A Case of fMRI-Guided rTMS Treatment of Coenesthetic Hallucinations
To the Editor: Hallucinations are the major first-rank symptoms in schizophrenia spectrum disorders and are commonly defined as a perceptual experience in the absence of sensory imput. However, these symptoms are rarely described outside of the auditory modality. We report the case of a patient with a positive diagnosis of schizoaffective disorder (according to DSM-IV-TR criteria).
“Mr. L” was a 33-year-old man who had been treated surgically 5 years previously for a testicular carcinoma. His regular clinical, biological, and imaging follow-up examinations did not show any signs of malignant extension. He developed coenesthetic hallucinations, experienced as electric shocks and alien objects moving inside his thorax, abdomen, and pelvis, for which treatment with antipsychotic and mood-stabilizing medications was unsuccessful. Through the use of new data-driven analyses (1) , we observed a bilateral neural activity in the somatosensory and superior parietal cortices during coenesthetic hallucinations on a functional magnetic resonance imaging (fMRI) scan ( Figure 1 ). Since repetitive transcranial magnetic stimulation (rTMS) has previously been used to treat auditory verbal hallucinations in adults (2) and children (3) with schizophrenia, Mr. L benefited from 10 daily sessions of fMRI-guided 1-Hz rTMS over the somatosensory cortex. A total of 10 4 pulses were delivered at 100% of the patient’s motor threshold using the Magstim super-rapid stimulator, with a figure-of-eight coil positioned tangentially to the brain target. Low frequency rTMS has been shown to be effective in reducing neural excitability (2) . The patient’s rTMS sessions were successful in reducing the frequency and intensity of his coenesthetic hallucinations, measured using the Visual Analogical Scale (score: –55%; frequency: 73% to 18%; intensity: 84% to 30%). This improvement remained stable for at least 8 weeks and allowed a significant improvement in the patient’s quality of life (improvement for Short Form-36–Physical Health subscores: from 35.5 to 65.1; improvement for Short Form-36–Mental Health subscores: from 21.8 to 53).
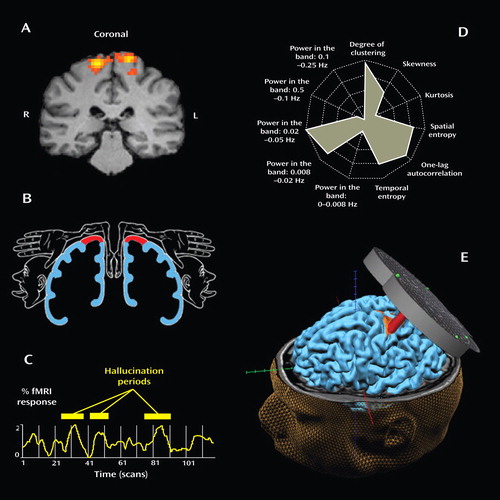
a Three coenesthetic hallucinatory episodes are shown, using the BrainVoyager QX 1.7 software package for fMRI data (panel A). This hyperactivation perfectly overlapped with the thoraco-abdominal zone of Penfield’s somatosensory homunculus (panel B) and corresponded to the anatomical site of the patient’s somatic symptoms. The time course of the fMRI signal (panel C) and the Independent-Component Fingerprint method (5) (panel D) confirmed the neurophysiological origin of these activations. The fMRI-guided repetitive rTMS targeted over the patient’s somatosensory cortex dramatically reduced his hallucinations (panel E); t=6.8; p<10 –4 .
Our case demonstrates a link between the visceral symptoms of a patient’s hallucinations and cortical somatotopic organization. This functional anatomical link is consistent with the results recently reported in the visual modality for a hallucinating patient with schizophrenia in whom neural hyperactivation was measured in category selective visual areas (4). To our knowledge, this is the first case report demonstrating the efficacy of neuronavigated rTMS in the treatment of coenesthetic hallucinations in a patient with schizoaffective disorder.
1. van de Ven VG, Formisano E, Roder CH, Prvulovic D, Bittner RA, Dietz MG, Hubl D, Dierks T, Federspiel A, Esposito F, Di Salle F, Jansma B, Goebel R, Linden DE: The spatiotemporal pattern of auditory cortical responses during verbal hallucinations. Neuroimage 2005; 27:644–655Google Scholar
2. Aleman A, Sommer IE, Kahn RS: Efficacy of slow repetitive transcranial magnetic stimulation in the treatment of resistant auditory hallucinations in schizophrenia: a meta-analysis. J Clin Psychiatry 2007; 68:416–421Google Scholar
3. Jardri R, Lucas B, Delevoye-Turrell Y, Delmaire C, Delion P, Thomas P, Goeb JL: An 11-year-old boy with drug-resistant schizophrenia treated with temporo-parietal rTMS. Mol Psychiatry 2007; 12:320Google Scholar
4. Oertel V, Rotarska-Jagiela A, van de Ven VG, Haenschel C, Maurer K, Linden DE: Visual hallucinations in schizophrenia investigated with functional magnetic resonance imaging. Psychiatry Res 2007; 156:269–273Google Scholar
5. De Martino F, Gentile F, Esposito F, Balsi M, Di Salle F, Goebel R, Formisano E: Classification of fMRI independent components using IC-fingerprints and support vector machine classifiers. Neuroimage 2007; 34:177–194Google Scholar



