref, Medline, Google Scholar
182 : Maternal meta-emotion philosophy moderates effect of maternal symptomatology on preschoolers exposed to domestic violence. J Child Fam Stud 2017; 26:1831–1843Crossref, Google Scholar
183 : Parental buffering of stress in the time of COVID-19: family-level factors may moderate the association between pandemic-related stress and youth symptomatology. Res Child Adolesc Psychopathol 2021; 49:935–948Crossref, Medline, Google Scholar
184 : Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull 2001; 127:87–127Crossref, Medline, Google Scholar
185 : Parental socialization of emotion. Psychol Inq 1998; 9:241–273Crossref, Medline, Google Scholar
186 : Maternal presence serves as a switch between learning fear and attraction in infancy. Nat Neurosci 2006; 9:1004–1006Crossref, Medline, Google Scholar
187 : The impact of early adverse care on HPA axis development: nonhuman primate models. Horm Behav 2006; 50:623–631Crossref, Medline, Google Scholar
188 : Parent support is less effective in buffering cortisol stress reactivity for adolescents compared to children. Dev Sci 2015; 18:281–297Crossref, Medline, Google Scholar
189 : Maternal buffering of human amygdala-prefrontal circuitry during childhood but not during adolescence. Psychol Sci 2014; 25:2067–2078Crossref, Medline, Google Scholar
190 : Psychobiological mechanisms underlying the social buffering of the hypothalamic-pituitary-adrenocortical axis: a review of animal models and human studies across development. Psychol Bull 2014; 140:256–282Crossref, Medline, Google Scholar
191 : Decreased amygdala reactivity to parent cues protects against anxiety following early adversity: an examination across 3 years. Biol Psychiatry Cogn Neurosci Neuroimaging 2019; 4:664–671Crossref, Medline, Google Scholar
192 : Neurobiology of maternal regulation of infant fear: the role of mesolimbic dopamine and its disruption by maltreatment. Neuropsychopharmacology 2019; 44:1247–1257Crossref, Medline, Google Scholar
193 : Infant trauma alters social buffering of threat learning: emerging role of prefrontal cortex in preadolescence. Front Behav Neurosci 2019; 13:132Crossref, Medline, Google Scholar
194 : Social buffering of stress responses in nonhuman primates: maternal regulation of the development of emotional regulatory brain circuits. Soc Neurosci 2015; 10:512–526Crossref, Medline, Google Scholar
195 : Pubertal recalibration of cortisol reactivity following early life stress: a cross-sectional analysis. J Child Psychol Psychiatry 2019; 60:566–575Crossref, Medline, Google Scholar
196 : Pubertal stress recalibration reverses the effects of early life stress in postinstitutionalized children. Proc Natl Acad Sci USA 2019; 116:23984–23988Crossref, Medline, Google Scholar
197 : The pubertal stress recalibration hypothesis: potential neural and behavioral consequences. Child Dev Perspect (Online ahead of print, August 24, 2021)Google Scholar
198 : The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl 2004; 28:771–784Crossref, Medline, Google Scholar
199 : Poly-victimization: a neglected component in child victimization. Child Abuse Negl 2007; 31:7–26Crossref, Medline, Google Scholar
200 : Toward an experimental ecology of human development. Am Psychol 1977; 32:513–531Crossref, Google Scholar
201 : Toward an ecological/transactional model of community violence and child maltreatment: consequences for children’s development. Psychiatry 1993; 56:96–118Crossref, Medline, Google Scholar
202 : An ecological approach to understanding the developing brain: examples linking poverty, parenting, neighborhoods, and the brain. Am Psychol 2020; 75:1245–1259Crossref, Medline, Google Scholar
203 : Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry 2019; 76:584–593Crossref, Medline, Google Scholar
204 : Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nat Hum Behav 2020; 4:811–818Crossref, Medline, Google Scholar
205 : Toward understanding how early-life stress reprograms cognitive and emotional brain networks. Neuropsychopharmacology 2016; 41:197–206Crossref, Medline, Google Scholar
206 : Understanding the potency of stressful early life experiences on brain and body function. Metabolism 2008; 57(suppl 2):S11–S15Crossref, Medline, Google Scholar
207 : Nonhuman primate models of neuropsychiatric disorders: influences of early rearing, genetics, and epigenetics. ILAR J 2014; 55:361–370Crossref, Medline, Google Scholar
208 : Nonhuman primate models to study anxiety, emotion regulation, and psychopathology. Ann N Y Acad Sci 2003; 1008:189–200Crossref, Medline, Google Scholar
209 : Early adversity and developmental outcomes: interaction between genetics, epigenetics, and social experiences across the life span. Perspect Psychol Sci 2010; 5:564–574Crossref, Medline, Google Scholar
210 : Early life stress, physiology, and genetics: a review. Front Psychol 2019; 10:1668Crossref, Medline, Google Scholar
211 : Research review: the neurobiology and genetics of maltreatment and adversity. J Child Psychol Psychiatry 2010; 51:1079–1095Crossref, Medline, Google Scholar
212 : Disruptive behavior disorders: the challenge of delineating mechanisms in the face of heterogeneity. Am J Psychiatry 2020; 177:811–817Link, Google Scholar
213 : Socio-emotional development following early abuse and neglect: challenges and insights from translational research, in Handbook of Developmental Social Neuroscience. Edited by Haan M, Gunnar MR. New York, Guilford, 2009, pp 497–520Google Scholar
214 : Lasting epigenetic influence of early-life adversity on the BDNF gene. Biol Psychiatry 2009; 65:760–769Crossref, Medline, Google Scholar
215 : Early-life adversity and neurological disease: age-old questions and novel answers. Nat Rev Neurol 2019; 15:657–669Crossref, Medline, Google Scholar
216 : Unraveling the epigenetic landscape of depression: focus on early life stress. Dialogues Clin Neurosci 2019; 21:341–357Crossref, Medline, Google Scholar
217 : Emerging roles of epigenetic mechanisms in the enduring effects of early-life stress and experience on learning and memory. Neurobiol Learn Mem 2011; 96:79–88Crossref, Medline, Google Scholar
218 : Epigenetic programming by maternal behavior. Nat Neurosci 2004; 7:847–854Crossref, Medline, Google Scholar
219 : Evolutionarily conserved prefrontal-amygdalar dysfunction in early-life anxiety. Mol Psychiatry 2014; 19:915–922Crossref, Medline, Google Scholar
220 : Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry 2016; 173:1083–1093Link, Google Scholar
221 : Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron 2005; 48:175–187Crossref, Medline, Google Scholar
222 : Using a developmental ecology framework to align fear neurobiology across species. Annu Rev Clin Psychol 2019; 15:345–369Crossref, Medline, Google Scholar
223 : Looking back and moving forward: evaluating and advancing translation from animal models to human studies of early life stress and DNA methylation. Dev Psychobiol 2019; 61:323–340Crossref, Medline, Google Scholar
224 : Bundling the haystack to find the needle: challenges and opportunities in modeling risk and resilience following early life stress. Front Neuroendocrinol 2019; 54:100768Crossref, Medline, Google Scholar
225 : FAAH genetic variation enhances fronto-amygdala function in mouse and human. Nat Commun 2015; 6:6395Crossref, Medline, Google Scholar
226 : Ventral hippocampus interacts with prelimbic cortex during inhibition of threat response via learned safety in both mice and humans. Proc Natl Acad Sci USA 2019; 116:26970–26979Crossref, Medline, Google Scholar
227 : Elevated infant cortisol is necessary but not sufficient for transmission of environmental risk to infant social development: cross-species evidence of mother-infant physiological social transmission. Dev Psychopathol 2020; 32:1696–1714Crossref, Medline, Google Scholar
228 : Modeling developmental change: contemporary approaches to key methodological challenges in developmental neuroimaging. Dev Cogn Neurosci 2018; 33:1–4Crossref, Medline, Google Scholar
229 : Insensitive parenting may accelerate the development of the amygdala-medial prefrontal cortex circuit. Dev Psychopathol 2017; 29:505–518Crossref, Medline, Google Scholar
230 : An open resource for transdiagnostic research in pediatric mental health and learning disorders. Sci Data 2017; 4:170181Crossref, Medline, Google Scholar
231 : Brain function and clinical characterization in the Boston Adolescent Neuroimaging of Depression and Anxiety Study. Neuroimage Clin 2020; 27:102240Crossref, Medline, Google Scholar
232 : The Generation R Study: design and cohort profile. Eur J Epidemiol 2006; 21:475–484Crossref, Medline, Google Scholar
233 : The Pediatric Imaging, Neurocognition, and Genetics (PING) data repository. Neuroimage 2016; 124(Pt B):1149–1154Crossref, Medline, Google Scholar
234 : Large, open datasets for human connectomics research: considerations for reproducible and responsible data use. Neuroimage 2021; 244:118579Crossref, Medline, Google Scholar
235 : The NKI-Rockland sample: a model for accelerating the pace of discovery science in psychiatry. Front Neurosci 2012; 6:152Crossref, Medline, Google Scholar
236 : Cohort profile: the Saguenay Youth Study (SYS). Int J Epidemiol 2017; 46:e19Medline, Google Scholar
237 : High risk cohort study for psychiatric disorders in childhood: rationale, design, methods and preliminary results. Int J Methods Psychiatr Res 2015; 24:58–73Crossref, Medline, Google Scholar
238 : The Philadelphia Neurodevelopmental Cohort: a publicly available resource for the study of normal and abnormal brain development in youth. Neuroimage 2016; 124(Pt B):1115–1119Crossref, Medline, Google Scholar
239 : The IMAGEN study: reinforcement-related behaviour in normal brain function and psychopathology. Mol Psychiatry 2010; 15:1128–1139Crossref, Medline, Google Scholar
240 : The Lifespan Human Connectome Project in Development: a large-scale study of brain connectivity development in 5-21 year olds. Neuroimage 2018; 183:456–468Crossref, Medline, Google Scholar
241 : The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev Cogn Neurosci 2018; 32:4–7Crossref, Medline, Google Scholar
242 : Leveraging big data to map neurodevelopmental trajectories in pediatric anxiety. Dev Cogn Neurosci 2021; 50:100974Crossref, Medline, Google Scholar
243 : Scanning the horizon: towards transparent and reproducible neuroimaging research. Nat Rev Neurosci 2017; 18:115–126Crossref, Medline, Google Scholar
244 : Towards reproducible brain-wide association studies. bioRxiv, August 22, 2020 (https://doi.org/10.1101/2020.08.21.257758)Google Scholar
245 : Interactive impact of childhood maltreatment, depression, and age on cortical brain structure: mega-analytic findings from a large multi-site cohort. Psychol Med 2020; 50:1020–1031Crossref, Medline, Google Scholar
246 : Deconstructing and reconstructing resilience: a dynamic network approach. Perspect Psychol Sci 2019; 14:765–777Crossref, Medline, Google Scholar
247 : Individual and environmental correlates of childhood maltreatment and exposure to community violence: utilizing a latent profile and a multilevel meta-analytic approach. Psychol Med (Online ahead of print, June 2, 2021) Google Scholar
248 : Decomposing complex links between the childhood environment and brain structure in school-aged youth. Dev Cogn Neurosci 2021; 48:100919Crossref, Medline, Google Scholar
249 : Network structure reveals clusters of associations between childhood adversities and development outcomes. Dev Sci 2020; 23:e12934Crossref, Medline, Google Scholar
250 : A developmental reduction of the excitation:inhibition ratio in association cortex during adolescence. bioRxiv, May 20, 2021 (https://doi.org/10.1101/2021.05.19.444703)Google Scholar
251 : Critical period plasticity in local cortical circuits. Nat Rev Neurosci 2005; 6:877–888Crossref, Medline, Google Scholar
252 : Critical period regulation across multiple timescales. Proc Natl Acad Sci USA 2020; 117:23242–23251Crossref, Medline, Google Scholar
253 : Inhibitory circuit gating of auditory critical-period plasticity. Nat Neurosci 2018; 21:218–227Crossref, Medline, Google Scholar
254 : The complex neurobiology of resilient functioning after child maltreatment. BMC Med 2020; 18:32Crossref, Medline, Google Scholar
255 : Equifinality and multifinality in developmental psychopathology. Dev Psychopathol 1996; 8:597–600Crossref, Google Scholar
256 : A developmental psychopathology perspective on child abuse and neglect. J Am Acad Child Adolesc Psychiatry 1995; 34:541–565Crossref, Medline, Google Scholar
257 : Developmental cascades. Dev Psychopathol 2010; 22:491–495Crossref, Medline, Google Scholar
258 : On stress and subjectivity. Theory Psychol 2021; 31:254–272Crossref, Google Scholar
259 : Adolescents’ perceptions of family social status correlate with health and life chances: a twin difference longitudinal cohort study. Proc Natl Acad Sci USA 2020; 117:23323–23328Crossref, Medline, Google Scholar
260 : Neurodevelopmental optimization after early-life adversity: cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci 2020; 43:744–751Google Scholar
261 : Modeling the evolution of sensitive periods. Dev Cogn Neurosci 2020; 41:100715Crossref, Medline, Google Scholar
262 : Experience and brain development. Child Dev 1987; 58:539–559Crossref, Medline, Google Scholar
263 : Early life adversity during the infant sensitive period for attachment: programming of behavioral neurobiology of threat processing and social behavior. Dev Cogn Neurosci 2017; 25:145–159Crossref, Medline, Google Scholar
264 : The stress response systems: universality and adaptive individual differences. Dev Rev 2006; 26:175–212Crossref, Google Scholar
265 : Beyond risk and protective factors: an adaptation-based approach to resilience. Perspect Psychol Sci 2017; 12:561–587Crossref, Medline, Google Scholar
266 : Toward a balanced view of stress-adapted cognition. Behav Brain Sci 2017; 40:e325Crossref, Medline, Google Scholar
267 : Sensitive periods of emotion regulation: influences of parental care on frontoamygdala circuitry and plasticity. New Dir Child Adolesc Dev 2016; 2016:87–110Crossref, Medline, Google Scholar
268 : Developmental adaptation to stress: an evolutionary perspective. Annu Rev Psychol 2019; 70:111–139Crossref, Medline, Google Scholar
269 : Hidden talents in harsh environments. Dev Psychopathol (Online ahead of print, July 16, 2020) Google Scholar
270 : The hidden talents approach: theoretical and methodological challenges. Trends Cogn Sci 2020; 24:569–581Crossref, Medline, Google Scholar
271 : Responsible use of open-access developmental data: the Adolescent Brain Cognitive Development (ABCD) Study. Psychol Sci 2021; 32:866–870Crossref, Medline, Google Scholar
272 : Trauma-focused cognitive-behavioral therapy for children and adolescents: assessing the evidence. Psychiatr Serv 2014; 65:591–602Link, Google Scholar
273 : The data behind the dissemination: a systematic review of trauma-focused cognitive behavioral therapy for use with children and youth. Child Youth Serv Rev 2012; 34:748–757Crossref, Google Scholar
274 : Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. J Clin Child Adolesc Psychol 2017; 46:303–330Crossref, Medline, Google Scholar
275 : Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. J Clin Child Adolesc Psychol 2008; 37:105–130Crossref, Medline, Google Scholar
276 : Treatment of posttraumatic stress disorder in children and adolescents. Curr Opin Psychiatry 2013; 26:66–72Crossref, Medline, Google Scholar
277 : Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Syst Rev 2016; 10:CD012371Medline, Google Scholar
278 : Early adversity in chronic depression: clinical correlates and response to pharmacotherapy. Depress Anxiety 2009; 26:701–710Crossref, Medline, Google Scholar
279 : Chronic harsh parenting and anxiety associations with fear circuitry function in healthy adolescents: a preliminary study. Biol Psychol 2019; 145:198–210Crossref, Medline, Google Scholar
280 : Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry 2013; 170:1114–1133Link, Google Scholar
281 : Differential involvement of the medial prefrontal cortex in the expression of learned fear across development. Behav Neurosci 2012; 126:217–225Crossref, Medline, Google Scholar
282 : Impaired extinction retention in adolescent rats: effects of d-cycloserine. Neuropsychopharmacology 2010; 35:2134–2142Crossref, Medline, Google Scholar
283 : Multimodal evidence for delayed threat extinction learning in adolescence and young adulthood. Sci Rep 2019; 9:7748Crossref, Medline, Google Scholar
284 : Altered fear learning across development in both mouse and human. Proc Natl Acad Sci USA 2012; 109:16318–16323Crossref, Medline, Google Scholar
285 : vlPFC-vmPFC-Amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cereb Cortex 2017; 27:3502–3514Medline, Google Scholar
286 : Treating the developing versus developed brain: translating preclinical mouse and human studies. Neuron 2015; 86:1358–1368Crossref, Medline, Google Scholar
287 : Adolescent mental health: opportunity and obligation. Science 2014; 346:547–549Crossref, Medline, Google Scholar
288 : Mechanisms linking childhood adversity with psychopathology: learning as an intervention target. Behav Res Ther 2019; 118:101–109Crossref, Medline, Google Scholar
289 : Translational neuroscience measures of fear conditioning across development: applications to high-risk children and adolescents. Biol Mood Anxiety Disord 2013; 3:17Crossref, Medline, Google Scholar
290 : Sensitive periods in affective development: nonlinear maturation of fear learning. Neuropsychopharmacology 2015; 40:50–60Crossref, Medline, Google Scholar
291 : Translating developmental neuroscience to understand risk for psychiatric disorders. Am J Psychiatry 2019; 176:179–185Link, Google Scholar
292 : Maturational changes in prefrontal and amygdala circuits in adolescence: implications for understanding fear inhibition during a vulnerable period of development. Brain Sci 2019; 9:65Crossref, Google Scholar
293 : Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol 2009; 77:566–579Crossref, Medline, Google Scholar
294 : State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Philos Trans R Soc Lond B Biol Sci 2018; 373:20170025Google Scholar
295 : Trauma-focused cognitive-behavioral therapy: the role of caregivers. J Affect Disord 2020; 277:39–45Crossref, Medline, Google Scholar
296 : Treatments for early childhood trauma: decision considerations for clinicians. J Child Adolesc Trauma 2018; 12:515–528Crossref, Medline, Google Scholar