In This Issue
Childhood Fearlessness and Adult Crime
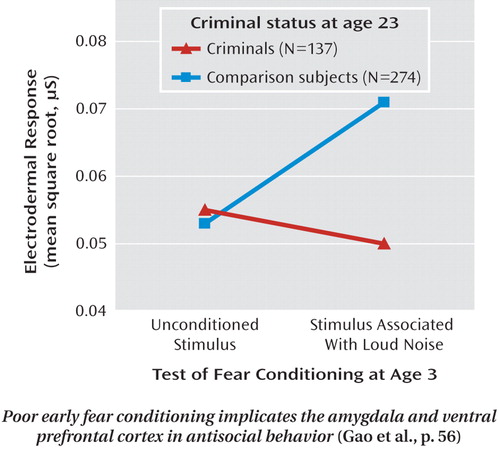
Gao et al. (CME, p. Original article: 56) present evidence that early brain dysfunction contributes to later antisocial behavior. Learning to associate a cue with a frightening outcome, known as fear conditioning, relies on prefrontal cortex regulation of an amygdala response. Among 1,795 3-year-old children tested for fear conditioning, 137 had convictions for serious offenses by age 23. Noncriminal subjects matched for ethnicity, gender, and social adversity showed normal fear conditioning at age 3, but the children who became criminals showed significantly reduced fear conditioning. Dr. Philipp Sterzer expands on the neurobiology of antisocial behavior in an editorial on p. Original article: 1.
Differentiating ADHD, Bipolar Disorder, and Severe Mood Dysregulation in Children
Fear-related activation of the left amygdala was greater in children and adolescents with attention deficit hyperactivity disorder (ADHD) than in healthy youth, but it was lower than normal in those with the chronic irritability known as severe mood dysregulation. Youth with bipolar disorder did not differ from the comparison subjects. Brotman et al. (p. Original article: 61) sought to differentiate childhood bipolar disorder, severe mood dysregulation, and ADHD because diagnosis is hindered by their shared characteristics, such as hyperarousal. Although fear-related activation was low in the group with severe mood dysregulation, their self-ratings of fear were higher than those of the comparison group. Dr. Mary Phillips notes important aspects of the study in an editorial on p. Original article: 4.
Mother's Prenatal Depression Adds to Familial Risk for Psychosis in Her Offspring
Mäki et al. (p. Original article: 70) asked mothers of 12,058 children in Finland were asked during pregnancy whether they felt depressed. A national hospital discharge registry provided data on parental and offspring hospitalizations for psychoses over the next 35 years. Prenatal maternal depressed mood alone was not associated with a higher than average risk for psychosis, and parental psychosis itself tripled the risk. However, the risk in offspring with both maternal depressed mood during pregnancy and parental psychosis was eight times as great as the risk for offspring with neither of these factors. Dr. John Gilmore discusses these findings in an editorial on p. Original article: 8.
Treatment of Comorbid PTSD Decreases Comorbid Substance Use
Integrated treatment for women with concurrent posttraumatic stress disorder (PTSD) and substance use disorder was associated with a decrease in PTSD symptoms and a subsequent reduction in substance use. However, the reverse was not observed: patients who had an early decrease in substance use did not show later improvement in PTSD. Hien et al. (p. Original article: 95) assigned 353 women to 12 sessions of either cognitive-behavioral therapy with both trauma and substance use components or health education. Among those with heavy baseline substance use and decreases in PTSD symptoms during the intervention, integrated treatment was more effective than health education in reducing substance use over the following year. Clinical implications are highlighted by Dr. Sudie Back in an editorial on p. Original article: 11.
Clinical Guidance: Treatment of Methamphetamine Psychosis
Methamphetamine psychosis often resolves spontaneously when patients become abstinent, but over 25% of patients have psychotic symptoms lasting more than 6 months. Rapid recurrence upon re-exposure to methamphetamine is also common. Evidence for response of these persistent cases to treatment with neuroleptic drugs is lacking. The case of a patient who responded to ECT is presented in this month's Clinical Case Conference (Grelotti et al., p. Original article: 17).



