In this Issue
Olanzapine for Anorexia Nervosa
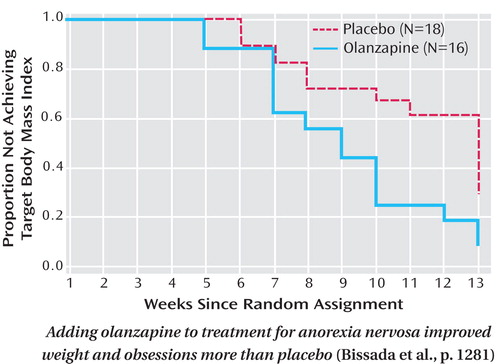
The weight gain associated with the antipsychotic olanzapine is a possible benefit for patients with anorexia nervosa. Bissada et al. (CME, p. Original article: 1281 ) compared olanzapine with placebo as an additional treatment for 34 women in an intensive day hospital program for anorexia nervosa. Over 10 weeks, those randomly assigned to olanzapine gained more weight and gained weight faster ; the target body mass index was reached by 88% of the olanzapine group and 56% of the placebo group. Both groups had declines in obsessions, compulsions, depression, and anxiety, but those taking olanzapine had significantly larger decreases in obsessive thoughts. Dr. Katherine Halmi discusses perplexities in randomized, placebo-controlled treatment trials for anorexia nervosa in an editorial on p. Original article: 1227 .
Compulsive Hoarding: Separate Syndrome?
People who hoard compulsively but do not have other symptoms of obsessive-compulsive disorder (OCD) differ in several respects from hoarders with OCD. Pertusa et al. (CME, p. Original article: 1289 ) found that those without OCD reported less hoarding-related checking and obsessions, cited intrinsic or sentimental value as motivation, and were older when their clutter was deemed excessive. Those with hoarding plus OCD scored higher on clinician ratings of severity and functional impairment. They were also more likely to hoard letters, receipts, old medication, and bizarre items, such as rotten food. On the other hand, both hoarding groups had more family history of OCD and hoarding than people with other anxiety disorders or community comparison groups. In an editorial on p. Original article: 1229 , Drs. James Leckman and Michael Bloch examine hoarding as part of their developmental and evolutionary perspective on OCD.
Adding Aripiprazole to Mood Stabilizers
Patients with bipolar disorder who responded only partially to either valproate or lithium achieved a 63% response rate after aripiprazole was added for 6 weeks, whereas adding placebo resulted in a 49% response rate. Vieta et al. (p. Original article: 1316 ) report that the difference in symptom reduction between adjunctive aripiprazole and placebo was evident after 1 week. The advantages for aripiprazole included a lower proportion of patients with emergent depression and more improvement in psychosocial functioning. Among the patients who completed the 6-week study, both the valproate and lithium subgroups had greater improvements with adjunctive aripiprazole than placebo. Patients taking lithium plus aripiprazole had a 28% rate of akathisia, versus 12% for those taking valproate plus aripiprazole and 4%–6% for patients taking adjunctive placebo. An editorial by Drs. Joseph Calabrese and David Kemp on p. Original article: 1234 relates clinical trials for bipolar disorder to treatment in the real world.
Diagnosing PTSD in Children
Diagnoses of posttraumatic stress disorder (PTSD) for very young children involved in motor vehicle accidents were more reliable when based on modified symptom criteria than on established DSM-IV criteria. For older children, however, a DSM-IV diagnosis of acute stress disorder in the month following the accident was better than the alternative criteria for predicting PTSD at 6 months. For the children ages 2 to 6 years, all diagnoses were based on parental reports of symptoms. For the children ages 7–10, Meiser-Stedman et al. (p. Original article: 1326 ) compared the findings based on reports by the child only, by the parents only, and by both. Diagnoses based on combined parent-child reports at 2–4 weeks were better predictors of 6-month diagnoses than those based on a single source. Dr. Michael Sheeringa highlights the study’s contributions in an editorial on p. Original article: 1237 .



