Prefrontal Activation Deficits During Episodic Memory in Schizophrenia
Abstract
Objective: Episodic memory impairments represent a core deficit in schizophrenia that severely limits patients’ functional outcome. This quantitative meta-analysis of functional imaging studies of episodic encoding and retrieval tests the prediction that these deficits are most consistently associated with dysfunction in the prefrontal cortex. Method: Activation likelihood estimation (ALE) was used to perform a quantitative meta-analysis of functional imaging studies that contrasted patients with schizophrenia and healthy volunteers during episodic encoding and retrieval. From a pool of 36 potential studies, 18 whole-brain studies in standard space that included a healthy comparison sample and low-level baseline contrast were selected. Results: As predicted, patients showed less prefrontal activation than comparison subjects in the frontal pole, dorsolateral and ventrolateral prefrontal cortex during encoding, and the dorsolateral prefrontal cortex and ventrolateral prefrontal cortex during retrieval. The ventrolateral prefrontal cortex encoding deficits were not present in studies that provided patients with encoding strategies, but dorsolateral prefrontal cortex deficits remained and were not secondary to group performance differences. The only medial temporal lobe finding was relatively greater patient versus comparison subject activation in the parahippocampal gyrus during encoding and retrieval. Conclusions: The finding of prominent prefrontal dysfunction suggests that cognitive control deficits strongly contribute to episodic memory impairment in schizophrenia. Memory rehabilitation approaches developed for patients with frontal lobe lesions and pharmacotherapy approaches designed to improve prefrontal cortex function may therefore hold special promise for remediating memory deficits in patients with schizophrenia.
Individuals with schizophrenia have pronounced episodic memory impairments (1) that are not explained by demographic variables such as education or sex (2) or by clinical variables, including medication, duration, or severity of illness (3) . Deficits in unaffected first- and second-degree relatives (4 , 5) suggest that these impairments are genetically mediated. Since these deficits limit functional outcome (6) and do not respond well to available treatments (7) , there is increased interest in identifying neural mechanisms that can become targets for new treatment development. Two leading candidate brain regions are the hippocampus and prefrontal cortex.
Basic research has highlighted the importance of the hippocampus and surrounding medial temporal lobe for episodic memory. Interest in the medial temporal lobe was sparked by observation of marked anterograde amnesia produced by bilateral resection of this structure (8) , and subsequent studies of humans and animals with medial temporal lobe lesions (9) documented its importance in relational binding, memory consolidation, and retrieval. Accordingly, a great deal of research has tested the hypothesis that memory deficits in schizophrenia may be due in part to medial temporal lobe dysfunction. Consistent with this hypothesis, structural and molecular hippocampal abnormalities have been documented in schizophrenia (10 , 11) . However, these patients do not exhibit the classic amnesic syndrome typical of medial temporal lobe dysfunction (12 , 13) , suggesting that regions beyond this lobe may contribute to memory deficits in such patients.
Close examination of relative memory strengths and weaknesses in patients with schizophrenia reveals compelling parallels to patients with prefrontal cortex damage. Like patients with prefrontal cortex lesions (14) , individuals with schizophrenia do not spontaneously use semantic information to categorize related word lists during encoding (13 , 15) but benefit when strategies are provided (16 , 17) . Both groups also become more impaired as retrieval tasks become less structured and cognitive control demands increase (1 , 13) . These parallels, as well as evidence of structural and molecular abnormalities (18 – 20) in the prefrontal cortex of patients with schizophrenia, contribute to the idea that a breakdown in prefrontally mediated cognitive control mechanisms may lead to episodic memory impairment in schizophrenia (21) .
Functional imaging of episodic memory in schizophrenia has documented medial temporal lobe and prefrontal cortex dysfunction (22) , with some authors proposing a disruption in frontotemporal connectivity (23) . However, in meta-analytic (22) and qualitative (23) reviews, the majority of studies reveal group differences in the prefrontal cortex and not in the medial temporal lobe (23) . Moreover, many studies finding group medial temporal lobe differences rely on region-of-interest methods that restrict analysis to this specific region. Thus, a limitation of a previous activation likelihood estimation (ALE) meta-analysis (22) was the combination of whole-brain and region-of-interest studies, which may have biased results in favor of selected regions of interest. ALE is a voxel-based method for finding concordance across neuroimaging studies that does not rely on author-assigned anatomical labels (24 , 25) . Our goal in this ALE study is to limit analysis to whole-brain experiments while testing the prediction that reduced activation in patients with schizophrenia during episodic encoding and retrieval is most prominent in the prefrontal cortex.
Method
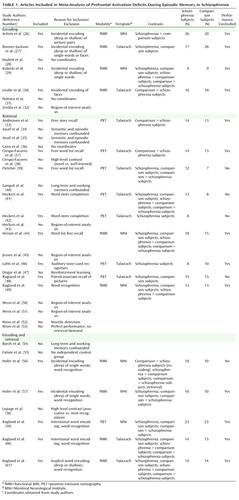
A PubMed search was conducted to identify functional MRI (fMRI) and positron emission tomography (PET) studies investigating episodic memory in patients with schizophrenia. The search identified 36 articles published through February 2008 that localized brain activity during encoding or retrieval of single stimuli (words, pictures, or tones), paired pictures, or word lists ( Table 1 ).
As a meta-analytic method, ALE identifies convergence across studies. However, this convergence depends on inclusion of studies that address a similar question and employ equivalent designs. The aim of the exclusions described below was to maintain a sufficient number of activation foci ( Table 2 ) while minimizing procedural differences. Accordingly, analyses were restricted to studies that employed incidental or intentional encoding tasks; examined retrieval using recognition, cued recall, or free recall tasks; and contrasted memory conditions with resting, visual fixation, or lower-level baseline tasks (e.g., word reading).
ALE produces convergence maps of brain activation by examining the probability that spatially smoothed activation foci from individual studies occur across multiple studies. This approach tests the null hypothesis that the location of activated foci is equal at every voxel against an alternative hypothesis that activated foci are spatially distributed. This null assumption is violated by region-of-interest studies because they do not provide results for all voxels in the brain. The need for studies to examine the whole brain eliminated five studies (32 , 43 , 45 , 50 , 51) . ALE also requires reporting of results in Talairach or Montreal Neurological Institute (MNI) coordinates, a requirement that eliminated three additional studies (28 , 31 , 36) . Four studies reported results only for higher-level contrasts (e.g., associative versus item encoding), and authors were contacted and asked whether they could provide lower-level baseline results. The authors of two studies (27 , 61) provided additional results, which were included in our analysis; the remaining two studies (38 , 58) were excluded. Four encoding studies (34 , 35 , 40 , 54) were omitted because memory was confounded with either semantic or working memory tasks in the same contrast, and two retrieval studies were omitted because they used measures of either reinforcement learning (47) or novelty detection (52) . An additional retrieval study was omitted because of absence of retrieval demands, as subjects had been practiced to perfect task performance (53) . Finally, one study was excluded because it lacked an independent comparison group (55) .
With these selection criteria, a sample of 18 articles was established ( Table 1 ). In two studies (33 , 37) patients were unmedicated at the time of testing. Coordinate (x, y, z) results from each study were divided into groups based on stage of memory processing: encoding (eight studies) and retrieval (14 studies). Encoding instructions were either intentional (e.g., “remember these items”) or incidental (deep versus shallow encoding). Incidental instructions were to make semantic discriminations, such as “abstract/concrete” during deep encoding, and perceptual discriminations, such as “uppercase/lowercase” during shallow encoding. Retrieval was tested with either “old”/“new” recognition tasks, cued recall (word stem completion), or free recall. Unlike in the previous ALE meta-analysis (22) , retrieval was not subdivided into high versus low performance because of an insufficient number of foci once region-of-interest studies were excluded. The number of foci was sufficient to perform a separate ALE analysis of incidental tasks in which an encoding strategy was provided. We also repeated between-group ALE analyses after excluding studies that did not control for group performance differences ( Table 1 ).
Encoding and retrieval contrasts were examined separately for within-group activations in schizophrenia patients and healthy comparison subjects, and for between-group comparisons (comparison subjects > schizophrenia patients and schizophrenia patients > comparison subjects). Coordinates using the MNI template were spatially renormalized to Talairach space using the Lancaster transform (62) . MNI coordinates in one study (44) had been converted to Talairach space using the Brett (mni2tal) transform (63) ; we therefore uncorrected and reconverted them using the Lancaster transform, which better reduces disparity between Talairach and MNI coordinates (62) .
ALE meta-analyses were performed on the contrasts specified in Table 2 using a full width at half maximum of 12 mm (24) in GingerALE 1.2, distributed by the BrainMap project (64 , 65) . Statistical significance was determined within GingerALE 1.2 using a permutation test of 5,000 permutations. ALE images were thresholded at significance level of 0.05, false-discovery-rate-corrected for multiple comparisons (66) , with a cluster extent threshold of 300 mm.
Results
Episodic Encoding
Healthy comparison subjects
Six studies reported activation for comparison subjects, resulting in 145 foci. Healthy participants activated 11 brain regions (see Table S1 in the data supplement that accompanies the online edition of this article), including the left middle (Brodmann’s area [BA] 46) and superior frontal gyri (BA 6), the inferior frontal gyrus bilaterally (BA 9, 44), the anterior cingulate gyrus (BA 24), the left superior parietal gyrus (BA 7, 40), the left inferior and right middle occipital gyrus (BA 18), the right insula (BA 13), and the cerebellum bilaterally.
Schizophrenia patients
Six studies reported encoding results for patients, resulting in 100 foci. As in comparison subjects, schizophrenia patients activated the left superior (BA 6) and the left and right inferior frontal gyri (BA 9, 44), the left superior parietal gyrus (BA 7), the left inferior (BA 18) and right middle occipital gyrus (BA 19), the right insula (BA 13), and the cerebellum bilaterally (see Table S1). Additional foci were observed in the precentral gyrus bilaterally (BA 4, 6), the left superior temporal gyrus (BA 22), the left postcentral gyrus (BA 2, 4, 40), the right cingulate gyrus (BA 31), the left insula (BA 13), and the thalamus bilaterally.
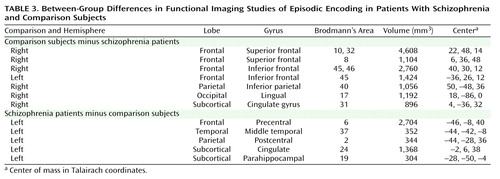
Comparison subjects > schizophrenia patients
Seven studies tested for greater activation in comparison subjects versus schizophrenia patients, resulting in 40 foci ( Table 3 ). As seen in Figure 1 , comparison subjects showed greater activation than patients in five brain regions. The largest differences were noted in the right superior frontal gyrus (BA 8, 10, 32) and the left and right inferior frontal gyri (BA 45, 46), followed by right hemisphere differences in the inferior parietal gyrus (BA 40), the lingual gyrus (BA 17), and the posterior cingulate gyrus (BA 31).
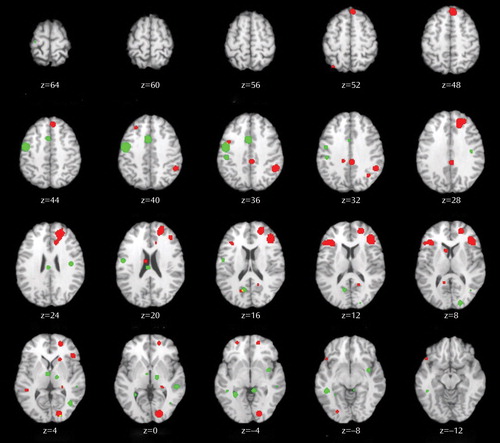
a Included studies are indicated in Table 1. Activation foci for contrasts of healthy comparison subjects > patients (red) and for regions where patients with schizophrenia > comparison subjects (green). Transaxial slices are spaced 4 mm apart and are presented according to neurological convention (right=right).
Four studies (five experiments and 30 foci) were of incidental tasks providing deep versus shallow encoding strategies. These were examined separately, given prior evidence (27 , 61) that ventrolateral prefrontal cortex (BA 44, 45, 47) activity may be restored when patients are provided with encoding strategies. Given the exploratory nature of this analysis, ALE was limited to comparison subject minus patient group contrasts (see Table S2 in the online supplement). As in the full ALE, patients had reduced activity in the right superior frontal gyrus (BA 8, 10, 32), the right dorsolateral prefrontal cortex (BA 46), the right inferior parietal gyrus (BA 40), the right lingual gyrus (BA 17), and the right cingulate gyrus (BA 31). However, there was no longer a group difference in the left ventrolateral prefrontal cortex ( Figure 2 ).
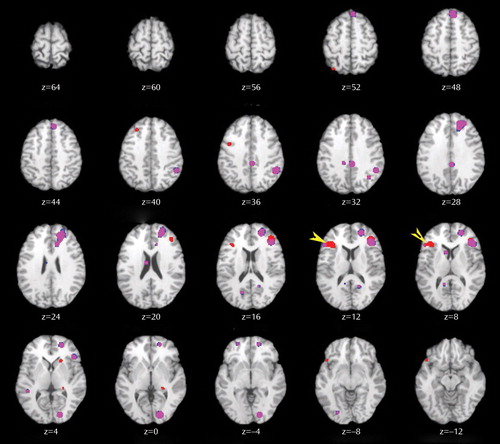
a The figure shows results for all selected encoding studies as illustrated in Figure 1 (red) and for a subset of incidental encoding studies in which patients were provided with encoding strategies (blue). Areas of overlap are indicated in purple, and the area of the dorsolateral prefrontal cortex where groups continued to differ when patients were provided with encoding strategies is indicated by yellow arrows. Slices formatted as in Figure 1.
Finally, the full ALE analysis was also repeated after excluding one study (57) because it did not control for group performance differences. When the comparison minus schizophrenia contrast was repeated with the remaining six studies (34 foci), the results were unchanged from those of the full sample (see Table S3 in the online supplement).
Schizophrenia patients > comparison subjects
Four studies performed this reverse contrast to identify significantly greater patient than comparison subject activation, resulting in 20 foci ( Table 3 ). This produced five distinct areas of greater patient activation ( Figure 1 ), including the left precentral gyrus (BA 6), the left middle temporal gyrus (BA 37), the left postcentral gyrus (BA 2, 43), the left cingulate gyrus (BA 24), and the left parahippocampal gyrus (BA 19). All studies included in this contrast accounted for group performance differences.
Episodic Retrieval
Healthy comparison subjects
Nine studies reported retrieval results for healthy subjects, resulting in 108 foci. Table S4 in the online supplement lists the 11 distinct brain regions activated. These included the left and right frontal gyri (BA 6, 9, 46), the right middle (BA 46) and medial frontal gyri (BA 6), the left superior frontal gyrus (BA 6), the left inferior temporal gyrus (BA 20), the left and right superior parietal gyri (BA 7), the left precuneus (BA 7, 31), the left supramarginal gyrus (BA 40), the left and right middle occipital gyri (BA 18), the right insula (BA 13), and the thalamus bilaterally.
Schizophrenia patients
Retrieval results were reported for patients in 11 studies, for a total of 111 foci (see Table S4 in the online supplement). Similar to healthy comparison subjects, patients activated the left inferior (BA 6, 9), right medial (BA 6, 11), and right middle (BA 9, 10) frontal gyri, the right superior parietal gyrus (BA 7), the left and right middle occipital gyri (BA 18), and the right thalamus. Patients showed additional areas of activation in the left middle frontal gyrus (BA 6, 46), the left middle temporal gyrus (BA 21), the left fusiform gyrus (BA 37), the left inferior parietal gyrus (BA 40), the left superior occipital gyrus (BA 19), and the cerebellum bilaterally.
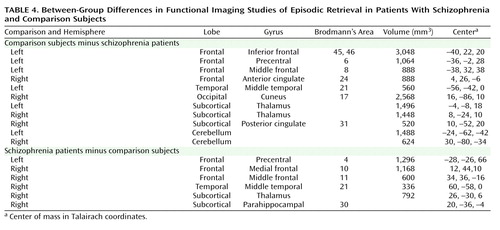
Comparison subjects > schizophrenia patients
Ten studies contrasted activity groups during retrieval, resulting in 76 foci ( Table 4 ). As seen in Figure 3 , the most extensive differences were in the left inferior frontal gyrus (BA 45, 46), followed by differences in the left precentral (BA 6) and middle frontal gyri (BA 8), the right anterior cingulate gyrus (BA 24), the left middle temporal gyrus (BA 21), the right cuneus (BA 17), the thalamus bilaterally, the right posterior cingulate gyrus (BA 31), and the cerebellum bilaterally.
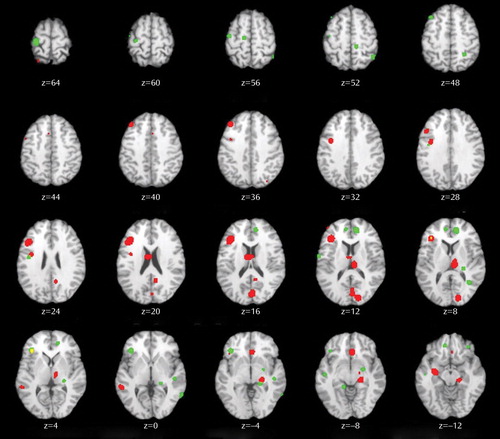
a Included studies are indicated in Table 1. Activation foci for contrasts of healthy comparison subjects > patients (red) and for regions where activation in patients with schizophrenia > comparison subjects (green). Slices formatted as in Figure 1.
Only seven studies (63 foci) controlled for group performance differences. When the ALE was limited to these studies, schizophrenia patients continued to have reduced activity in left inferior (BA 13, 46) and middle frontal gyri (BA 8), the right anterior cingulate gyrus (BA 24), the thalamus bilaterally, the right cuneus, and the cerebellum bilaterally (see Table S5 in the online supplement). However, previously observed group differences in the left precentral gyrus (BA 6), the left middle temporal gyrus (BA 21), and the right posterior cingulate gyrus (BA 31) were no longer present.
Schizophrenia patients > comparison subjects
This inverse contrast was examined in six studies, resulting in 26 foci demonstrating greater patient than comparison subject activation during episodic retrieval ( Table 4 ). As illustrated in Figure 3 , patients had greater activation in the left precentral gyrus (BA 4), followed by right hemisphere differences in the medial frontal gyrus (BA 10), the middle frontal gyrus (BA 11), the middle temporal gyrus (BA 21), the right thalamus, and the right parahippocampal gyrus (BA 30). When ALE was limited to the four studies (21 foci) that controlled for performance differences (see Table S5 in the online supplement), patients continued to show greater activity than comparison subjects in the left precentral gyrus (BA 4), the right medial frontal gyrus (BA 11), the right thalamus, and the right parahippocampal gyrus. There were no longer group differences in the right medial frontal (BA 10) and the medial temporal (BA 21) gyrus.
Discussion
This quantitative meta-analysis of episodic memory functional imaging studies, with a combined sample of 123 patients with schizophrenia and 137 healthy comparison subjects, found prominent deficits in the prefrontal cortex in patients. During encoding, these deficits were in the left frontopolar (BA 10, 32), ventrolateral (BA 45), and dorsolateral (BA 46) prefrontal cortex. During retrieval, the largest effects were also in the left ventrolateral and dorsolateral prefrontal cortex. When patients were provided with semantic encoding strategies, dorsolateral prefrontal cortex deficits remained, but activation of the ventrolateral prefrontal cortex was no longer reduced. This ventrolateral prefrontal cortex sparing is consistent with previous univariate (27 , 61 , 67 – 70) and meta-analytic studies (71) , which suggests that the ventrolateral prefrontal cortex may compensate for reduced dorsolateral prefrontal cortex function during working memory and episodic encoding (21 , 72 , 73) . In contrast, there was no evidence of reduced hippocampal or surrounding medial temporal lobe activation in patients versus comparison subjects during encoding or retrieval. The only group difference in the medial temporal lobe was a relative increase in activation in patients in the parahippocampal gyrus during encoding and retrieval. This prominent prefrontal dysfunction was not secondary to unequal performance, as prefrontal cortex deficits remained when studies that did not control for group performance differences were eliminated.
Patient dysfunction during encoding was relatively circumscribed, including portions of the prefrontal cortex and a default mode network (74) previously associated with increased task-related deactivation in schizophrenia across a wide array of behavioral paradigms (75 , 76) . Frontal lobe dysfunction was localized to the frontopolar, ventrolateral, and dorsolateral prefrontal cortex. These three regions are associated with discrete working memory and episodic encoding functions. The frontopolar prefrontal cortex provides for selection and processing of subgoals during working memory (77 , 78) ; the ventrolateral prefrontal cortex is involved with semantic processing and working memory maintenance (79) and binding of items with their context during working memory and episodic encoding (80) ; and the dorsolateral prefrontal cortex is involved with active working memory maintenance and manipulation (67 , 81) and with processing relationships between items during encoding (82 , 83) . These functional deficits suggest that patients have difficulty selecting and maintaining rules to process items in their context and in relation to each other to facilitate encoding. If rules are provided, schizophrenia patients appear capable of ventrolateral prefrontal cortex-mediated item-specific processing but remain unable to recruit the dorsolateral prefrontal cortex to establish more interactive relational memory representations, leading to severe deficits in relational memory (21) .
Patient deficits were more distributed during retrieval, even after group performance differences were eliminated. Impairments were noted in a frontocortical-cerebellar-thalamic network previously described by Andreasen and colleagues (33 , 37) as creating a condition of “cognitive dysmetria” in which patients have trouble coordinating sensorimotor and mental processes. However, cognitive dysmetria was formulated to extend beyond episodic retrieval, and our finding that these distributed regions were not impaired during encoding suggests that cognitive dysmetria cannot uniquely explain the pattern of our findings. On the other hand, evidence is accumulating that many components of this distributed network mediate specific cognitive functions that are important for successful episodic retrieval. The dorsolateral prefrontal cortex is associated with postretrieval monitoring (84 , 85) , the anterior cingulate gyrus with error or conflict detection (86) , the thalamus with attention and working memory (87) , and the cerebellum with working memory and mental flexibility (88) . These combined functional deficits suggest a scenario in which schizophrenia patients have difficulty monitoring their response output and detecting errors in order to flexibly adjust signal-detection thresholds to optimize sensitivity to targets while avoiding nontargets.
The aforementioned regions serve functions beyond episodic memory and are impaired in schizophrenia during other cognitive and emotional paradigms. The dorsolateral prefrontal cortex is broadly implicated in cognitive control mechanisms that allow information processing and behavior to vary adaptively from moment to moment, depending on current goals (89) . Our ALE findings may reflect a more general deficit in control mechanisms such as context maintenance (90) . Likewise, the thalamus is a central relay station that gates and filters sensory input to the cortex (91) , and thalamic dysfunction may reflect a fundamental deficit in sensory integration. Because ALE combines disparate studies, our analysis is not sufficiently constrained to establish functional specificity of these memory deficits. Establishing this level of specificity would require a focused effort, such as the Cognitive Neuroscience Treatment Research to Improve Cognition in Schizophrenia (CNTRICS) initiative (92) , to translate cognitive neuroscience tasks that are designed to parse these complex and overlapping functions to the study of schizophrenia.
The only group difference in the medial temporal lobe was increased activation in the parahippocampal gyrus in patients during encoding and retrieval. Overactivation in this and other regions (sensorimotor, middle cingulate gyrus, and middle temporal gyrus) in patients may reflect inefficient, compensatory brain activity as extraneous task-related activation can also be seen at early stages of learning before an optimal cognitive strategy has been reached (93) , and during reorganization following acute brain injury (94) . The parahippocampal gyrus is also associated with familiarity-based episodic retrieval (9) , and excess activity in this region may reflect patients’ overreliance on familiarity-based retrieval because of a specific recollection deficit (95) . Unlike the previous ALE study (22) , we did not find reduced hippocampal activation in schizophrenia, which may have resulted from our exclusion of region-of-interest studies to preserve the validity of the ALE method. The absence of hippocampal findings on the whole-brain level may have reflected increased susceptibility of small regions to smoothing artifact, although there were still no differences when the smoothing kernel was reduced to 6 mm and the ALEs repeated (data available on request). The absence of hippocampal findings may also reflect minimal relational binding demands (96 , 97) , as most included studies employed overlearned word stimuli. As more studies are performed that contrast relational versus item-specific encoding and retrieval, it will be interesting to see if medial temporal lobe differences can be detected on a meta-analytic level.
Several caveats must be considered when interpreting the results of this meta-analysis. First, in light of the limited number of articles meeting the study criteria, it was necessary to combine studies with disparate encoding and retrieval conditions and varying stimulus characteristics. This has the advantage of revealing the most robust and replicable task effects and group differences across memory paradigms, but the disadvantage of limiting our ability to ascribe specific brain regions to discrete memory processes. With a larger group of studies to choose from, it would be informative to segregate ALE analyses based on encoding condition (e.g., item-specific versus relational), stimulus modality (e.g., verbal, nonverbal), and retrieval task (e.g., recall versus recognition, cued versus uncued, item-specific versus relational). Second, the ALE method does not account for differences in sample size across included studies. This can be a strength in that it reveals the central tendency of the data, but a limitation if a study with a small sample and large effects that may not replicate is included and unduly influences overall results. Fortunately, the majority of studies had relatively equal sample sizes. Finally, all but two studies examined patients while they were receiving antipsychotic medication, which raises the question of drug effects. However, a qualitative examination of the two studies of unmedicated patients, both retrieval studies (33 , 37) , revealed the same pattern of reduced patient activation in prefrontal, cingulate, thalamic, and cerebellar regions that was seen in the studies of medicated patients. This apparent lack of medication effects is consistent with several studies of unmedicated patients (54 , 69) that documented reduced prefrontal activation in patients that was not restored by antipsychotic treatment (98) .
In sum, the results of this study provide strong support for the conclusion that episodic memory impairments in schizophrenia during encoding and retrieval are related to a reduction in memory control mechanisms implemented by the anterior, ventrolateral, and dorsolateral prefrontal cortex. These results suggest that behavioral interventions developed for remediating memory deficits in patients with frontal lobe damage (99) may also be applicable to schizophrenia. Use of pharmaco-fMRI (100 , 101) to identify compounds that improve prefrontal function (102) may also lead to new medications that improve memory and daily functioning in individuals with schizophrenia.
1. Aleman A, Hijman R, de Haan EHF, Kahn RS: Memory impairment in schizophrenia: a meta-analysis. Am J Psychiatry 1999; 156:1358–1366Google Scholar
2. Seidman LJ, Stone WS, Jones R, Harrison RH, Mirsky AF: Comparative effects of schizophrenia and temporal lobe epilepsy on memory. J Int Neuropsychol Soc 1998; 4:342–352Google Scholar
3. Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, Gur RC: Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 1994; 51:124–131Google Scholar
4. Cannon TD, Zorrilla LE, Shtasel D, Gur RE, Gur RC, Marco EJ, Moberg P, Price RA: Neuropsychological functioning in siblings discordant for schizophrenia and healthy volunteers. Arch Gen Psychiatry 1994; 51:651–661Google Scholar
5. Glahn DC, Almasy L, Blangero J, Burk GM, Estrada J, Peralta JM, Meyenberg N, Castro MP, Barrett J, Nicolini H, Raventos H, Escamilla MA: Adjudicating neurocognitive endophenotypes for schizophrenia. Am J Med Genet B Neuropsychiatr Genet 2007; 144B(2):242–249Google Scholar
6. Goldberg TE, Goldman RS, Burdick KE, Malhotra AK, Lencz T, Patel RC, Woerner MG, Schooler NR, Kane JM, Robinson DG: Cognitive improvement after treatment with second-generation antipsychotic medications in first-episode schizophrenia: is it a practice effect? Arch Gen Psychiatry 2007; 64:1115–1122Google Scholar
7. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996; 153:321–330Google Scholar
8. Scoville WB, Milner B: Loss of recent memory after bilateral hippocampal lesions. J Neurol Neurosurg Psychiatry 1957; 20:11–21Google Scholar
9. Eichenbaum H, Yonelinas AP, Ranganath C: The medial temporal lobe and recognition memory. Annu Rev Neurosci 2007; 30:123–152Google Scholar
10. Heckers S: Neuroimaging studies of the hippocampus in schizophrenia. Hippocampus 2001; 11:520–528Google Scholar
11. Benes FM, Berretta S: GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder. Neuropsychopharmacology 2001; 25:1–27Google Scholar
12. Gold JM, Randolph C, Carpenter CJ, Goldberg TE, Weinberger DR: Forms of memory failure in schizophrenia. J Abnorm Psychol 1992; 101:487–494Google Scholar
13. Paulsen JS, Heaton RK, Sadek JR, Perry W, Delis DC, Braff D, Kuck J, Zisook S, Jeste DV: The nature of learning and memory impairments in schizophrenia. J Int Neuropsychol Soc 1995; 1:88–99Google Scholar
14. Ranganath C, Knight RT: Prefrontal cortex-related functional neuroimaging, in The Cognitive Neuroscience of Memory Encoding and Retrieval. Edited by Parker A, Wilding EL, Bussey TJ. Philadelphia, Psychology Press, 2003, pp 83–99Google Scholar
15. Iddon JL, McKenna PJ, Sahakian BJ, Robbins TW: Impaired generation and use of strategy in schizophrenia: evidence from visuospatial and verbal tasks. Psychol Med 1998; 28:1049–1062Google Scholar
16. Brebion G, Amador X, Smith MJ, Gorman JM: Mechanisms underlying memory impairment in schizophrenia. Psychol Med 1997; 27:383–393Google Scholar
17. Ragland JD, Moelter ST, McGrath C, Hill SK, Gur RE, Bilker WB, Siegel SJ, Gur RC: Levels-of-processing effect on word recognition in schizophrenia. Biol Psychiatry 2003; 54:1154–1161Google Scholar
18. Baare WF, Hulshoff Pol HE, Hijman R, Mali WP, Viergever MA, Kahn RS: Volumetric analysis of frontal lobe regions in schizophrenia: relation to cognitive function and symptomatology. Biol Psychiatry 1999; 45:1597–1605Google Scholar
19. Coyle JT, Tsai G: NMDA receptor function, neuroplasticity, and the pathophysiology of schizophrenia. Int Rev Neurobiol 2004; 59:491–515Google Scholar
20. Goldman-Rakic PS, Selemon LD: Functional and anatomical aspects of prefrontal pathology in schizophrenia. Schizophr Bull 1997; 23:437–458Google Scholar
21. Ranganath C, Minzenberg MJ, Ragland JD: The cognitive neuroscience of memory function and dysfunction in schizophrenia. Biol Psychiatry 2008; 64:18–25Google Scholar
22. Achim AM, Lepage M: Episodic memory-related activation in schizophrenia: meta-analysis. Br J Psychiatry 2005; 187:500–509Google Scholar
23. Weiss AP, Heckers S: Neuroimaging of declarative memory in schizophrenia. Scand J Psychol 2001; 42:239–250Google Scholar
24. Turkeltaub P, Eden G, Jones K, Zeffiro T: Meta-analysis of the functional neuroanatomy of single-word reading: method and validation. Neuroimage 2002; 16:765–780Google Scholar
25. Laird AR, Fox PM, Price CJ, Glahn DC, Uecker AM, Lancaster JL, Turkeltaub PE, Kochunov P, Fox PT: ALE meta-analysis: controlling the false discovery rate and performing statistical contrasts. Hum Brain Mapp 2005; 25:155–164Google Scholar
26. Achim AM, Bertrand MC, Sutton H, Montoya A, Czechowska Y, Malla AK, Joober R, Pruessner JC, Lepage M: Selective abnormal modulation of hippocampal activity during memory formation in first-episode psychosis. Arch Gen Psychiatry 2007; 64:999–1014Google Scholar
27. Bonner-Jackson A, Haut K, Csernansky JG, Barch DM: The influence of encoding strategy on episodic memory and cortical activity in schizophrenia. Biol Psychiatry 2005; 58:47–55Google Scholar
28. Hazlett EA, Buchsbaum MS, Jeu LA, Nenadic I, Fleischman MB, Shihabuddin L, Haznedar MM, Harvey PD: Hypofrontality in unmedicated schizophrenia patients studied with PET during performance of a serial verbal learning task. Schizophr Res 2000; 43:33–46Google Scholar
29. Kubicki M, McCarley RW, Nestor PG, Huh T, Kikinis R, Shenton ME, Wible CG: An fMRI study of semantic processing in men with schizophrenia. Neuroimage 2003; 20:1923–1933Google Scholar
30. Leube DT, Rapp A, Buchkremer G, Bartels M, Kircher TT, Erb M, Grodd W: Hippocampal dysfunction during episodic memory encoding in patients with schizophrenia: an fMRI study. Schizophr Res 2003; 64:83–85Google Scholar
31. Nohara S, Suzuki M, Kurachi M, Yamashita I, Matsui M, Seto H, Saitoh O: Neural correlates of memory organization deficits in schizophrenia: a single photon emission computed tomography study with 99mTc-ethyl-cysteinate dimer during a verbal learning task. Schizophr Res 2000; 42:209–222Google Scholar
32. Zorilla LT, Jeste DV, Brown GG: Functional MRI and novel picture-learning among older patients with chronic schizophrenia: abnormal correlations between recognition memory and medial temporal brain response. Am J Geriatr Psychiatry 2002; 10:52–61Google Scholar
33. Andreasen NC, O’Leary DS, Cizadlo T, Arndt S, Rezai K, Ponto LL, Watkins GL, Hichwa RD: Schizophrenia and cognitive dysmetria: a positron-emission tomography study of dysfunctional prefrontal-thalamic-cerebellar circuitry. Proc Natl Acad Sci USA 1996; 93:9985–9990Google Scholar
34. Assaf M, Calhoun VD, Kuzu CH, Kraut MA, Rivkin PR, Hart J Jr, Pearlson GD: Neural correlates of the object-recall process in semantic memory. Psychiatry Res 2006; 147:115–126Google Scholar
35. Assaf M, Rivkin PR, Kuzu CH, Calhoun VD, Kraut MA, Groth KM, Yassa MA, Hart J Jr, Pearlson GD: Abnormal object recall and anterior cingulate overactivation correlate with formal thought disorder in schizophrenia. Biol Psychiatry 2006; 59:452–459Google Scholar
36. Cairo TA, Woodward TS, Ngan ET: Decreased encoding efficiency in schizophrenia. Biol Psychiatry 2006; 59:740–746Google Scholar
37. Crespo-Facorro B, Paradiso S, Andreasen NC, O’Leary DS, Watkins GL, Boles Ponto LL, Hichwa RD: Recalling word lists reveals “cognitive dysmetria” in schizophrenia: a positron emission tomography study. Am J Psychiatry 1999; 156:386–392Google Scholar
38. Crespo-Facorro B, Wiser AK, Andreasen NC, O’Leary DS, Watkins GL, Boles Ponto LL, Hichwa RD: Neural basis of novel and well-learned recognition memory in schizophrenia: a positron emission tomography study. Hum Brain Mapp 2001; 12:219–231Google Scholar
39. Fletcher P: The missing link: a failure of fronto-hippocampal integration in schizophrenia. Nat Neurosci 1998; 1:266–267Google Scholar
40. Ganguli R, Carter C, Mintun M, Brar J, Becker J, Sarma R, Nichols T, Bennington E: PET brain mapping study of auditory verbal supraspan memory versus visual fixation in schizophrenia. Biol Psychiatry 1997; 41:33–42Google Scholar
41. Heckers S, Rauch SL, Goff D, Savage CR, Schacter DL, Fischman AJ, Alpert NM: Impaired recruitment of the hippocampus during conscious recollection in schizophrenia. Nat Neurosci 1998; 1:318–323Google Scholar
42. Heckers S, Goff D, Schacter DL, Savage CR, Fischman AJ, Alpert NM, Rauch SL: Functional imaging of memory retrieval in deficit vs nondeficit schizophrenia. Arch Gen Psychiatry 1999; 56:1117–1123Google Scholar
43. Heckers S, Curran T, Goff D, Rauch SL, Fischman AJ, Alpert NM, Schacter DL: Abnormalities in the thalamus and prefrontal cortex during episodic object recognition in schizophrenia. Biol Psychiatry 2000; 48:651–657Google Scholar
44. Heinze S, Sartory G, Muller BW, de Greiff A, Forsting M, Juptner M: Neural activation during successful and unsuccessful verbal learning in schizophrenia. Schizophr Res 2006; 83:121–130Google Scholar
45. Jessen F, Scheef L, Germeshausen L, Tawo Y, Kockler M, Kuhn K-U, Maier W, Schild HH, Heun R: Reduced hippocampal activation during encoding and recognition of words in schizophrenia patients. Am J Psychiatry 2003; 160:1305–1312Google Scholar
46. Lahti AC, Holcomb HH, Medoff DR, Weiler MA, Tamminga CA, Carpenter WT Jr: Abnormal patterns of regional cerebral blood flow in schizophrenia with primary negative symptoms during an effortful auditory recognition task. Am J Psychiatry 2001; 158:1797–1808Google Scholar
47. Ongür D, Cullen TJ, Wolf DH, Rohan M, Barreira P, Zalesak M, Heckers S: The neural basis of relational memory deficits in schizophrenia. Arch Gen Psychiatry 2006; 63:356–365Google Scholar
48. Ragland JD, Gur RC, Glahn DC, Censits DM, Smith RJ, Lazarev MG, Alavi A, Gur RE: Frontotemporal cerebral blood flow change during executive and declarative memory tasks in schizophrenia: a positron emission tomography study. Neuropsychology 1998; 12:399–413Google Scholar
49. Ragland JD, McCarthy E, Bilker WB, Brensinger CM, Valdez J, Kohler C, Gur RE, Gur RC: Levels-of-processing effect on internal source monitoring in schizophrenia. Psychol Med 2006; 36:641–648Google Scholar
50. Weiss AP, Schacter DL, Goff DC, Rauch SL, Alpert NM, Fischman AJ, Heckers S: Impaired hippocampal recruitment during normal modulation of memory performance in schizophrenia. Biol Psychiatry 2003; 53:48–55Google Scholar
51. Weiss AP, Zalesak M, DeWitt I, Goff D, Kunkel L, Heckers S: Impaired hippocampal function during the detection of novel words in schizophrenia. Biol Psychiatry 2004; 55:668–675Google Scholar
52. Weiss AP, Goff D, Schacter DL, Ditman T, Freudenreich O, Henderson D, Heckers S: Fronto-hippocampal function during temporal context monitoring in schizophrenia. Biol Psychiatry 2006; 60:1268–1277Google Scholar
53. Wiser AK, Andreasen NC, O’Leary DS, Watkins GL, Boles Ponto LL, Hichwa RD: Dysfunctional cortico-cerebellar circuits cause “cognitive dysmetria” in schizophrenia. Neuroreport 1998; 9:1895–1899Google Scholar
54. Barch DM, Csernansky JG, Conturo T, Snyder AZ: Working and long-term memory deficits in schizophrenia: is there a common prefrontal mechanism? J Abnorm Psychol 2002; 111:478–494Google Scholar
55. Fahim C, Stip E, Mancini-Marie A, Beauregard M: Genes and memory: the neuroanatomical correlates of emotional memory in monozygotic twin discordant for schizophrenia. Brain Cogn 2004; 55:250–253Google Scholar
56. Hofer A, Weiss EM, Golaszewski SM, Siedentopf CM, Brinkhoff C, Kremser C, Felber S, Fleischhacker WW: An FMRI study of episodic encoding and recognition of words in patients with schizophrenia in remission. Am J Psychiatry 2003; 160:911–918Google Scholar
57. Hofer A, Weiss EM, Golaszewski SM, Siedentopf CM, Brinkhoff C, Kremser C, Felber S, Fleischhacker WW: Neural correlates of episodic encoding and recognition of words in unmedicated patients during an acute episode of schizophrenia: a functional MRI study. Am J Psychiatry 2003; 160:1802–1808Google Scholar
58. Lepage M, Montoya A, Pelletier M, Achim AM, Menear M, Lal S: Associative memory encoding and recognition in schizophrenia: an event-related fMRI study. Biol Psychiatry 2006; 60:1215–1223Google Scholar
59. Ragland JD, Gur RC, Raz J, Schroeder L, Kohler CG, Smith RJ, Alavi A, Gur RE: Effect of schizophrenia on frontotemporal activity during word encoding and recognition: a PET cerebral blood flow study. Am J Psychiatry 2001; 158:1114–1125Google Scholar
60. Ragland JD, Gur RC, Valdez J, Turetsky BI, Elliott M, Kohler C, Siegel S, Kanes S, Gur RE: Event-related fMRI of frontotemporal activity during word encoding and recognition in schizophrenia. Am J Psychiatry 2004; 161:1004–1015Google Scholar
61. Ragland JD, Gur RC, Valdez JN, Loughead J, Elliott M, Kohler C, Kanes S, Siegel SJ, Moelter ST, Gur RE: Levels-of-processing effect on frontotemporal function in schizophrenia during word encoding and recognition. Am J Psychiatry 2005; 162:1840–1848Google Scholar
62. Lancaster JL, Tordesillas-Gutierrez D, Martinez M, Salinas F, Evans A, Zilles K, Mazziotta JC, Fox PT: Bias between MNI and Talairach coordinates analyzed using the ICBM-152 brain template. Hum Brain Mapp 2007; 28:1194–1205Google Scholar
63. Brett M, Leff AP, Rorden C, Ashburner J: Spatial normalization of brain images with focal lesions using cost function masking. Neuroimage 2001; 14:486–500Google Scholar
64. Fox PT, Lancaster JL: Opinion: mapping context and content: the BrainMap model. Nat Rev Neurosci 2002; 3:319–321Google Scholar
65. Laird AR, McMillan KM, Lancaster JL, Kochunov P, Turkeltaub PE, Pardo JV, Fox PT: A comparison of label-based review and ALE meta-analysis in the Stroop task. Hum Brain Mapp 2005; 25:6–21Google Scholar
66. Laird AR, Lancaster JL, Fox PT: BrainMap: the social evolution of a human brain mapping database. Neuroinformatics 2005; 3:65–78Google Scholar
67. Barch DM, Carter CS, Braver TS, Sabb FW, MacDonald A 3rd, Noll DC, Cohen JD: Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Arch Gen Psychiatry 2001; 58:280–288Google Scholar
68. Callicott JH, Mattay VS, Verchinski BA, Marenco S, Egan MF, Weinberger DR: Complexity of prefrontal cortical dysfunction in schizophrenia: more than up or down. Am J Psychiatry 2003; 160:2209–2215Google Scholar
69. MacDonald AW III, Carter CS, Kerns JG, Ursu S, Barch DM, Holmes AJ, Stenger VA, Cohen JD: Specificity of prefrontal dysfunction and context processing deficits to schizophrenia in never-medicated patients with first-episode psychosis. Am J Psychiatry 2005; 162:475–484Google Scholar
70. Tan H-Y, Sust S, Buckholtz JW, Mattay VS, Meyer-Lindenberg A, Egan MF, Weinberger DR, Callicott JH: Dysfunctional prefrontal regional specialization and compensation in schizophrenia. Am J Psychiatry 2006; 163:1969–1977Google Scholar
71. Glahn DC, Ragland JD, Abramoff A, Barrett J, Laird AR, Bearden CE, Velligan DI: Beyond hypofrontality: a quantitative meta-analysis of functional neuroimaging studies of working memory in schizophrenia. Hum Brain Mapp 2005; 25:60–69Google Scholar
72. Tan HY, Callicott JH, Weinberger DR: Dysfunctional and compensatory prefrontal cortical systems, genes, and the pathogenesis of schizophrenia. Cereb Cortex 2007; 17(suppl 1):i171–i181Google Scholar
73. Wolf DH, Gur RC, Valdez JN, Loughead J, Elliott MA, Gur RE, Ragland JD: Alterations of fronto-temporal connectivity during word encoding in schizophrenia. Psychiatr Res 2007; 154:221–232Google Scholar
74. Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL: A default mode of brain function. Proc Natl Acad Sci USA 2001; 98:676–682Google Scholar
75. Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJ: Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev 2009; 33:279–296Google Scholar
76. Garrity AG, Pearlson GD, McKiernan K, Lloyd D, Kiehl KA, Calhoun VD: Aberrant “default mode” functional connectivity in schizophrenia. Am J Psychiatry 2007; 164:450–457Google Scholar
77. Braver TS, Bongiolatti SR: The role of frontopolar cortex in subgoal processing during working memory. Neuroimage 2002; 15:523–536Google Scholar
78. Fletcher PC, Henson RN: Frontal lobes and human memory: insights from functional neuroimaging. Brain 2001; 124:849–881Google Scholar
79. Kan IP, Thompson-Schill SL: Selection from perceptual and conceptual representations. Cogn Affect Behav Neurosci 2004; 4:466–482Google Scholar
80. Blumenfeld RS, Ranganath C: Prefrontal cortex and long-term memory encoding: an integrative review of findings from neuropsychology and neuroimaging. Neuroscientist 2007; 13:280–291Google Scholar
81. Barch DM, Braver TS, Nystrom LE, Forman SD, Noll DC, Cohen JD: Dissociating working memory from task difficulty in human prefrontal cortex. Neuropsychologia 1997; 35:1373–1380Google Scholar
82. Blumenfeld RS, Ranganath C: Dorsolateral prefrontal cortex promotes long-term memory formation through its role in working memory organization. J Neurosci 2006; 26:916–925Google Scholar
83. Murray LJ, Ranganath C: The dorsolateral prefrontal cortex contributes to successful relational memory encoding. J Neurosci 2007; 27:5515–5522Google Scholar
84. Achim AM, Lepage M: Neural correlates of memory for items and for associations: an event-related functional magnetic resonance imaging study. J Cogn Neurosci 2005; 17:652–667Google Scholar
85. Rugg MD, Henson RN, Robb WG: Neural correlates of retrieval processing in the prefrontal cortex during recognition and exclusion tasks. Neuropsychologia 2003; 41:40–52Google Scholar
86. Carter CS, van Veen V: Anterior cingulate cortex and conflict detection: an update of theory and data. Cogn Affect Behav Neurosci 2007; 7:367–379Google Scholar
87. Andrews J, Wang L, Csernansky JG, Gado MH, Barch DM: Abnormalities of thalamic activation and cognition in schizophrenia. Am J Psychiatry 2006; 163:463–469Google Scholar
88. Segarra N, Bernardo M, Valdes M, Caldu X, Falcon C, Rami L, Bargallo N, Parramon G, Junque C: Cerebellar deficits in schizophrenia are associated with executive dysfunction. Neuroreport 2008; 19:1513–1517Google Scholar
89. Shallice T: From Neuropsychology to Mental Structure. Cambridge, UK, Cambridge University Press, 1988Google Scholar
90. Cohen JD, Servan-Schreiber D: Context, cortex, and dopamine: a connectionist approach to behavior and biology in schizophrenia. Psychol Rev 1992; 99:45–77Google Scholar
91. Jones EG: The Thalamus. New York, Plenum Press, 1985Google Scholar
92. Carter CS, Barch DM: Cognitive neuroscience-based approaches to measuring and improving treatment effects on cognition in schizophrenia: the CNTRICS initiative. Schizophr Bull 2007; 33:1131–1137Google Scholar
93. Ramsey NF, Jansma JM, Jager G, Van Raalten T, Kahn RS: Neurophysiological factors in human information processing capacity. Brain 2004; 127:517–525Google Scholar
94. Johansen-Berg H: Structural plasticity: rewiring the brain. Curr Biol 2007; 17(4):R141–R144Google Scholar
95. Achim AM, Lepage M: Is associative recognition more impaired than item recognition memory in schizophrenia? a meta-analysis. Brain Cogn 2003; 53:121–124Google Scholar
96. Eldridge LL, Knowlton BJ, Furmanski CS, Bookheimer SY, Engel SA: Remembering episodes: a selective role for the hippocampus during retrieval. Nat Neurosci 2000; 3:1149–1152Google Scholar
97. Hannula DE, Tranel D, Cohen NJ: The long and the short of it: relational memory impairments in amnesia, even at short lags. J Neurosci 2006; 26:8352–8359Google Scholar
98. Snitz BE, MacDonald A III, Cohen JD, Cho RY, Becker T, Carter CS: Lateral and medial hypofrontality in first-episode schizophrenia: functional activity in a medication-naive state and effects of short-term atypical antipsychotic treatment. Am J Psychiatry 2005; 162:2322–2329Google Scholar
99. Davidson PS, Troyer AK, Moscovitch M: Frontal lobe contributions to recognition and recall: linking basic research with clinical evaluation and remediation. J Int Neuropsychol Soc 2006; 12(2):210–223Google Scholar
100. Stein EA: fMRI: a new tool for the in vivo localization of drug actions in the brain. J Anal Toxicol 2001; 29:419–424Google Scholar
101. Honey G, Bullmore E: Human pharmacological MRI. Trends Pharmacol Sci 2004; 25:366–374Google Scholar
102. Gray JA, Roth BL: Molecular targets for treating cognitive dysfunction in schizophrenia. Schizophr Bull 2007; 33:1100–1119Google Scholar