In This Issue
Step Therapy Savings on Antidepressants Are Offset by Higher Medical Spending
Requiring initial use of a lower-cost antidepressant before approval of a more expensive one, i.e., “step therapy,” decreases the cost of antidepressant drugs initially but is accompanied by increased expenses for inpatient and emergency room treatment. Mark et al. (p. Original article: 1202) compared health care expenditures for antidepressant users employed by two large companies using step therapy and by two companies without it. Not only did step therapy result in higher total payments to providers soon after implementation of step therapy, the difference increased over the next 2 years. During the same period, the advantage in prescription drug spending decreased. Dr. John Greden points out in an editorial (p. Original article: 1148) that requirements such as step therapy result in lower adherence to prescribed treatments.
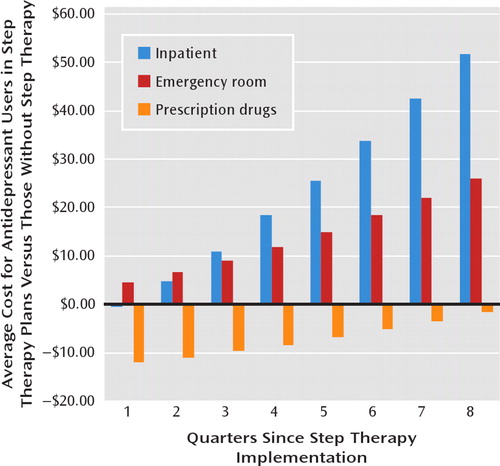
Costs increased both in general and for mental health conditions specifically with step therapy (Mark et al., p. 1202)
Children under 5 years of age in the pediatric intensive care unit may develop delirium as a consequence of the presence and treatment of severe medical illnesses. Silver et al. (CME, p. Original article: 1172) illustrate the evaluation and treatment of delirium in this age group with the case of an 8-month-old girl. Symptoms, which include disorientation, agitated behavior, and failure to respond to parents, can be rated on the Pediatric Anesthesia Emergence Delirium Scale. Intravenous haloperidol (0.05 to 0.15 mg/kg daily in divided doses) can be used if cardiac risk is not present. Second-generation antipsychotics are also recommended.
Flashbacks from childhood or adult sexual trauma can trigger suicidal and nonsuicidal self-injurious behavior in chronically suicidal women with co-occurring borderline personality disorder and PTSD, according to Harned et al. (p. Original article: 1210). Use of the behavior for interpersonal needs, emotional numbing from the PTSD, and comorbid panic disorder possibly contribute to these behaviors. Treatment should be directed toward reducing trauma cue reactivity, as well as developing tolerance skills and substituting alternative, nonharmful behaviors. In an editorial (p. Original article: 1152), Dr. Burr Eichelman notes that this study provides evidence that PTSD causes psychopathology that is distinct from borderline personality disorder.
Hypertension and increased body mass index, common concomitants of the weight gain induced by antipsychotic medications, are associated with decreased immediate and delayed memory in schizophrenia. Friedman et al.(CME, p. Original article: 1232) found that these neurocognitive deficits are associated with decreased psychosocial function in patients with schizophrenia. Addressing hypertension and obesity in patients may therefore improve disabling neuro-cognitive deficits that are not otherwise amenable to treatment. Dr. Henry Nasrallah states in an editorial (p. Original article: 1155) that prevention of weight loss is critical for optimal therapeutic response for schizophrenia.
Part A of APA's Major Depressive Disorder Practice Guideline accompanies this issue as a supplement



