Factors Associated With Remission From Alcohol Dependence in an American Indian Community Group
Abstract
Objective: This study identified factors associated with remission from DSM-III-R alcohol dependence in an American Indian community group. Method: Participants were assessed by using the Semi-Structured Assessment for the Genetics of Alcoholism. Results: Five hundred eighty participants were assessed for alcohol use and alcohol use symptoms; 254 participants were found to have alcohol dependence. The rate of remission in this group was 59%. Thirty-four percent of remitters and 39% of nonremitters had received treatment for alcohol problems. Remission from alcohol dependence was associated with being female, older, and married; an earlier age of onset of alcohol dependence; and self-reported depression symptoms from drinking. Absence of remission was associated with continuing to drink despite knowing one had medical problems from drinking and self-reported anxiety symptoms from drinking. Conclusions: Attention to factors associated with remission from alcohol dependence may be important in designing more effective treatment and prevention programs in this high-risk population.
Native Americans, as a group, have the highest alcohol-related death rates of any U.S. ethnic group (1) , and rates of alcohol dependence in the small number of tribes studied have been reported as 20%–70% (2 – 6) , higher than the epidemiological rate of DSM-IV (7) alcohol dependence of 13% in the U.S. general population (8) . Although research has delineated factors posing increased risk for the development of alcohol dependence in Native Americans (9 – 13) , little is known about factors associated with remission from alcohol dependence in this high-risk group.
In the U.S. general population, the rate of remission from alcohol dependence is substantial. Dawson and colleagues (14) , using data from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions, found that 75% of adults with prior to past year DSM-IV alcohol dependence were currently in remission. Forty-eight percent were in complete remission, showing no symptoms of alcohol dependence for the preceding year. Thirty-six percent were in recovery, defined as showing no signs of alcohol dependence and either abstinence or drinking at levels below those considered to constitute risk drinking in the preceding year. These rates of remission are similar to those found in other epidemiologic studies of remission and recovery from alcohol dependence in the United States (15) , Canada (16) , and Germany (17) .
Over the past two decades, a large body of research has focused on identifying factors associated with remission from alcohol dependence. Despite using different variables of interest, diagnostic criteria, diagnostic instruments, and interview and sampling techniques, generally consistent themes have emerged from these studies. Female gender, older age at assessment, current marriage, more robust social support, younger age at onset of alcohol dependence, less quantity of drinking, and less severity of drinking all tend to be associated with remission (14 , 18 , 19) . In contrast to studies of treatment samples, which have generally shown less sustained remission in individuals with comorbid anxiety and affective disorders (20 – 22) , epidemiologic samples have not shown an association of those disorders with absence of remission (14 , 17) . Much of the literature on remission from alcohol dependence has focused on the role of treatment in remission; however, data from the National Epidemiologic Survey on Alcohol and Related Conditions (14) have demonstrated that abstinent and nonabstinent recovery from alcohol dependence are similar in individuals who have received treatment and those who have not.
The available evidence suggests that rates of remission from alcohol dependence are also substantial in Native American communities (3 – 5 , 23) . Ehlers and colleagues (3) , in a study of the first 243 American Indian adults who participated in the present study, found a remission rate of 61% from DSM-III-R alcohol dependence. Factors associated with remission were not examined in that study. This report is an effort to identify factors associated with remission in this American Indian group.
Method
Participants
American Indian participants were recruited from eight geographically contiguous reservations with a total population of about 3,000 individuals. Participants were recruited using a combination of a venue-based method for sampling hard-to-reach populations (24 , 25) and a respondent-driven procedure (26) that has been described elsewhere (10) . To be included in the study, the participants had to be of at least 1/16th Native American Heritage, be between the ages of 18 and 70 years, and be mobile enough to be transported from their homes to the General Clinical Research Center of the Scripps Research Institute. The protocol for the study was approved by the Institutional Review Board of the Scripps Research Institute, the Scientific Advisory Committee of the General Clinical Research Center, and the Indian Health Council, a tribal review group overseeing health issues for the reservations where recruitment was undertaken. Written informed consent was obtained from each participant after the study was fully explained.
Measures
Each participant completed an interview with the Semi-Structured Assessment for the Genetics of Alcoholism (27) , which gathers demographic, onset, and recency information on alcohol use, drug use, and psychiatric disorder symptoms. This measure is a fully structured, polydiagnostic psychiatric interview that generates DSM-III-R diagnoses and has undergone both reliability and validity testing (27 , 28) . The Semi-Structured Assessment for the Genetics of Alcoholism interviews were administered by trained research assistants, and all the best final diagnoses were made by a research psychiatrist/addiction specialist (D.A.G.).
In this study, a lifetime diagnosis of alcohol dependence was made if a participant met three or more dependence criteria for DSM-III-R (29) alcohol dependence, with the added condition that three or more criteria had to occur or “cluster” during the same month or longer in the participant’s life. One-month clustering exceeds the DSM-IV (7) criterion of 1-year clustering. Remission was defined as having no symptom of alcohol dependence for 6 months or longer at the time of the interview (6 months of full remission).
Other DSM-III-R diagnostic criteria were defined as follows. Having any lifetime DSM-III-R anxiety disorder was defined as having any one or more of the following disorders: panic, agoraphobia without panic, social phobia, and obsessive-compulsive disorders. Having any lifetime affective disorder was defined as having any one or more of the following disorders: major depressive, bipolar I, bipolar II, and dysthymic disorders. Two types of anxiety and affective disorders were considered: those independent of substance use and those considered to be substance induced. To be considered substance induced, the anxiety or affective disorder had to occur in the context of persistent and heavy use of one or more substances, either as an intoxication or withdrawal syndrome. Criteria for diagnosing substance-induced disorders were derived from Schuckit and colleagues (30) , Hesselbrock and colleagues (31) , and DSM-IV-TR (32) . These criteria have been reported elsewhere (10 , 33) .
Childhood conduct disorder was defined as having three or more criteria for conduct disorder before the age of 15 without meeting criteria for adult antisocial personality disorder. The Semi-Structured Assessment for the Genetics of Alcoholism does not make the DSM-IV requirements of nicotine dependence but is able to generate information that allows for the lifetime ascertainment of persistent smoking, defined as smoking 10 or more cigarettes per day over 1 year or more during a participant’s lifetime.
In addition to collecting information sufficient to make DSM-III-R disorder diagnoses, the Semi-Structured Assessment for the Genetics of Alcoholism collects information on self-reported alcohol-induced symptoms. It also asks whether a participant felt anxious or depressed during alcohol withdrawal. In contrast to questions that gathered information to generate anxiety and affective disorder (independent and substance-induced) diagnoses by DSM-III-R criteria, these questions asked participants to report significant anxiety and depressive symptoms that the participants themselves identified (i.e., self-reported) as caused by alcohol intoxication or withdrawal.
Other information collected by the Semi-Structured Assessment for the Genetics of Alcoholism and other questionnaires included demographic information, the number of religious (both traditional American Indian and Euro-American origin) services attended in the past year, drinking history, and dependence symptoms. The number of standard drinks consumed per month during the period of heaviest drinking since the participant began to drink regularly was collected with a drinking history questionnaire that employs a timeline follow-back procedure and is administered with the Semi-Structured Assessment for the Genetics of Alcoholism. Legal endangering (to self or others) problems from drinking, alcohol use severity, and continued drinking despite medical problems were taken from Semi-Structured Assessment for the Genetics of Alcoholism questions used to establish dependence criteria. The number of lifetime alcohol-dependent criteria (three to nine) was also collected. Duration of dependence was considered the number of years between the age of onset of 1-month clustered alcohol dependence and the most recent age at which the participant had any symptom of alcohol dependence, even if the participant had not used alcohol for a portion of that period or had failed to meet full criteria for dependence at any time during those years.
Data Analysis
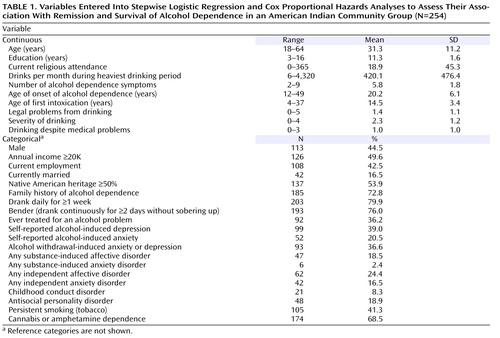
Demographic and clinical variables putatively associated with remission from and survival duration of alcohol dependence for the group as a whole are listed in Table 1 . Table 2 describes each variable in the remitter and nonremitter groups. Each variable was compared in the remitter versus the nonremitter group in univariate comparisons with the nonparametric Mann-Whitney U test for continuous variables and Fisher’s exact test for categorical variables.
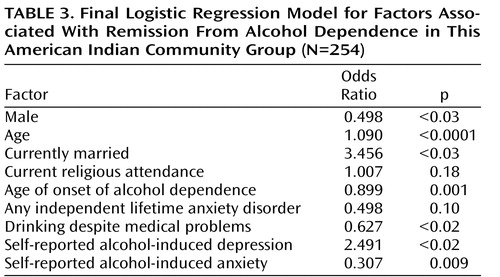
Subsequent data analyses focused on the two aims of the study. The first aim of the study was to determine the significance of variables putatively associated with remission. A multivariate logistic regression analysis was conducted for remission from alcohol dependence (yes or no) as the outcome variable with independent variables putatively related to remission, which included variables examined in the National Epidemiologic Survey on Alcohol and Related Conditions data set (14) . Logistic regression was carried out using the forward stepwise likelihood ratio approach of Hosmer and Lemeshow (34) . In this approach, p entry is 0.15 and p removal is 0.20. Significance was set at p<0.05 for variables in the final model, which is shown in Table 3 .
The second aim of the study was to examine the factors affecting the survival of alcohol dependence in this group. Cox proportional hazards regression was used to determine the impact of the same variables on survival of alcohol dependence from age of onset of alcohol dependence to age of recency in the presence of censored cases. In the Cox regression analysis, the p entry criterion of 0.15 and p removal criterion of 0.20 were used in a forward stepwise likelihood ratio approach. Significance was set at p<0.05 in the final model, which is shown in Table 4 .
Results
Five hundred eighty participants were assessed for alcohol use and alcohol use symptoms. Two hundred fifty-four participants met criteria for lifetime DSM-III-R alcohol dependence with the added condition that three or more symptom criteria of dependence had to cluster during the same month or more in the participant’s life and the 254 participants had complete data for all variables used in the logistic regression and Cox proportional hazards analyses. Of these, 150 (59%) participants had complete remission from alcohol dependence.
Demographic characteristics of the group as a whole resemble those of U.S. census data (35) . Descriptive statistics for all demographic and clinical variables used in the logistic and Cox regression analyses are shown in Table 1 . The results of univariate comparisons of each variable in the remitter versus nonremitter groups are shown in Table 2 .
Stepwise logistic regression analysis of factors putatively associated with remission resulted in the final model shown in Table 3 . Being older, female, and married; having an earlier age of onset of alcohol dependence; and having self-reported depression symptoms from drinking were significantly associated with remission. Continuing to drink despite medical problems and having self-reported anxiety symptoms from drinking were significantly associated with absence of remission. None of the other variables, including years of education, income, employment, first-degree family history of alcohol dependence, Native American Heritage, age of first intoxication, drinking daily for a week or more, having gone on benders of 2 days or more, quantity of drinking during the period of heaviest drinking, number of criteria of alcohol dependence, childhood conduct disorder, antisocial personality disorder, independent or substance-induced anxiety and affective disorders, cannabis or amphetamine dependence, persistent smoking (tobacco), having legal, endangering or alcohol use severity problems associated with drinking, and ever having had treatment for problems related to alcohol use, were associated with remission. The final model accounted for 30.2% of the variance in remission from alcohol dependence.
Evaluation of factors associated with survival time of alcohol dependence following diagnosis using stepwise Cox regression resulted in the final model shown in Table 4 . Being younger, being married, having an older age of onset of alcohol dependence were associated with a shorter duration of alcohol dependence. Continuing to drink (despite medical problems) and self-reported anxiety symptoms from drinking were associated with a longer duration of alcohol dependence. Other factors, including gender, independent and substance-induced anxiety and affective disorders, childhood conduct disorder, antisocial personality disorder, cannabis or amphetamine dependence, other problems related to alcohol use, and treatment for alcohol problems, were not associated with survival of alcohol dependence.
Discussion
In this study, the rate of 6-month full remission from DSM-III-R alcohol dependence with 1-month clustering of 59% is comparable to the U.S. epidemiological rate of 1 year prior to past year, full remission from DSM-IV alcohol dependence of 48% (14) , the 1-year partial remission rate of 64% in a German representative population sample (17) , and the 1-year full remission rate from alcohol abuse and dependence of 53% found in Ontario, Canada (16) . Despite the high rate of 1-month clustered DSM-III-R alcohol dependence of 49% in this group, the rate of full remission is comparable to studies of predominantly European ancestry populations.
Several factors associated with full remission in this American Indian group are consistent with factors associated with full remission in the general U.S. population. Our findings are consistent with the findings of Dawson and colleagues (14) that abstinent and nonabstinent recovery in the general U.S. population are associated with female gender, increasing age, and being married, but not with tobacco use, dependent use of illicit drugs, and having any lifetime anxiety or affective disorder. Our findings are also consistent with Schuckit and colleagues (30) , who found that episodes of 3-month abstinence in a mixed treatment and nontreatment group were associated with female gender, older age, ever having been married, and younger age of onset of alcohol dependence, but not with a primary diagnosis of antisocial personality disorder.
Increasing likelihood of remission with advancing age in this American Indian group is consistent with the “aging out” phenomenon described in the Navajo (5 , 23) . Why “aging out” occurs in American Indians and other ethnicities is unclear. Alcohol dependence may biologically run its course in a proportion of alcohol dependents, and/or the accumulating psychosocial burden of alcohol dependence may prompt increasingly successful attempts at cutting back on drinking. In addition, as age advances, individuals with alcohol dependence, as well as those without, may develop new work, social, and family networks (19) that play a role in reducing drinking. The consistent association of remission with marriage (14 , 18 , 36) suggests that the social support and limit setting that can come from a spouse are important factors in promoting remission.
This study is also noteworthy for the factors that were not associated with remission. Several demographic variables, including current employment, years of education, economic status, frequency of attendance at religious services, first-degree family history of alcohol dependence, and Native American Heritage were not significantly associated with remission. Treatment for alcohol problems was not associated with remission in the group, a finding that may suggest that alcohol-dependent individuals find nontreatment as well as treatment-related pathways out of dependence, and/or individuals with a more refractory illness are those most likely to seek treatment.
In contrast to Dawson and colleagues (14) , we did not find that either the amount of alcohol use (as measured by quantity and frequency during the period of heaviest use), the severity of dependence (as measured by total lifetime dependence symptoms), legal/endangering problems from drinking, or alcohol use severity was associated with remission. These findings suggest that, at least in this group, increasing quantity of alcohol use and severity of dependence does not militate against remission. We did find that continuing to drink despite medical problems was associated with absence of remission, perhaps because the groups of individuals who continue to drink over extended periods tend to develop medical problems.
Of particular note is our finding that comorbid disorders, including independent anxiety and affective, substance-induced anxiety and affective, childhood conduct, adult antisocial personality, and cannabis- or amphetamine-dependence disorders, were not associated with a greater or lesser likelihood of remission from alcohol dependence. In general, these findings are consistent with epidemiologic studies of the general U.S. (14) and north German (17) populations. In treatment populations, comorbid disorders have generally been associated with increased likelihood of relapse following treatment (20 – 22) . Although comorbid disorders are etiologically associated with alcohol dependence, the results of this study, taken together with those of Dawson and colleagues (14) and Bischof and colleagues (17) , suggest that comorbidity per se is not etiologically related to remission from alcohol dependence in both predominantly Euro-American and American Indian samples. This finding, as well as the findings that severity of use and dependence are not associated with remission status, may justify some optimism that comorbidity and severity of illness do not militate against remission, at least in nontreatment-seeking populations.
A surprising and novel finding of this study is that self-reported depression and anxiety symptoms do play a significant role in increasing and decreasing, respectively, the likelihood of remission. These are not depression and anxiety symptoms occurring in the context of alcohol withdrawal, because a similar question asking whether withdrawal had ever caused depression or anxiety symptoms did not appear in the final logistic regression model. Why self-reported depression and anxiety caused by drinking should be significantly associated with remission, especially in light of the absence of association of independent or substance-induced anxiety and affective disorders with remission, is unclear. It may be that insight about the nature of the relationship between drinking and depression and anxiety is a critical element in promoting or inhibiting remission. Why self-reported alcohol-induced depression would increase while self-reported alcohol induced anxiety would decrease the likelihood of remission is also unclear. The former is consistent with findings that insight promotes increased compliance with treatment and remission of other psychiatric disorders (37 – 39) . The latter is consistent with the hypothesis that individuals with alcohol dependence and alcohol-induced anxiety symptoms are more likely to continue drinking, perhaps as a means to self-medicate those symptoms. Both raise the possibility that education about the depression and anxious effects of alcohol and alternative ways of dealing with anxiety symptoms that accompany alcohol dependence may have an important role in treatment and community prevention programs in this high-risk population.
We also tested whether factors associated with remission of alcohol dependence were also associated with the survival of alcohol dependence. Two factors significantly associated with remission (being married and having self-reported depression symptoms from drinking) were also significantly associated with a shorter duration of alcohol dependence, and two factors associated with nonremission (continuing to drink despite medical problems and having self-reported anxiety symptoms from drinking) were also significantly associated with a longer duration of alcohol dependence. Advancing age and younger age at onset of alcohol dependence were both associated with increased likelihood of remission. However, both advancing age and younger age at onset of alcohol dependence were associated with increased duration of alcohol dependence. These data are consistent with previous findings in this group that alcohol dependence runs a typical clinical course that includes duration as well as symptom profile (3) . These data are not consistent with the notion that, from the standpoint of remission, there may be two groups of alcohol-dependent individuals: those with early onset who have a shorter course of alcoholism and those with later onset who have a longer course, which has been suggested for other populations (16 , 40) .
The results of this study should be interpreted in light of several limitations. First, our findings may not generalize to other American Indians or be representative of all American Indians. Second, we used cross-sectional and retrospective data. Cross-sectional data include individuals who will remit during their lifetimes but have not yet remitted, and so the odds ratios for factors associated with remission may be higher or lower than they would otherwise be. Retrospective data suffer from recall bias, which may include a reporting bias that results from having remitted or not remitted, advancing age, and other variables used in the logistic regression analysis. A prospective study of the development of alcohol dependence and its clinical course would provide a more powerful model for remission in this population. Third, comparisons to other populations of alcoholics may be limited by differences in sampling techniques as well as varying genetic and environmental variables in different populations. Fourth, in this study, we chose to examine 6-month full remission from DSM-III-R alcohol dependence with the added condition that three or more criteria of alcohol dependence had to “cluster,” that is, occur in the same month or longer in the participant’s life. In this group, 17.1% of the group had a lifetime diagnosis of DSM-III-R alcohol abuse. If we had chosen another definition of remission, had examined DSM-III-R alcohol dependence without 1-month clustering, or included alcohol dependence and alcohol abuse as a unitary alcohol use disorder diagnosis, we might have found that other variables were associated with remission from and survival of the alcohol use disorder. Fifth, we did not assess two important anxiety disorders, generalized anxiety disorder and posttraumatic stress disorder. If we had information on those diagnoses, our findings on the association of remission from and survival of alcohol dependence with anxiety disorders might have been different. Finally, a higher mortality rate among nonremitters than remitters may have skewed variables associated with nonremission, rendering them more or less associated with nonremission and survival of alcohol dependence than they would be if potential participants who had died before being interviewed could have been sampled. Despite these limitations, this report represents an important first step in identifying factors associated with remission from alcohol dependence in this high-risk group.
1. Shalala DE, Trujillo MH, Hartz PE, Paisano EL: Trends in Indian Health 1998–99. Washington, DC, United States Department Health and Human Services, Indian Health Service, Division of Program Statistics, 1999Google Scholar
2. Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM: Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry 2005; 162:1723–1732Google Scholar
3. Ehlers CL, Wall TL, Betancourt M, Gilder DA: The clinical course of alcoholism in 243 mission Indians. Am J Psychiatry 2004; 161:1204–1210Google Scholar
4. Leung PK, Kinzie JD, Boehnlein JK, Shore JH: A prospective study of the natural course of alcoholism in a Native American village. J Stud Alcohol 1993; 54:733–738Google Scholar
5. Kunitz SJ: Life-course observations of alcohol use among Navajo Indians: natural history or careers? Med Anthropol Q 2006; 20:279–296Google Scholar
6. Robin RW, Long JC, Rasmussen JK, Albaugh B, Goldman D: Relationship of binge drinking to alcohol dependence, other psychiatric disorders, and behavioral problems in an American Indian tribe. Alcohol Clin Exp Res 1998; 22:518–523Google Scholar
7. American Psychiatric Association, Task Force on DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Washington, DC, American Psychiatric Association, 1994Google Scholar
8. Hasin DS, Stinson FS, Ogburn E, Grant BF: Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2007; 64:830–842Google Scholar
9. Ehlers CL, Slutske WS, Gilder DA, Lau P, Wilhelmsen KC: Age at first intoxication and alcohol use disorders in southwest California Indians. Alcohol Clin Exp Res 2006; 30:1856–1865Google Scholar
10. Gilder DA, Wall TL, Ehlers CL: Comorbidity of select anxiety and affective disorders with alcohol dependence in southwest California Indians. Alcohol Clin Exp Res 2004; 28:1805–1813Google Scholar
11. Kunitz SJ, Gabriel KR, Levy JE, Henderson E, Lampert K, McCloskey J, Quintero G, Russell S, Vince A: Alcohol dependence and conduct disorder among Navajo Indians. J Stud Alcohol 1999; 60:159–167Google Scholar
12. Wall TL, Carr LG, Ehlers CL: Protective association of genetic variation in alcohol dehydrogenase with alcohol dependence in Native American mission Indians. Am J Psychiatry 2003; 160:41–46Google Scholar
13. Whitbeck LB, Chen X, Hoyt DR, Adams GW: Discrimination, historical loss and enculturation: culturally specific risk and resiliency factors for alcohol abuse among American Indians. J Stud Alcohol 2004; 65:409–418Google Scholar
14. Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ: Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction 2005; 100:281–292Google Scholar
15. Dawson DA, Archer LD, Grant BF: Reducing alcohol-use disorders via decreased consumption: a comparison of population and high-risk strategies. Drug Alcohol Depend 1996; 42:39–47Google Scholar
16. Cunningham JA, Lin E, Ross HE, Walsh GW: Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav 2000; 25:317–321Google Scholar
17. Bischof G, Rumpf HJ, Meyer C, Hapke U, John U: Influence of psychiatric comorbidity in alcohol-dependent subjects in a representative population survey on treatment utilization and natural recovery. Addiction 2005; 100:405–413Google Scholar
18. McAweeney MJ, Zucker RA, Fitzgerald HE, Puttler LI, Wong MM: Individual and partner predictors of recovery from alcohol-use disorder over a nine-year interval: findings from a community sample of alcoholic married men. J Stud Alcohol 2005; 66:220–228Google Scholar
19. Moos RH, Moos BS: Protective resources and long-term recovery from alcohol use disorders. Drug Alcohol Depend 2007; 86:46–54Google Scholar
20. Dodge R, Sindelar J, Sinha R: The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. J Subst Abuse Treat 2005; 28:189–196Google Scholar
21. Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J: Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry 2002; 59:375–380Google Scholar
22. Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE: Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry 1987; 44:505–513Google Scholar
23. Quintero G: “The lizard in the green bottle”: “aging out” of problem drinking among Navajo men. Soc Sci Med 2000; 51:1031–1045Google Scholar
24. Kalton G, Anderson DW: Sampling rare populations. J Royal Stat Society 1986; 149:65–82Google Scholar
25. Muhib FB, Lin LS, Stueve A, Miller RL, Ford WL, Johnson WD, Smith PJ: A venue-based method for sampling hard-to-reach populations. Public Health Rep 2001; 116(suppl 1):216–222Google Scholar
26. Heckathorn DD: Respondent-driven sampling: a new approach to the study of hidden populations. Soc Problems 1997; 44:174–199Google Scholar
27. Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI Jr, Reich T, Schmidt I, Schuckit MA: A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol 1994; 55:149–158Google Scholar
28. Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V: A validity study of the SSAGA—a comparison with the scan. Addiction 1999; 94:1361–1370Google Scholar
29. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R). Washington, DC, American Psychiatric Association, 1987Google Scholar
30. Schuckit MA, Tipp JE, Bucholz KK, Nurnberger JI Jr, Hesselbrock VM, Crowe RR, Kramer J: The life-time rates of three major mood disorders and four major anxiety disorders in alcoholics and controls. Addiction 1997; 92:1289–1304Google Scholar
31. Hesselbrock VM, Segal B, Hesselbrock MN: Alcohol dependence among Alaska natives entering alcoholism treatment: a gender comparison. J Stud Alcohol 2000; 61:150–156Google Scholar
32. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). Washington, DC, American Psychiatric Association, 2000Google Scholar
33. Gilder DA, Lau P, Dixon M, Corey L, Phillips E, Ehlers CL: Co-morbidity of select anxiety, affective, and psychotic disorders with cannabis dependence in southwest California Indians. J Addict Dis 2006; 25:67–79Google Scholar
34. Hosmer DW, Lemeshow S: Applied Logistic Regression, 2nd ed. New York, John Wiley & Sons, 2000Google Scholar
35. United States Bureau of the Census: Characteristics of American Indians by Tribe and Language. Washington, DC, United States Department of Commerce, Economics and Statistics Administration, 1990Google Scholar
36. Humphreys K, Moos RH, Cohen C: Social and community resources and long-term recovery from treated and untreated alcoholism. J Stud Alcohol 1997; 58:231–238Google Scholar
37. Caton CL, Hasin DS, Shrout PE, Drake RE, Dominguez B, Samet S, Schanzer B: Predictors of psychosis remission in psychotic disorders that co-occur with substance use. Schizophr Bull 2006; 32:618–625Google Scholar
38. Ko NY, Yeh ML, Hsu ST, Chung HH, Yen CF: Investigation of insight formation using narrative analyses of people with schizophrenia in remission. J Nerv Ment Dis 2006; 194:124–127Google Scholar
39. Smith TE, Hull JW, Huppert JD, Silverstein SM, Anthony DT, McClough JF: Insight and recovery from psychosis in chronic schizophrenia and schizoaffective disorder patients. J Psychiatr Res 2004; 38:169–176Google Scholar
40. Moss HB, Chen CM, Yi HY: Subtypes of alcohol dependence in a nationally representative sample. Drug Alcohol Depend 2007; 91(2–3):149–158Google Scholar