Drug Interactions and Pharmacogenomics in the Treatment of Breast Cancer and Depression
“Ms. B” is a 45-year-old married premenopausal woman who was diagnosed with major depressive disorder 10 years ago and then successfully treated for 12 months with fluoxetine (20 mg/day) without significant side effects. She remained free of depressive symptoms for the next 8–9 years. One year ago, she was diagnosed with estrogen receptor-positive invasive breast cancer and underwent treatment with surgery, followed by chemotherapy, and then radiation therapy. Ms. B. has been treated with tamoxifen (a selective estrogen receptor modulator) for the past 6 months to reduce the likelihood of breast cancer recurrence. She has tolerated tamoxifen relatively well, except for moderately bothersome hot flashes, for which she has received no pharmacotherapy. Recently, however, she developed recurrent depressive symptoms and sought treatment from her psychiatrist. What pharmacologic agents are effective against both depression and hot flashes in women with breast cancer? Would any of these agents compromise the efficacy of tamoxifen or increase its toxicity through a drug-drug interaction?
Depression in Breast Cancer
Many women experience distress following the diagnosis of breast cancer, and a subset of these women experience clinically significant depression (1) . The estimated point prevalence of major depressive disorder in all women is in the range of 3.5%–7% (2) . In comparison, the rate of depression in women with breast cancer is estimated to be in the range of 10%–25%, depending on the method of assessment (3) . Rates appear higher in the first year following diagnosis, especially in younger women and in women treated with chemotherapy (3) .
Studies evaluating the association between depression and treatment with tamoxifen have yielded mixed results. In some trials, a subset of patients have discontinued tamoxifen therapy because of depressive symptoms, whereas in other studies, conducted primarily in the breast cancer prevention setting, no increased risk of depression was observed during treatment with tamoxifen (4 , 5) .
Endocrine Therapy for Breast Cancer
Approximately 180,000 women are diagnosed with invasive breast cancer in the United States each year (6) . The majority of these patients will have tumors that express estrogen receptor and/or progesterone receptor on the cell surfaces. Women with hormone receptor-positive tumors obtain substantial benefit from treatment with tamoxifen or agents that decrease circulating levels of estrogen, such as aromatase inhibitors (7) . At present, the standard of care for treatment of premenopausal women with estrogen receptor-positive invasive breast cancer is tamoxifen therapy, whereas for postmenopausal women, both tamoxifen and aromatase inhibitors are acceptable treatment options. Analyses of thousands of women treated with 5 years of tamoxifen versus no endocrine therapy for invasive breast cancer demonstrate a 31% decrease in annual breast cancer death rate with tamoxifen (7) .
An additional 60,000 women are diagnosed with noninvasive breast cancer each year (6) , and many will be offered tamoxifen to reduce the risk of an in-breast recurrence or a new primary tumor. Moreover, well-validated population-based models have been developed to estimate an unaffected woman’s risk of developing breast cancer. Women at risk for breast cancer may be recommended for therapy with tamoxifen or raloxifene (8) . Several prospective randomized controlled trials have demonstrated that tamoxifen decreases the risk of a new primary breast cancer in high-risk women by 40%–50% (8) . Thus, a substantial number of women with an increased risk for breast cancer are treated annually with antiestrogen therapy.
Tamoxifen has both antiestrogenic and estrogenic activity, depending on the target organ. These differential effects lead to clinical benefit as well as to potentially bothersome side effects and rare but severe toxicity (9) . Tamoxifen is antiestrogenic in the breast, resulting in decreased breast cancer development and recurrence, as well as in the brain, leading to hot flashes. Conversely, tamoxifen is estrogenic in the bone, liver, and uterus, resulting in improvements in bone density and lipid profile, but also potentially increasing the risk of both thromboembolic disease and uterine cancer (8 , 9) . As noted above, it is unclear whether tamoxifen causes or exacerbates depression, but this agent was recently demonstrated to have antimanic properties in patients with bipolar disorder (10) .
Treatments for Concurrent Hot Flashes and Depression
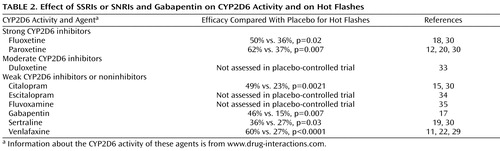
Antiestrogen therapy for patients with breast cancer, which may induce or exacerbate depression and anxiety and which frequently causes hot flashes, has led to an intersection between clinical oncology and clinical psychiatry. Prospective randomized clinical trials have demonstrated that selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) effectively decrease vasomotor symptoms in healthy menopausal women and women with breast cancer, on or off endocrine therapy (11 – 16) . In general, these studies have shown that most of these medications decrease hot flash frequency by about 60%, compared with a decrease of 25%–35% with placebo (11 , 12 , 16) . These observations have primarily been made with venlafaxine, paroxetine (continuous release formulation), and citalopram (11 , 12 , 15 , 16) . In addition to these antidepressants, the anticonvulsant gabapentin has been shown to decrease hot flashes to a similar degree (16 , 17) . Modest improvements in hot flashes have also been reported for other SSRIs and SNRIs, including fluoxetine and sertraline (18 , 19) .
Tamoxifen Metabolism
Tamoxifen itself is a relatively weak selective estrogen receptor modulator and is considered to be a classical prodrug—it is converted to metabolites that are notably more potent than the parent drug itself. It is primarily metabolized in the liver by the cytochrome P450 system to a number of active metabolites, including 4-hydroxytamoxifen (4-OH tamoxifen) and 4-hydroxy-N-desmethyltamoxifen, designated endoxifen (20) . Endoxifen and 4-OH tamoxifen are equipotent, and both are approximately 100 times more active as antiestrogens than the parent compound, tamoxifen (21) . However, endoxifen is present in concentrations 5–10 times higher than 4-OH tamoxifen in most women taking tamoxifen.
Tamoxifen is converted to endoxifen principally by a noninducible P450 enzyme that is coded for by the most polymorphic, and most studied, gene in the cytochrome P450 system: CYP2D6. More than 80 different major alleles of the CYP2D6 gene have been identified, many of which confer decreased or absent CYP2D6 activity, and patients can be divided into poor, intermediate, extensive, and ultrarapid metabolizers on the basis of their genotype. While 60% of individuals of European descent are homozygous for the active, most common allele (*1), approximately 7% are homozygous for an inactive, variant allele (*4). Other alleles, including *5, *10, and *41, also confer absent CYP2D6 activity. In one study, breast cancer patients treated with tamoxifen who were homozygous for a poor metabolizer genotype (*4/*4) had significantly lower serum concentrations of endoxifen than those with the active (*1/*1) genotype (22) .
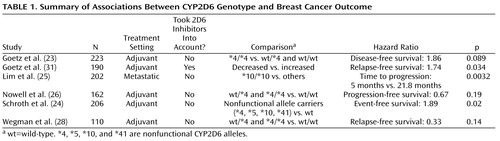
These results have led to retrospective studies evaluating the effect of CYP2D6 genotype on breast cancer outcomes. In one study, estrogen receptor-positive breast cancer patients homozygous for the poor metabolizer genotype who were treated with tamoxifen monotherapy were more likely to experience a recurrence of breast cancer than those patients who carried an allele coding for active enzyme (adjusted hazard ratio=1.86, p=0.089) (23) . These findings were consistent with the hypothesis that homozygous *4/*4 patients did not activate tamoxifen to endoxifen and therefore received less or no benefit from the drug. Results from subsequent studies have been mixed; some confirmed this finding (24 – 26) , while others did not ( Table 1 ) (27 , 28) . In fact, two of these studies suggested just the opposite effect: CYP2D6 *4/*4 patients actually had better outcomes with tamoxifen monotherapy (27 , 28) . Nevertheless, although further studies are required, these investigations suggest an important role for CYP2D6 activity in tamoxifen metabolism.
Coadministration of Tamoxifen and an SSRI or SNRI
In addition to genetic inactivation of CYP2D6, CYP2D6 activity can be decreased by medications that inhibit the enzyme (22 , 29 , 30) . Therefore, use of CYP2D6 inhibitors in patients who are being treated with tamoxifen, even if they have the homozygous active genotype, could potentially affect breast cancer outcomes, in a manner similar to the poor metabolizer genotype. Inhibition of tamoxifen conversion to endoxifen may decrease the efficacy of tamoxifen therapy and increase the risk of breast cancer development or recurrence. Several SSRIs and SNRIs are potent, moderate, or mild inhibitors of CYP2D6 ( Table 2 ).
Indeed, women with wild-type CYP2D6 genotype treated with tamoxifen have been shown to have statistically significant decreases in endoxifen concentration following initiation of concomitant paroxetine therapy (20) . An observational study of women treated with tamoxifen demonstrated low serum concentrations of endoxifen in those concomitantly treated with strong inhibitors of CYP2D6, such as paroxetine and fluoxetine, and intermediate levels of endoxifen in those concomitantly treated with weak inhibitors, such as sertraline and citalopram (29) . It is noteworthy that venlafaxine, which does not inhibit CYP2D6, had little effect on endoxifen concentration. Similarly, it would be expected that other SSRIs and SNRIs that have not been shown to inhibit CYP2D6 activity, such as fluvoxamine and escitalopram, would have little effect on endoxifen concentration, although this hypothesis has not yet been formally studied.
The influence of concomitant medications in addition to CYP2D6 genotype on breast cancer outcome has also been investigated in one of the retrospective patient cohorts mentioned earlier (31) . Information about concomitant treatment with CYP2D6 inhibitors was extracted from medical records and combined with genotype information to classify patients on the basis of metabolizer status. Those women with decreased CYP2D6 metabolism had increased rates of breast cancer recurrence and decreased relapse-free survival time. Since it was a retrospective analysis of a previously conducted study, endoxifen concentrations were not available. Nonetheless, the authors concluded that based on these data, CYP2D6 inhibitors should probably be avoided in patients being treated with tamoxifen.
Although these studies are small relative to major studies of breast cancer outcome, the data suggest that SSRIs and SNRIs with no or minimal effect on CYP2D6 activity, such as citalopram and venlafaxine, are unlikely to interfere with the formation of endoxifen. Similarly, the anticonvulsant gabapentin is not known to affect CYP2D6 activity or the formation of endoxifen. Other SSRIs that inhibit CYP2D6 may prevent endoxifen formation and adversely affect tamoxifen activity. However, since SSRIs and SNRIs have been demonstrated to decrease hot flashes in otherwise healthy postmenopausal women who are not taking tamoxifen, and since citalopram, venlafaxine, and gabapentin are as effective in reducing hot flashes as strong CYP2D6 inhibitors in women taking tamoxifen, the mechanism by which these antidepressants reduce hot flashes is likely not due to blockade of endoxifen production. Taken together, these data suggest that concomitant use of potent CYP2D6 inhibitors ( Table 2 ) should be avoided in women taking tamoxifen, unless the patient is committed to one of these drugs as an effective antidepressant where other medications have been ineffective, or a patient requiring antidepressant therapy cannot tolerate alternative agents. Antidepressant therapy with escitalopram or fluvoxamine could also be considered in patients being treated with tamoxifen, but the effect of these medications on hot flashes has not yet been assessed.
Summary and Recommendations
The retrospective data regarding CYP2D6 genotype and breast cancer outcomes in patients receiving treatment with tamoxifen were presented to the U.S. Food and Drug Administration (FDA) at an advisory committee meeting in October 2006. At that time, some members of the panel recommended routine CYP2D6 genotyping for patients being treated with tamoxifen. However, others were more conservative given the mixed results described above ( Table 1 ) and recommended that genotyping be considered as an option in these patients. At this time, the FDA has not recommended changing the package insert for tamoxifen to describe metabolism by CYP2D6 or to recommend CYP2D6 genotyping of patients prior to initiation of therapy, and genotyping for CYP2D6 is not routinely performed in the clinical management of breast cancer patients. Further studies of the impact of CYP2D6 genotype on breast cancer outcomes are under way, so additional information should be available in the near future to help guide treatment decision making for individual patients (32) .
At present, however, since the data suggest that CYP2D6 activity may adversely affect tamoxifen metabolism, which in turn may influence breast cancer outcomes, it is reasonable to avoid known CYP2D6 inhibitors in women taking tamoxifen, assuming that alternative treatment options (such as citalopram, gabapentin, and venlafaxine) will be tolerable. Some women are stable on therapy with an SSRI or SNRI that inhibits CYP2D6 or are unable to tolerate the medications that do not inhibit CYP2D6. In these situations, the patient’s psychiatrist should discuss therapy options with the treating oncologist, since there may be alternative endocrine therapy options available for management of the patient’s breast cancer. For example, ovarian suppression can be used for treatment of premenopausal women, and aromatase inhibitor therapy can be an excellent option for postmenopausal women.
In the vignette, Ms. B was interested in taking a single medication that could treat both her depressive symptoms and her hot flashes, and she had heard that some antidepressants were able to manage both. Because she had previously tolerated fluoxetine well, she requested this medication. Her psychiatrist had heard about the possible drug-drug interactions between tamoxifen and some SSRIs, however, and therefore encouraged Ms. B to consider trying a different antidepressant to avoid any potential decrease in tamoxifen efficacy. The psychiatrist initiated therapy with extended-release venlafaxine, and Ms. B is currently taking 75 mg daily. Ms. B has tolerated this antidepressant well, her depressive symptoms have improved, and her hot flashes are now mild and infrequent.
1. Payne DK, Hoffman RG, Theodoulou M, Dosik M, Massie MJ: Screening for anxiety and depression in women with breast cancer: psychiatry and medical oncology gear up for managed care. Psychosomatics 1999; 40:64–69Google Scholar
2. Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH: A 40-year perspective on the prevalence of depression: the Stirling County study. Arch Gen Psychiatry 2000; 57:209–215Google Scholar
3. Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J: Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 2008; 30:112–126Google Scholar
4. Thompson DS, Spanier CA, Vogel VG: The relationship between tamoxifen, estrogen, and depressive symptoms. Breast J 1999; 5:375–382Google Scholar
5. Day R, Ganz PA, Costantino JP: Tamoxifen and depression: more evidence from the National Surgical Adjuvant Breast and Bowel Project’s Breast Cancer Prevention (P-1) Randomized Study. J Natl Cancer Inst 2001; 93:1615–1623Google Scholar
6. American Cancer Society: Breast Cancer Facts and Figures, 2007–2008. http://www.cancer.org/downloads/STT/BCFF-Final.pdfGoogle Scholar
7. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG): Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; 365:1687–1717Google Scholar
8. Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, Bevers TB, Kavanah MT, Atkins JN, Margolese RG, Runowicz CD, James JM, Ford LG, Wolmark N: Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 2005; 97:1652–1662Google Scholar
9. Osborne CK: Tamoxifen in the treatment of breast cancer. N Engl J Med 1998; 339:1609–1618Google Scholar
10. Yildiz A, Guleryuz S, Ankerst DP, Ongur D, Renshaw PF: Protein kinase C inhibition in the treatment of mania: a double-blind, placebo-controlled trial of tamoxifen. Arch Gen Psychiatry 2008; 65:255–263Google Scholar
11. Loprinzi CL, Kugler JW, Sloan JA, Mailliard JA, LaVasseur BI, Barton DL, Novotny PJ, Dakhil SR, Rodger K, Rummans TA, Christensen BJ: Venlafaxine in management of hot flashes in survivors of breast cancer: a randomised controlled trial. Lancet 2000; 356:2059–2063Google Scholar
12. Stearns V, Beebe KL, Iyengar M, Dube E: Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. JAMA 2003; 289:2827–2834Google Scholar
13. Nelson HD, Vesco KK, Haney E, Fu R, Nedrow A, Miller J, Nicolaidis C, Walker M, Humphrey L: Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA 2006; 295:2057–2071Google Scholar
14. Stearns V: Clinical update: new treatments for hot flushes. Lancet 2007; 369:2062–2064Google Scholar
15. Barton DL, LaVasseur B, Sloan JA, Stella PJ, Flynn K, Dyar M, Dakhil SR, Atherton PJ, Diekmann B, Loprinzi CL: A phase III trial evaluating three doses of citalopram for hot flashes: NCCTG trial N05C9. J Clin Oncol 2008; 26:9538aGoogle Scholar
16. Loprinzi CL, Sloan JA, Stearns V, Diekmann B, Novotny PJ, Kimmick G, Gordon P, Pandya KJ, Guttuso T, Reddy S: Newer antidepressants and gabapentin for hot flashes: an individual subject pooled analysis. J Clin Oncol 2008; 26:9537aGoogle Scholar
17. Pandya KJ, Morrow GR, Roscoe JA, Zhao H, Hickok JT, Pajon E, Sweeney TJ, Banerjee TK, Flynn PJ: Gabapentin for hot flashes in 420 women with breast cancer: a randomised double-blind placebo-controlled trial. Lancet 2005; 366:818–824Google Scholar
18. Loprinzi CL, Sloan JA, Perez EA, Quella SK, Stella PJ, Mailliard JA, Halyard MY, Pruthi S, Novotny PJ, Rummans TA: Phase III evaluation of fluoxetine for treatment of hot flashes. J Clin Oncol 2002; 20:1578–1583Google Scholar
19. Kimmick GG, Lovato J, McQuellon R, Robinson E, Muss HB: Randomized, double-blind, placebo-controlled, crossover study of sertraline (Zoloft) for the treatment of hot flashes in women with early stage breast cancer taking tamoxifen. Breast J 2006; 12:114–122Google Scholar
20. Stearns V, Johnson MD, Rae JM, Morocho A, Novielli A, Bhargava P, Hayes DF, Desta Z, Flockhart DA: Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst 2003; 95:1758–1764Google Scholar
21. Johnson MD, Zuo H, Lee KH, Trebley JP, Rae JM, Weatherman RV, Desta Z, Flockhart DA, Skaar TC: Pharmacological characterization of 4-hydroxy-N-desmethyl tamoxifen, a novel active metabolite of tamoxifen. Breast Cancer Res Treat 2004; 85:151–159Google Scholar
22. Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH, Skaar T, Storniolo AM, Li L, Araba A, Blanchard R, Nguyen A, Ullmer L, Hayden J, Lemler S, Weinshilboum RM, Rae JM, Hayes DF, Flockhart DA: CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 2005; 97:30–39Google Scholar
23. Goetz MP, Rae JM, Suman VJ, Safgren SL, Ames MM, Visscher DW, Reynolds C, Couch FJ, Lingle WL, Flockhart DA, Desta Z, Perez EA, Ingle JN: Pharmacogenetics of tamoxifen biotransformation is associated with clinical outcomes of efficacy and hot flashes. J Clin Oncol 2005; 23:9312–9318Google Scholar
24. Schroth W, Antoniadou L, Fritz P, Schwab M, Muerdter T, Zanger UM, Simon W, Eichelbaum M, Brauch H: Breast cancer treatment outcome with adjuvant tamoxifen relative to patient CYP2D6 and CYP2C19 genotypes. J Clin Oncol 2007; 25:5187–5193Google Scholar
25. Lim HS, Ju Lee H, Seok Lee K, Sook Lee E, Jang IJ, Ro J: Clinical implications of CYP2D6 genotypes predictive of tamoxifen pharmacokinetics in metastatic breast cancer. J Clin Oncol 2007; 25:3837–3845Google Scholar
26. Nowell S, Ahn J, Rae JM, Scheys JO, Trovato A, Sweeney C, MacLeod SL, Kadlubar FF, Ambrosone CB: Association of genetic variation in tamoxifen-metabolizing enzymes with overall survival and recurrence of disease in breast cancer patients. Breast Cancer Res Treat 2005; 91:249–258Google Scholar
27. Wegman P, Vainikka L, Stal O, Nordenskjold B, Skoog L, Rutqvist LE, Wingren S: Genotype of metabolic enzymes and the benefit of tamoxifen in postmenopausal breast cancer patients. Breast Cancer Res 2005; 7:R284–R290Google Scholar
28. Wegman P, Elingarami S, Carstensen J, Stal O, Nordenskjold B, Wingren S: Genetic variants of CYP3A5, CYP2D6, SULT1A1, UGT2B15 and tamoxifen response in postmenopausal patients with breast cancer. Breast Cancer Res 2007; 9:R7Google Scholar
29. Borges S, Desta Z, Li L, Skaar TC, Ward BA, Nguyen A, Jin Y, Storniolo AM, Nikoloff DM, Wu L, Hillman G, Hayes DF, Stearns V, Flockhart DA: Quantitative effect of CYP2D6 genotype and inhibitors on tamoxifen metabolism: implication for optimization of breast cancer treatment. Clin Pharmacol Ther 2006; 80:61–74Google Scholar
30. Hemeryck A, Belpaire FM: Selective serotonin reuptake inhibitors and cytochrome P-450 mediated drug-drug interactions: an update. Curr Drug Metab 2002; 3:13–37Google Scholar
31. Goetz MP, Knox SK, Suman VJ, Rae JM, Safgren SL, Ames MM, Visscher DW, Reynolds C, Couch FJ, Lingle WL, Weinshilboum RM, Fritcher EG, Nibbe AM, Desta Z, Nguyen A, Flockhart DA, Perez EA, Ingle JN: The impact of cytochrome P450 2D6 metabolism in women receiving adjuvant tamoxifen. Breast Cancer Res Treat 2007; 101:113–121Google Scholar
32. Hayes DF, Stearns V, Rae J, Flockhart DA: A model citizen? is tamoxifen more effective than aromatase inhibitors if we pick the right patients? J Natl Cancer Inst 2008; 100:610–613Google Scholar
33. Skinner MH, Kuan HY, Pan A, Sathirakul K, Knadler MP, Gonzales CR, Yeo KP, Reddy S, Lim M, Ayan-Oshodi M, Wise SD: Duloxetine is both an inhibitor and a substrate of cytochrome P4502D6 in healthy volunteers. Clin Pharmacol Ther 2003; 73:170–177Google Scholar
34. Preskorn SH, Greenblatt DJ, Flockhart D, Luo Y, Perloff ES, Harmatz JS, Baker B, Klick-Davis A, Desta Z, Burt T: Comparison of duloxetine, escitalopram, and sertraline effects on cytochrome P450 2D6 function in healthy volunteers. J Clin Psychopharmacol 2007; 27:28–34Google Scholar
35. Gerstenberg G, Aoshima T, Fukasawa T, Yoshida K, Takahashi H, Higuchi H, Murata Y, Shimoyama R, Ohkubo T, Shimizu T, Otani K: Effects of the CYP 2D6 genotype and cigarette smoking on the steady-state plasma concentrations of fluvoxamine and its major metabolite fluvoxamino acid in Japanese depressed patients. Ther Drug Monit 2003; 25:463–468Google Scholar