The Outcome of Bulimia Nervosa: Findings From One-Quarter Century of Research
Abstract
Objective: The present review addresses the outcome of bulimia nervosa, effect variables, and prognostic factors. Method: A total of 79 study series covering 5,653 patients suffering from bulimia nervosa were analyzed with regard to recovery, improvement, chronicity, crossover to another eating disorder, mortality, and comorbid psychiatric disorders at outcome. Forty-nine studies dealt with prognosis only. Final analyses on prognostic factors were based on 4,639 patients. Results: Joint analyses of data were hampered by a lack of standardized outcome criteria. There were large variations in the outcome parameters across studies. Based on 27 studies with three outcome criteria (recovery, improvement, chronicity), close to 45% of the patients on average showed full recovery of bulimia nervosa, whereas 27% on average improved considerably and nearly 23% on average had a chronic protracted course. Crossover to another eating disorder at the follow-up evaluation in 23 studies amounted to a mean of 22.5%. The crude mortality rate was 0.32%, and other psychiatric disorders at outcome were very common. Among various variables of effect, duration of follow-up had the largest effect size. The data suggest a curvilinear course, with highest recovery rates between 4 and 9 years of follow-up evaluation and reverse peaks for both improvement and chronicity, including rates of crossover to another eating disorder, before 4 years and after 10 years of follow-up evaluation. For most prognostic factors, there was only conflicting evidence. Conclusions: One-quarter of a century of specific research in bulimia nervosa shows that the disorder still has an unsatisfactory outcome in many patients. More refined interventions may contribute to more favorable outcomes in the future.
The introduction and definition of bulimia nervosa were presented only 30 years ago. In his salient publication, Gerald Russell (1) emphasized the dread of overeating, various compensatory measures, and the morbid fear of gaining weight and getting fat. Within this relatively short period of time, a remarkably large number of outcome studies have been published. Early reviews included one review based on eight studies (2) and another on 24 follow-up studies (3) . The latter found a mean recovery rate of 47.5% and mean rates of 26% for both improvement and chronicity. Shortly before the turn of the century, Keel and Mitchell (4) analyzed the course of 56 patient series and found a recovery rate of 50% and chronicity in 20% of the patients. The mortality rate of 0.3% was slightly lower than that reported in the prior review of 24 studies (3) . The review by Vaz (5) concentrated on prognostic factors only, and Quadflieg and Fichter (6) reviewed various outcome measures in a total of 33 studies. Finally, a recent, more selective review based on very rigorous inclusion criteria by Berkman et al. (7) provided findings from 13 patient series. Steinhausen’s analysis (8) of the outcome of anorexia nervosa in the second half of the last century served as a model for the present review.
Method
Selection criteria for the inclusion of studies in the present review were 1) data on at least one out of five outcome measures for bulimia nervosa after a minimum follow-up evaluation period of 6 months following the treatment episode and/or 2) data on any prognostic factor of the disorder. The aforementioned reviews consisted of a total of 141 studies. A systematic search with various databases was performed using the terms “bulimia nervosa,” “outcome,” “follow-up,” and “prognosis.” A search using PubMed led to an additional 60 studies, and a search using PsycINFO resulted in 19 studies. Thus, before applying any exclusion criteria, a total of 220 published studies were available. As a result of duplicate or review-type studies, 68 studies were excluded. Furthermore, 26 studies did not include sufficient information on the duration of follow-up evaluation or provided pre-post measures only or were based only on follow-up periods <6 months. In another 21 studies, information on the course of the disorder was insufficient (e.g., no information on sample size or no independent assessment of anorexia and bulimia nervosa patients was provided). Finally, there were 14 studies dealing with prognostic factors only, and another 12 studies presented additional data based on the same patient cohort. Thus, at the end, a total of 79 patient series were entered into the analyses for the outcome of bulimia nervosa in the present review. Findings were published between 1981 and 2007. Data based on reports from a total of 32 studies were extracted by the expert senior author. Decisions on the inclusion of the remaining studies were jointly made by both the junior and senior authors.
Study Characteristics
The 79 published reports (9 – 87) were composed of 5,653 patients (group mean size=71.6 [SD=113.4], range=4–884). There were considerable differences in design, group size, methods, duration of follow-up evaluation, and missing data. Diagnostic classification changed considerably over the period in which the studies were conducted. Since the 1990s, there has been an increasing reliance on DSM-IV and ICD-10 criteria. In 46 studies consisting of 2,508 patients, the mean age at onset was 17.2 years (SD=1.7, range=4.3–23.2), and the mean age at follow-up assessment was 28.4 years (SD=4.3, range=16.6–38.0) in 39 studies consisting of 2,478 patients. The mean duration of follow-up evaluation varied between 6 months and 12.5 years (mean=3.2 months [SD=3.3]) in 77 studies of 5,239 patients. In 66 studies of 3,830 patients, a total of 75 men (1.9%) were included.
A minority of studies used combined intervention and follow-up evaluation, whereas the majority of studies used only limited evaluation of treatment effects. The available information on treatment was classified as 1) nonbehavioral psychotherapy, 2) unspecified medical intervention, 3) cognitive-behavioral therapy (CBT), 4) family intervention, or 5) mixed or uncontrolled intervention.
In the analyses for prognostic factors, 35 studies included information on prognostic factors in addition to data on outcome (10 , 14 , 15 , 17 , 21 , 24 , 25 , 30 , 34 – 36 , 40 – 44 , 52 , 54 , 55 , 57 , 61 , 63 , 65 , 68 , 71 – 73 , 75 , 76 , 83 , 88 – 92) , and 14 studies (93 – 106) dealt exclusively with prognostic factors. The total sample of these studies on prognosis consisted of 4,639 patients (mean=94.62 [SD=133.76], range=4–884).
Outcome Measures
The five central outcome criteria for the present analyses were recovery, improvement, chronicity, mortality, and crossover to other eating disorders. In addition, information on comorbid mental disorders was collected. Information on recovery was provided in the studies as part of 1) a three-level classification in combination with improvement and chronicity, 2) a two-level classification mostly in combination with chronicity, or 3) a single criterion. There were 22 synonyms of recovery (e.g., “abstinent”). Improvement was most commonly used as a medium category of a three-level classification. In a few instances, rates of improvement were reported in combination with recovery only. Among the 27 synonyms of improvement were terms such as “intermediate course,” “some remaining symptoms,” or “partial remission.” Finally, among 21 synonyms of chronicity, the most common were “bulimia nervosa,” and “poor course.” Some studies used crossover to another eating disorder according to DSM-IV criteria as an outcome category in addition to recovery and chronicity. All mortality rates represented crude mortality rates. None of the studies reported standardized mortality rates.
Statistical Analyses
The five outcome measures were calculated in percentages that were rounded to the nearest whole value. In order to take into account the large variation in sample sizes, weighted percentages were calculated by weighting each reported rate with the size of the study group. Data for all studies were converted into individual data for performance of statistical analyses using SPSS 14 (SPSS, Chicago).
All analyses were based on adjusted sample sizes at follow-up assessments rather than actual sample sizes after patient recruitment. Differences between these two figures were considered the dropout rate. The latter was dichotomized into high (≥16% of the original sample) and low (0%–15% of the original sample) categories and served as a first independent effect variable. In accordance with previous analyses (8) , the duration of follow-up evaluations was the second independent effect variable and categorized as <4 years, 4 to 9 years, or ≥10 years. Studies with a variable length of course were not considered for analyses of effect. In case there was more than one report based on the same cohort, only the last report with the longest duration of follow-up assessment was considered for the analyses. The third independent variable was represented by the type of intervention. Because of limited data, the aforementioned classification of available information on treatment into five types was restricted to the following three types: nonbehavioral psychotherapy, unspecified medical therapy, and CBT.
Effects of these three variables for treatment type on four outcome measures were analyzed using multivariate analyses of variance. In addition, effect sizes were calculated using partial eta-squared (η 2 ) as a measure of association between independent and dependent variables. According to Cohen (107) , η 2 =0.01–0.059 represents a small effect, η 2 =0.06–0.13 represents a median effect, and there is a large effect starting with η 2 =0.14. Furthermore, the frequencies of positive, negative, and insignificant prognostic factors were calculated.
Results
Main Outcome Findings
The main findings on outcome are presented in Table 1 . Twenty-seven studies used a three-level classification of global outcome (recovery, improvement, chronicity), supplemented by additional information on rates of crossover to another eating disorder in six studies. According to this procedure, close to 45% of the patients on average showed full recovery from bulimia nervosa, whereas 27% on average improved considerably and nearly 23% on average had a chronic protracted course. In another 27 studies, only two outcome parameters were used. Nineteen of these studies used recovery and chronicity, supplemented by additional information on rates of crossover as an indicator of the course of illness in nine studies. In these studies, recovery increased to almost 60% on average, 30% of patients on average had a chronic course, and 10% on average were marked by crossover to another eating disorder. Eight studies used a two-level classification (recovery and improvement) and found a mean of 42% of patients on average to be recovered and 41% on average to be improved. There was no information on crossover to another eating disorder in addition to a rather substantial amount of missing outcome data. Twenty-five studies used a single outcome criterion only. Among these studies, the mean recovery rate was 42% on average in 15 studies, whereas the mean improvement rate was two-thirds on average in two studies and chronicity was nearly 51% on average in eight studies. Eight of the 25 studies provided additional information on crossover to another eating disorder, which was almost 32% on average.
Detailed information on crossover diagnoses was available in 23 studies. As shown in Table 1 , more than one-fifth of the patients fulfilled this criterion, with a majority of 16% on average crossing over to eating disorder not otherwise specified, which in most cases was a subclinical manifestation of bulimia nervosa, and nearly 6% on average developed full anorexia nervosa. A few patients developed binge eating disorder.
Seventy-six studies reported on mortality, and there were 14 deaths among 4,309 patients, leading to a crude mortality rate of 0.32%. For two patients, car accidents were the cause of death, four deaths were the result of suicide, one death was the result of a drug overdose, two deaths were caused by an eating disorder, and no causes of death were given for two subjects.
There was a large list of reported comorbid mental disorders. At follow-up assessments, patients most frequently suffered from affective disorders, followed by neurotic disorders (mostly anxiety disorders). Nonspecific personality disorders and borderline personality disorder were also frequent. Substance use disorders were less frequently seen, and obsessive-compulsive and schizophrenia spectrum disorders were described only in a single study.
Findings From Repeated Follow-Up Assessments
A few studies shed some light on the differential course of bulimia nervosa across time. Fichter and Quadflieg (91) published findings after 2-, 6-, and 12-year follow-up evaluations (34) and found substantial improvement in patients who completed longer follow-up assessment periods. Similarly, in the study by Herzog et al. (42) , recovery rates increased between the first follow-up assessment after 2 years and the second follow-up assessment after 7 years, but rates of improvement and chronicity declined correspondingly. Another study on intervention (59) found that the reduction of binge eating episodes and compensatory vomiting and laxative abuse remained constant between the 6- and 12-month follow-up evaluations. A change in outcome rates was observed in two smaller studies. Nevonen and Broberg (64) found a decreased recovery rate and an increased improvement rate between 1 and 2.5 years of follow-up evaluation when comparing individual and group psychotherapy. Similarly, in a very small sample of six patients, Toro et al. (80) observed that all patients were recovered at the first follow-up evaluation, but only four patients remained recovered after 25 years.
Intervention Effects on Outcome
There are various intervention studies on bulimia nervosa that include follow-up assessments. Two studies (28 , 30) compared three types of interventions and found that both interpersonal therapy and CBT were superior to behavior therapy without cognitive components. Other studies reported that CBT was superior to interpersonal therapy (29 , 84) or found no significant differences in the effects of either CBT or the combination of behavior therapy and hypnotherapy (40) . In another study (12) , more patients became symptom-free by the use of a self-help manual rather than CBT. Physical activity, but not diet counseling, was shown to be superior to CBT in one report (78) .
In a study on the optimization of CBT (82) , one group of patients used a self-help manual and received additional CBT when necessary. The other patients received behavior therapy only. There were no significant differences between these two approaches. In a study on the effectiveness of either the antidepressant fluoxetine or interpersonal therapy after a first inefficient phase of CBT (62) , no significant differences between the two approaches were found.
When comparing the effects of the antidepressant desipramine, CBT, or a combination of both measures (11) , CBT or the combined intervention resulted in stronger reduction of symptoms after 24 weeks relative to the pure antidepressant treatment. Adding exposure and response prevention to CBT did not result in improved results (19) . Another study (59) revealed that relative to a coping with stress program, diet counseling led to a more rapid improvement of eating behavior and to reduction and abstinence of binge eating episodes.
Two studies on the effects of family therapy revealed contradictory findings. One study (74) found that family intervention was inferior to individual psychotherapy, whereas family therapy was found to be superior in another study (39) . No significant differences were found in the effectiveness of group versus individual psychotherapy (64) . Finally, a positive effect of after-treatment control visits on the course of bulimia nervosa has been documented (58) .
Effect Variables
As a result of methodological restrictions, the presentation of findings based on effect analyses was limited to the set of 27 studies that used the three-level classification with recovery, improvement, and chronicity, supplemented by the smaller number of studies that provided additional information on rates of diagnoses for crossover to other eating disorders. There were no missing data in this data set.
Dropout rate
The dropout rate had a strong effect on rates of recovery and crossover diagnoses ( Table 2 ). The rate of recovered patients at follow-up evaluations was lower in studies with high dropout rates, and the reverse pattern was true for the rate of crossover. There was a medium effect size for the rate of improvement and no significant effect for chronicity.
Duration of follow-up evaluation
The effect of duration of follow-up evaluation was robust among the three effect variables. The effect size for recovery, chronicity, and crossover was strong but medium for improvement ( Table 3 , Figure 1 ). Post hoc comparisons indicated that the recovery rate was strongest after 4 years of the course of bulimia nervosa but less robust before 4 years and later at ≥10 years. The rates of improvement and the number of patients with a chronic course of the disorder were highest before 4 years of follow-up evaluation. A considerable number of crossover diagnoses were only seen in patients with long-term follow-up assessment >10 years.
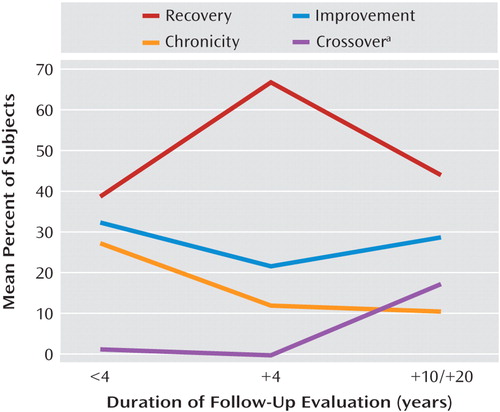
a Data represent crossover to other eating disorders.
Type of intervention
In general, the effects of outcome of intervention in a small sample of 10 patient series were strong. There was a clear gradient of effects for recovery with psychotherapy, which ranked highest, followed by medical therapy and behavior therapy ( Table 4 , Figure 2 ). The gradient effect for improvement was highest with behavior therapy, followed by medical therapy and psychotherapy, and there was no real eminent difference in the proportion of patients with chronic illness across intervention types except that it was higher for behavior therapy than nonbehavioral psychotherapy. The effect of treatment type on chronicity was weak. Crossover was observed most frequently with behavior therapy, less frequently with medical therapy, and not at all with psychotherapy.
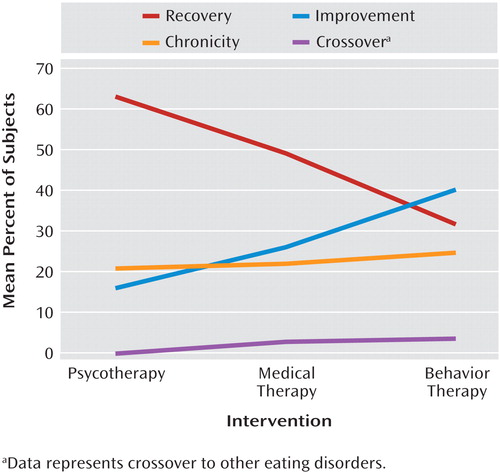
a Data represent crossover to other eating disorders.
Prognostic Factors
In general, many prognostic factors of bulimia nervosa have been evaluated in the literature. Findings were grouped into various categories as follows:
Specific characteristics of bulimia nervosa
Duration of the disorder has been assessed in most studies, finding no effect on the course of illness. In five studies (25 , 54 , 71 , 88 , 90) , a short duration was beneficial, whereas it was negative in one study (105) . Similarly, most of the studies did not find a significant association between age at onset and outcome. Only in three studies (10 , 21 , 34) was a young age at onset favorable for the outcome. Various indicators of severity did not show a clear association with the outcome of bulimia nervosa. Only two studies (63 , 73) found that frequent binge eating episodes were related to poor outcome. Four studies (25 , 63 , 65 , 105) showed the same association for purging behavior, whereas one study (31) identified laxative abuse as a positive prognostic factor. Predominant vomiting was a negative factor in one study (25) but insignificant in another study (10) . Restrictive dieting was not a significant factor in any study.
An overemphasis on weight and body shape was a negative prognostic factor in three studies (88 , 89 , 101) , whereas it was insignificant in three other studies (30 , 63 , 97) . Furthermore, no significant associations with outcome were found for low ideal weight (25 , 52) , maximum and minimum body weight, or body mass index prior to treatment (10 , 25 , 52 , 65) . Weight fluctuations were considered to have a positive effect in one study (31) and a negative effect in another study (63) .
Additional patient characteristics
The findings on the effect of age were mostly heterogeneous. Older age was found to be a negative prognostic factor in one study (73) , a positive factor in two studies (25 , 65) , and nonsignificant in six studies (10 , 42 , 54 , 61 , 71 , 101) . Advanced academic education (24) and having children (21) or giving birth to a child (96) were not found to be significantly associated with follow-up status.
One study addressed the effect of either current or past premorbid anorexia nervosa and found no influence of these conditions on the course of bulimia nervosa (43) . Two studies examined coexisting personality disorders and, particularly, the effect of borderline personality disorder. Although Johnson et al. (51) found a negative effect of borderline and nonborderline personality disorders on the course of bulimia nervosa, this was not fully replicated in the study by Steiger and Stotland (75) . In the latter study, personality disorders were associated more strongly with general psychiatric symptoms rather than with the course of bulimia nervosa. The differentiation between patients with or without treatment with imipramine (24) did not lead to significant differences in the course of bulimia nervosa.
Introversion (91) , perfectionism (91) , neuroticism (76) , and emotional lability (91) were not significant in terms of prognosis. One study found that low self-esteem had a negative effect on the course of bulimia nervosa (108) , but six other studies did not replicate this finding (30 , 65 , 88 , 91 , 97 , 103) . Patients seeking social support during the first month of treatment experienced a more favorable course (94) , and adaptive coping contributed to recovery (106) .
No association was found between obsessive or various impulsive features and the course of the disorder (25 , 52) . Patients with multi-impulsive behaviors, including self-injury behaviors and substance use disorders, had a worse course than those without these behaviors (98) . Findings on the effect of suicidal behaviors were contradictory, with two studies implying a negative prognostic function (10 , 25) and four studies failing to replicate this finding (15 , 42 , 43 , 52) . Cue reactivity, in terms of reacting by binge eating after presentations of food, was found not to be a significant prognostic factor in one study (95) , but it was a negative predictor in another study (17) .
Patient history
Only two studies found that a history of anorexia nervosa was an unfavorable prognostic sign (34 , 57) , and there was no indication that premorbid eating disorders in early infancy had any effect (76) . However, a premorbid overweight condition was considered as both an impediment to a favorable course (17 , 30 , 88) and a nonsignificant factor (34 , 76 , 91 , 97) . Two studies found that depressive symptoms before treatment of bulimia nervosa had a negative effect (17 , 92) . Most studies did not find a significant association between a substance use disorder and the course of bulimia nervosa, with only two studies finding a negative effect (54 , 57) and one study finding a positive effect (17) .
Among a large list of comorbid mental disorders, none of the various axis I disorders and only a single axis II disorder showed a significant negative association with outcome (25) . Only the combination of all comorbidities had a significant negative effect in a single study (34) , which was not replicated in another study (91) . Furthermore, frequent hospitalizations (25 , 52 , 101) and treatment of other diagnoses (10 , 30 , 42 , 52 , 61 , 71 , 76) did not imply poor response to treatment of bulimia nervosa.
Family history and environment
The search for family history and environment variables with an effect on the course of bulimia nervosa resulted in only a few significant findings. No significant associations were found for affective disorders (25 , 30 , 52 , 71 , 90) or eating disorders in patients’ family history (21 , 30 , 52 , 90) or for any parental psychopathology (15 , 30 , 90) . Nonsignificant findings were obtained for parental socioeconomic status (52) , sexual abuse (30 , 90) , and quality of family bonding (30) . However, a single study (90) found that physical maltreatment within a controlling family environment lacking support and affection contributed to an unfavorable course of bulimia nervosa.
A family history of obesity (30 , 73) and disturbed family relationships (73) had a negative effect on outcome, whereas the findings for substance use disorders were heterogeneous. Four studies revealed nonsignificant findings for substance use disorders (30 , 52 , 90 , 91) , one study identified substance use disorders as favorable prognostic factors (21) , and another study (15) identified substance use disorders as unfavorable prognostic factors.
Social Factors
Positive social adjustment (88) , close social relationships (55) , and high socioeconomic status (21) were all identified as positive prognostic factors, whereas a high amount of psychosocial distress (72 , 73) and low job status (72) were considered negative factors.
Treatment Factors
Neither previous outpatient (34 , 52 , 63) nor hospital treatment (10 , 52) had a significant effect on the course of bulimia nervosa. However, poor motivation at treatment onset was an unfavorable prognostic factor in one study (102) . A rapid reduction in symptoms during the first 4 weeks of treatment was linked to a positive course (15 , 97) , but the number of treatment sessions was not significant (35) . Continuous dieting and overemphasis on weight and body shape after treatment were clearly linked to a negative course of the disorder (17 , 35 , 88) . Furthermore, continuous treatment after hospital discharge was associated with a poor prognosis in two studies (92 , 102) and found to be nonsignificant in another study (76) .
Discussion
Similar to the previous extended review by Steinhausen (8) on the course and outcome of anorexia nervosa, the present review on the course and outcome of bulimia nervosa was based on the largest database currently available and was not confined to descriptive statistics, which was the case in most prior reviews. Using methods of inferential statistics, an attempt was also made to isolate factors that might have influenced the course of bulimia nervosa. Findings were based on a large group of 5,653 patients on whom data were published in little more than one-quarter of a century. In the Steinhausen review, a similar number of patients suffering from anorexia nervosa (N=5,590) was studied within one-half a century. Thus, the intensity of studying the outcome of bulimia nervosa has been very strong. Furthermore, it has to be noted that the present review was based on published data on patients who had been seen predominantly by expert groups. However, as long as there are no reports from other sources, such as community physicians, it is impossible to conclude whether or not the present findings are biased as a result of patient selection.
The discussion of the main outcome findings was severely hampered by a lack of commonly accepted outcome criteria. Different three- and two-level classifications or single criteria for the outcome of bulimia nervosa were presented in the literature. Given the wide acceptance of the distinction among recovery, improvement, and chronicity as classification of the global outcome of diseases in general, and in the previous review by Steinhausen on the course of anorexia nervosa in particular (8) , findings based on this classification should be considered those with the highest face value. Within this scheme, findings on mean recovery rates for bulimia nervosa (45%) and anorexia nervosa (46%) (8) were remarkably similar. In addition, the mean improvement rates (bulimia nervosa, 27%, versus anorexia nervosa, 33%) and mean chronicity rates (bulimia nervosa, 23%, versus anorexia nervosa, 20%) were not extremely different in these two largest reviews. However, it needs to be mentioned that, first, these figures represented only a central tendency, and there was a large variation across studies in both reviews. Second, the different criteria of outcome on the course of bulimia nervosa in the studies add to the uncertainty of the data. Thus, studies relying on other schemes of classification resulted in higher or similar mean rates of recovery or higher mean rates of improvement and chronicity. There is no meta-analytical strategy to overcome these different findings because they are rooted in basic differences of the studies.
According to the present review, crossover to other eating disorders in the course of bulimia nervosa is very common. However, as a result of differences in the design of the outcome criteria of the studies, it was difficult to identify precisely the mean rate of crossover diagnoses, which was between a 10% and 32% range, depending on the criteria for the outcome. Obviously, the most common crossover at follow-up evaluations was to eating disorder not otherwise specified, followed by anorexia nervosa, and the least common crossover was to binge eating disorder. However, the low rate of binge eating disorder may be partially the result of underreporting because the term was not yet introduced when many of the older outcome studies were performed.
With a mean crude mortality rate of 0.32%, including a number of deaths not caused by bulimia nervosa, bulimia nervosa was definitely less fatal than anorexia nervosa, which resulted in a mean crude mortality rate of 5% in the review by Steinhausen (8) . However, the frequencies of comorbid psychiatric disorders were high for both disorders. Affective and neurotic/anxiety disorders ranked highest, and there was a sizable proportion of patients with personality disorders at follow-up evaluations. Although the crude figures for comorbid disorders were higher for anorexia nervosa, these differences should not be overestimated because many studies did not clearly indicate the criteria for assessment or diagnosis.
Several conclusions may be drawn from the present analyses of three central variables (dropout rate, duration of follow-up evaluation, and type of intervention) with an effect on outcome. First, there is some evidence that, perhaps counter to expectation, patients who dropped out of follow-up studies may have had a more favorable course of bulimia nervosa. Staying in the follow-up cohort may reflect patients’ continuous need for further treatment. Thus, one might argue that the outcome of representative samples of patients without sample loss may be more favorable than delineated from the present data.
Second, duration of follow-up evaluation was the variable with the strongest effect on outcome. The distribution of data did not allow for a more fine-grained analysis, particularly for ≤4 years of follow-up evaluation. The profiles shown in Figure 1 clearly indicate a curvilinear course of bulimia nervosa, particularly if one considers the curve representing crossover diagnoses to be a part of the chronic course of illness. It is also obvious that the mean recovery rate peaked in the 4- to 9-year follow-up interval and declined thereafter, whereas the rates for chronicity and crossover followed the reverse pattern and the rates of improvement remained relatively stable across time. According to these data, the developmental trajectory of bulimia nervosa in the present analyses was rather different from the course of anorexia nervosa in the previous review by Steinhausen (8) , which showed a linear relationship indicating better outcome with increasing duration of follow-up evaluation. However, it needs to be taken into consideration that these data were derived from a composition of cross-sectional samples only. The few larger longitudinal bulimia nervosa outcome studies with repeated assessments over extended follow-up periods tended to show a more favorable course with increasing duration of follow-up evaluation (34 , 42) . However, these findings may not be representative because they were based on patients who had been treated in expert centers.
Third, both the analyses of effect variables and of intervention studies allow for conclusions on the role of treatment for bulimia nervosa. This is in contrast to the studies on anorexia nervosa, which included a paucity of facts on the effect of interventions on outcome (8) . In the entire data set of studies in the present analyses, there were strong effects indicating a clear superiority of psychotherapy over medical therapy and behavior therapy. However, this finding was overshadowed by a lack of clear description of the type and modalities of treatment employed in the various studies. Furthermore, as a result of methodological shortcomings and/or contradictory findings, intervention studies provided only limited evidence regarding which treatments actually may contribute to a positive outcome. Standards of intervention studies, such as controlled randomization or a waiting comparison group analysis, are almost entirely missing in the literature because of problems with clinical practicality. At least for CBT, there is some limited evidence that it may contribute to more favorable outcomes for bulimia nervosa. Clearly, this field is in need of more sophisticated research.
Finally, there was a large number of studies dealing with prognostic factors in various domains. Despite the considerable effort that was invested in this area of research, the majority of these factors did not prove to have any significant effect on the disorder. Only a few of the significant factors were replicated, and many studies resulted in contradictory findings. Information on prediction models, excluded variables, or nonsignificant factors was mostly missing in the reports. Most frequently, prognostic factors were seen in isolation. In the outcome literature on anorexia nervosa, it was shown that favorable, unfavorable, or nonsignificant prognostic factors may be extracted from the various study reports (8) . However, multivariate analyses with consideration of a large group of factors in a large sample of patients with anorexia nervosa have clearly shown that very few variables actually have an effect on outcome if their covariation is considered (109) . Thus, most of the findings on prognostic factors of bulimia nervosa must be considered as insufficiently controlled. Certainly, this field also is in need of further refinement of research. From the existing literature, a concentration on treatment factors seems most promising. However, one has to consider the likely nature of study data that preclude any delineation of rules for individual prognosis for a given patient.
In conclusion, the present comprehensive review of one-quarter of a century of outcome research shows that bulimia nervosa remains a serious disorder with unsatisfactory recovery and improvement rates and high rates of patients who continue to have chronic eating disorder problems and other comorbid psychiatric disorders over extended periods of their lives. Future research efforts could benefit from more collaborative and prospective studies based on large unselected samples and standardized assessment procedures using a common set of operationalized criteria of outcome. Refined study designs should particularly focus on the role of intervention in the long-term outcome of the disorder so that research might also identify beneficial effects on the course of the individual patient.
1. Russell G: Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 1979; 9:429–448Google Scholar
2. Rathner G: Aspects of the natural history of normal and disordered eating and some methodological considerations, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 273–301Google Scholar
3. Steinhausen H-C: Eating disorders, in Risks and Outcomes in Developmental Psychopathology. Edited by Steinhausen H-C, Verhulst FC. Oxford, UK, Oxford University Press, 1996, pp 210–330Google Scholar
4. Keel PK, Mitchell JE: Outcome in bulimia nervosa. Am J Psychiatry 1997; 54:313–321Google Scholar
5. Vaz FJ: Outcome of bulimia nervosa: prognostic indicators. J Psychosom Res 1998; 45:391–400Google Scholar
6. Quadflieg N, Fichter MM: The course and outcome of bulimia nervosa. Eur Child Adolesc Psychiatry 2003; 12:99–109Google Scholar
7. Berkman NB, Lohr KN, Bulik CM: Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord 2007; 40:293–309Google Scholar
8. Steinhausen H-C: The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 2002; 159:1284–1293Google Scholar
9. Abraham SF: Sexuality and reproduction in bulimia nervosa patients over 10 years. J Psychosom Res 1998; 44:491–502Google Scholar
10. Abraham SF, Mira M, Llewellyn-Jones D: Bulimia: a study of outcome. Int J Eat Disord 1983; 2:175–180Google Scholar
11. Agras WS, Rossiter EM, Arnow B, Telch CF, Raeburn SD, Bruce B, Koran LM: One-year follow-up of psychosocial and pharmacologic treatments for bulimia nervosa. J Clin Psychiatry 1994; 55:179–183Google Scholar
12. Bailer U, de Zwaan M, Leisch F, Strnad A, Lennkh-Wolfsberg C, El-Giamal N, Hornik K, Kasper S: Guided self-help versus cognitive-behavioral group therapy in the treatment of bulimia nervosa. Int J Eat Disord 2004; 35:522–537Google Scholar
13. Banasiak SJ, Paxton SJ, Hay P: Guided self-help for bulimia nervosa in primary care: a randomized controlled trial. Psychol Med 2005; 35:1283–1294Google Scholar
14. Ben-Tovim D, Walker K, Freeman R, Kalucy R, Esterman A: Outcome in patients with eating disorders: a 5-year study. Lancet 2001; 357:1254–1257Google Scholar
15. Bogh EH, Rokkedal K, Valbak K: A 4-year follow-up on bulimia nervosa. Eur Eat Disord Rev 2005; 13:48–53Google Scholar
16. Brotman AW, Herzog DB, Hamburg P: Long-term course in 14 bulimic patients treated with psychotherapy. J Clin Psychiatry 1988; 49:157–160Google Scholar
17. Bulik CM, Sullivan PF, Joyce PR, Carter RA, McIntosh VV: Predictors of 1-year treatment outcome in bulimia nervosa. Compr Psychiatry 1998; 39:206–214Google Scholar
18. Carter FA, McIntosh VV, Joyce PR, Frampton CM, Bulik CM: Cue reactivity in bulimia nervosa: a useful self-report approach. Int J Eat Disord 2006; 39:694–699Google Scholar
19. Carter FA, McIntosh VV, Joyce PR, Sullivan PF, Bulik CM: Role exposure with response prevention in cognitive-behavioral therapy for bulimia nervosa: three-year follow-up results. Int J Eat Disord 2003; 33:127–135Google Scholar
20. Chen E, Touyz SW, Beumont PJ, Fairburn CG, Griffiths R, Butow P, Russell J, Schotte DE, Gertler R, Basten C: Comparison of group and individual cognitive-behavioral therapy for patients with bulimia nervosa. Int J Eat Disord 2003; 33:241–254Google Scholar
21. Collings S, King M: Ten-year follow-up of 50 patients with bulimia nervosa. Br J Psychiatry 1994; 164:80–87Google Scholar
22. Connors ME, Johnson CL, Stuckey NK: Treatment of bulimia with brief psychoeducational group therapy. Am J Psychiatry 1984; 141:1512–1516Google Scholar
23. Drewnowski A, Yee DK, Kurth CL, Krahn DD: Eating pathology and DSM-III-R bulimia nervosa: a continuum of behavior. Am J Psychiatry 1994; 151:1217–1219Google Scholar
24. Edelstein CK, Yager J, Gitlin M, Landsverk J: A clinical study of antidepressant medications in the treatment of bulimia. Psychiatr Med 1989; 7:111–121Google Scholar
25. Fahy TA, Russell GF: Outcome and prognostic variables in bulimia nervosa. Int J Eat Disord 1993; 14:135–145Google Scholar
26. Fairburn CG: A cognitive-behavioural approach to the management of bulimia. Psychol Med 1981; 11:707–711Google Scholar
27. Fairburn CG, Cooper Z, Doll HA, Norman P, O’Connor M: The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry 2000; 57:659–665Google Scholar
28. Fairburn CG, Jones R, Peveler RC, Hope RA, O’Connor M: Psychotherapy and bulimia nervosa: longer-term effects of interpersonal psychotherapy, behavior therapy and cognitive behavior therapy. Arch Gen Psychiatry 1993; 50:419–428Google Scholar
29. Fairburn CG, Kirk J, O’Connor M, Cooper PJ: A comparison of two psychological treatments for bulimia nervosa. Behav Res Therapy 1986; 24:629–643Google Scholar
30. Fairburn CG, Norman PA, Welch SL, O’Connor ME, Doll HA, Peveler RC: A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Arch Gen Psychiatry 1995; 52:304–312Google Scholar
31. Fallon BA, Walsh BT, Sadik C, Saoud JB, Lukasik V: Outcome and clinical course in inpatient bulimic women: a 2- to 9-year follow-up study. J Clin Psychiatry 1991; 52:272–278Google Scholar
32. Fichter MM, Quadflieg N, Rief W: The German Longitudinal Bulimia Nervosa Study, in The Course of Eating Disorders: Long-Term Follow-up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 133–149Google Scholar
33. Fichter MM, Quadflieg N: Course and two-year outcome in anorexic and bulimic adolescents. J Youth Adolesc 1996; 25:546–560Google Scholar
34. Fichter MM, Quadflieg N: Twelve-year course and outcome of bulimia nervosa. Psychol Med 2004; 34:1395–1406Google Scholar
35. Freeman RJ, Beach B, Davis R, Solyom L: The prediction of relapse in bulimia nervosa. J Psychiatr Res 1985; 19:349–353Google Scholar
36. Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM: Thyroid indices and treatment outcome in bulimia nervosa. Acta Psychiatr Scand 2003; 108:190–195Google Scholar
37. Ghaderi A: Does individualization matter? A randomized trial of standardized (focused) versus individualized (broad) cognitive behavior therapy for bulimia nervosa. Behav Res Therapy 2006; 44:273–288Google Scholar
38. Giles TR, Young RR, Young DE: Case studies and clinical replication series: behavioral treatment of severe bulimia. Behav Therapy 1985; 16:393–405Google Scholar
39. Ie Grange D, Crosby RD, Rathouz PJ, Leventhal BL: A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch Gen Psychiatry 2007; 64:1049–1056Google Scholar
40. Griffiths R, Channon-Little L, Hadzi-Pavlovic D: Hypnotizablility and outcome in the treatment of bulimia nervosa. Contemp Hypnosis 1995; 12:165–172Google Scholar
41. Grilo CM, Sanislow CA, Shea MT, Skodol AE, Stout RL, Pagano ME, Yen S, McGlashan TH: The natural course of bulimia nervosa and eating disorder not otherwise specified is not influenced by personality disorders. Int J Eat Disord 2003; 34:319–330Google Scholar
42. Herzog DB, Dorrer D, Keel PK, Selwyn SE, Ekeblad E, Flores AT, Greenwood DN, Burwell RA, Keller MB: Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study. J Am Acad Child Adolesc Psychiatry 1999; 38:829–837Google Scholar
43. Herzog DB, Field AE, Keller MB, West JC, Robbins WM, Staley J, Colditz GA: Subtyping eating disorders: Is it justified? J Am Acad Child Adolesc Psychiatry 1996; 35:928–936Google Scholar
44. Herzog DB, Keller MB, Lavori PW, Ott IL: Short-term prospective study of recovery in bulimia nervosa. Psychiatry Res 1988; 23:45–55Google Scholar
45. Herzog DB, Sacks NR, Keller MB, Lavori PW, Ranson KB, Gray HM: Patterns and predictors of recovery in anorexia nervosa and bulimia nervosa. J Am Acad Child Adolesc Psychiatry 1993; 32:835–842Google Scholar
46. Hsu LK: Treatment of bulimia with lithium. Am J Psychiatry 1984; 141:1260–1262Google Scholar
47. Hsu LK, Sobkiewicz TA: Bulimia nervosa: a four- to six-year follow-up study. Psychol Med 1989; 19:1035–1038Google Scholar
48. Hudson JI, Pope HG Jr, Keck PE Jr, McElroy SL: Treatment of bulimia nervosa with trazodone: short-term response and long-term follow-up. Clin Neuropharmacol 1989; 12:S38–S46Google Scholar
49. Huon GF, Brown LB: Evaluating a group treatment for bulimia. J Psychiatr Res 1985; 19:479–483Google Scholar
50. Jäger B, Liedtke R, Lamprecht F, Freyberger H: Social and health adjustment of bulimic women 7 to 9 years following therapy. Acta Psychiatr Scand 2004; 110:138–145Google Scholar
51. Johnson C, Tobin DL, Dennis A: Differences in treatment outcome between borderline and nonborderline bulimics at one-year follow-up. Int J Eat Disord 1990; 9:617–626Google Scholar
52. Johnson-Sabine E, Reiss D, Dayson D: Bulimia nervosa: a 5-year follow-up study. Psychol Med 1992; 22:951–959Google Scholar
53. Keel PK, Mitchell JE, Davis TL, Crow SJ: Long-term impact of treatment in women diagnosed with bulimia nervosa. Int J Eat Disord 2002; 31:151–158Google Scholar
54. Keel PK, Mitchell JE, Miller KB, Davis TL, Crow SJ: Long-term outcome of bulimia nervosa. Arch Gen Psychiatry 1999; 56:63–69Google Scholar
55. Keller MB, Herzog DB, Lavori PW, Bradburn IS, Mahoney EM: The naturalistic history of bulimia nervosa: extraordinarily high rates of chronicity, relapse, recurrence and psychological morbidity. Int J Eat Disord 1992; 12:1–9Google Scholar
56. King M: The natural history of eating pathology in attenders to primary medical care. Int J Eat Disord 1991; 10:379–387Google Scholar
57. Lacey JH: Bulimia nervosa, binge eating and psychogenic vomiting: a controlled treatment study and long-term outcome. BMJ 1983; 286:1609–1613Google Scholar
58. Lacey JH: Long-term follow-up of bulimic patients treated in integrated behavioural and psychodynamic treatment programmes, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 150–173Google Scholar
59. Laessle RG, Beumont PJ, Butow P, Lennerts W, O’Connor ME, Pirke KM, Touyz SW, Waadt S: A comparison of nutritional management with stress management in the treatment of bulimia nervosa. Br J Psychiatry 1991; 159:250–261Google Scholar
60. Maddocks SE, Kaplan AS, Woodside DB, Langdon L, Piran N: Two year follow-up of bulimia nervosa: the importance of abstinence as the criterion of outcome. Int J Eat Disord 1992; 12:133–141Google Scholar
61. Mitchell JE, Davis L, Goff G, Pyle RL: A follow-up study of patients with bulimia. Int J Eat Disord 1986; 5:441–450Google Scholar
62. Mitchell JE, Halmi K, Wilson GT, Agras WS, Kraemer H, Crow S: A randomized secondary treatment study of women with bulimia nervosa who fail to respond to CBT. Int J Eat Disord 2002; 32:271–281Google Scholar
63. Mitchell JE, Pyle RL, Hatsukami D, Goff G, Glotter D, Harper J: A 2 to 5 year follow-up study of patients treated for bulimia. Int J Eat Disord 1988; 8:157–165Google Scholar
64. Nevonen L, Broberg AG: A comparison of sequenced individual and group psychotherapy for patients with bulimia nervosa. Int J Eat Disord 2006; 39:117–127Google Scholar
65. Olmsted MP, Kaplan AS, Rockert W: Rate and prediction of relapse in bulimia nervosa. Am J Psychiatry 1994; 151:738–743Google Scholar
66. Olmsted MP, Kaplan AS, Rockert W: Defining remission and relapse in bulimia nervosa. Int J Eat Disord 2005; 38:1–6Google Scholar
67. Openshaw C, Waller G, Sperlinger D: Group cognitive-behavior therapy for bulimia nervosa: statistical versus clinical significance of changes in symptoms across treatment. Int J Eat Disord 2004; 36:363–375Google Scholar
68. Peterson CB, Wimmer S, Ackard DM, Crosby RD, Cavanagh LC, Engbloom S, Mitchell JE: Changes in body image during cognitive-behavioral treatment in women with bulimia nervosa. Body Image 2004; 1:139–153Google Scholar
69. Pope HG, Hudson JI, Jonas JM, Yurgelun-Todd D: Antidepressant treatment of bulimia: a two-year follow-up study. J Clin Psychopharmacol 1985; 5:320–327Google Scholar
70. Pyle RL, Mitchell JE, Eckert ED, Hatsukami D, Pomeroy C, Zimmerman R: Maintenance treatment and 6-month outcome for bulimic patients who respond to initial treatment. Am J Psychiatry 1990; 147:871–875Google Scholar
71. Reas DL, Williamson DA, Martin CK, Zucker NL: Duration of illness predicts outcome for bulimia nervosa: a long-term follow-up study. Int J Eat Disord 2000; 27:428–434Google Scholar
72. Reiss D, Johnson-Sabine E: Bulimia nervosa: 5-year social outcome and relationship to eating pathology. Int J Eat Disord 1995; 18:127–133Google Scholar
73. Richard M: Effective treatment of eating disorders in Europe: treatment outcome and its predictors. Eur Eat Disord Rev 2005; 13:169–179Google Scholar
74. Russell GF, Szmukler GI, Dare C, Eisler I: An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1987; 44:1047–1056Google Scholar
75. Steiger H, Stotland S: Prospective study of outcome in bulimics as a function of axis-II comorbidity: long-term responses on eating and psychiatric symptoms. Int J Eat Disord 1996; 20:149–161Google Scholar
76. Steinhausen H-C, Seidel R: Outcome in adolescent eating disorders. Int J Eat Disord 1993; 14:487–496Google Scholar
77. Stevens EV, Salisbury JD: Group therapy for bulimic adults. Am J Orthopsychiatry 1984; 54:156–161Google Scholar
78. Sundgot-Borgen J, Rosenvinge JH, Bahr R, Sundgot-Schneider L: The effect of exercise, cognitive therapy and nutritional counseling in treating bulimia nervosa. Med Sci Sport Exer 2002; 34:190–194Google Scholar
79. Swift WJ, Ritzholz M, Kalin NH, Kaslow N: A follow-up study of thirty hospitalized bulimics. Psychosom Med 1987; 49:45–55Google Scholar
80. Toro J, Cervera M, Feliu MH, Garriga N, Jou M, Martinez E, Toro E: Cue exposure in the treatment of resistant bulimia nervosa. Int J Eat Disord 2003; 34:227–234Google Scholar
81. Tozzi F, Thornton LM, Klump KL, Fichter MM, Halmi K, Kaplan AS, Strober M, Woodside DB, Crow SJ, Mitchell JE, Rotondo A, Mauri M, Cassano G, Keel PK, Plotnicov KH, Pollice C, Lilenfeld LR, Berettini WH, Bulik CM, Kaye WH: Symptom fluctuation in eating disorders: correlates of diagnostic crossover. Am J Psychiatry 2005; 162:732–740Google Scholar
82. Treasure J, Schmidt U, Troop N, Tiller J, Todd G, Turnbull S: Sequential treatment for bulimia nervosa incorporating a self-care manual. Br J Psychiatry 1996; 168:94–98Google Scholar
83. Tseng MC, Lee MB, Lee YJ, Chen YY: Long-term outcome of bulimia nervosa in Taiwanese. J Formos Med Assoc 2004; 103:701–706Google Scholar
84. Wilson GT, Agras WS, Fairburn CG, Walsh BT, Kraemer H: Cognitive behavior therapy for bulimia nervosa: time course and mechanisms of change. J Consult Clin Psychol 2002; 70:267–274Google Scholar
85. Yager J, Landsverk J, Edelstein CK: A 20-month follow-up study of 628 women with eating disorders, II: course and severity. Am J Psychiatry 1987; 144:1172–1177Google Scholar
86. Yashkov YI, Bekuzaro DK: Effectiveness of biliopancreatic diversion in the patients with bulimia nervosa. Obes Surg 2006; 16:1433–1439Google Scholar
87. Zeeck A, Herzog T, Hartmann A: Day clinic or inpatient care for severe bulimia nervosa. Eur Eat Disord Rev 2004; 12:79–86Google Scholar
88. Fairburn CG, Cooper Z, Doll HA, Norman PA, O’Connor ME: Understanding persistence in bulimia nervosa: a 5-year naturalistic study. J Consult Clin Psychol 2003; 71:103–109Google Scholar
89. Fairburn CG, Peveler RC, Jones R, Hope RA, Doll HA: Predictors of 12-month outcome in bulimia nervosa and the influence of attitudes to shape and weight. J Consult Clin Psychol 1993; 61:696–698Google Scholar
90. Fallon BA, Sadik C, Saoud JB, Garfinkel RS: Childhood abuse, family environment, and outcome in bulimia nervosa. J Clin Psychiatry 1994; 55:424–428Google Scholar
91. Fichter MM, Quadflieg N: Six-year course of bulimia nervosa. Int J Eat Disord 1997; 22:361–384Google Scholar
92. Swift WJ, Kalin NH, Wamboldt FS, Kaslow N, Ritholz M: Depression in bulimia at 2- to 5-year follow-up. Psychiatry Res 1985; 16:111–122Google Scholar
93. Anderson CB, Joyce PR, Carter FA, McIntosh VV, Bulik CM: The effect of cognitive-behavioral therapy for bulimia nervosa on temperament and character as measured by the Temperament and Character Inventory. Compr Psychiatry 2002; 43:182–188Google Scholar
94. Binford RB, Crosby RD, Mussell MP, Peterson CB, Crow SJ: Coping strategies in bulimia nervosa treatment: impact on outcome in group cognitive-behavioral therapy. J Consult Clin Psychol 2005; 73:1089–1096Google Scholar
95. Carter FA, Bulik CM, McIntosh VV, Joyce PR: Cue reactivity as a predictor of outcome with bulimia nervosa. Int J Eat Disord 2002; 31:240–250Google Scholar
96. Carter FA, McIntosh VV, Joyce PR, Frampton CM, Bulik CM: Bulimia nervosa, childbirth and psychopathology. J Psychosom Res 2003; 55:357–361Google Scholar
97. Fairburn CG, Agras WS, Walsh BT, Wilson GT, Stice E: Prediction of outcome in bulimia nervosa by early change in treatment. Am J Psychiatry 2004; 161:2322–2324Google Scholar
98. Fichter MM, Quadflieg N, Rief W: Course of multi-impulsive bulimia. Psychol Med 1994; 24:591–604Google Scholar
99. Herzog T, Hartmann A, Sanholz A, Stammer H: Prognostic factors in outpatient psychotherapy of bulimia. Psychother Psychosom 1991; 56:48–55Google Scholar
100. Joiner TE, Heatherton TF, Keel PK: Ten-year stability and predictive validity of five bulimia-related indicators. Am J Psychiatry 1997; 154:1133–1138Google Scholar
101. Keel PK, Dorer DJ, Franko DL, Jackson SC, Herzog DB: Postremission predictors of relapse in women with eating disorders. Am J Psychiatry 2005; 162:2263–2268Google Scholar
102. Richard M, Bauer S, Kordy H; COST Action B6: Relapse in anorexia and bulimia nervosa: a 2.5-year follow-up study. Eur Eat Disord Rev 2005; 13:180–190Google Scholar
103. Rossiter EM, Agras WS, Telch CF, Schneider JA: Cluster B personality disorder characteristics predict outcome in the treatment of bulimia nervosa. Int J Eat Disord 1993; 13:349–357Google Scholar
104. Thiel A, Züger M, Jacoby GE, Schüssler G: Thirty-month outcome in patients with anorexia or bulimia nervosa and concomitant obsessive-compulsive disorder. Am J Psychiatry 1998; 155:244–249Google Scholar
105. Turnbull S, Schmidt U, Troop NA, Tiller J, Todd G, Treasure JL: Predictors of outcome for two treatments for bulimia nervosa: short and long-term. Int J Eat Disord 1997; 21:17–22Google Scholar
106. Yager J, Rorty M, Rossotto E: Coping styles differ between recovered and nonrecovered women with bulimia nervosa, but not between recovered women and noneating-disordered control subjects. J Nerv Ment Dis 1995; 183:86–94Google Scholar
107. Cohen J: Statistical Power Analysis for the Behavioral Sciences. New York, Academic Press, 1977Google Scholar
108. Fairburn CG, Kirk J, O’Connor M, Anastasiades P, Cooper PJ: Prognostic factors in bulimia nervosa. Br J Clin Psychol 1987; 26(pt 3):223–224Google Scholar
109. Steinhausen H-C, Boyadjieva S, Griogoroiu-Serbanescu M, Neumärker KJ: The outcome of adolescent eating disorders: findings from an international collaborative study. Eur Child Adolesc Psychiatry 2003; 12(suppl 1):91–98Google Scholar







