In This Issue
Environmental Factors in Schizophrenia
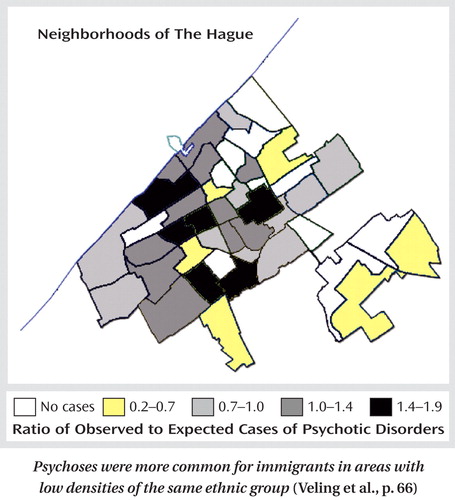
Three epidemiological studies bolster the evidence for infectious and social influences on the development of schizophrenia. Swedish national registers show an association between psychotic illness and childhood viral, but not bacterial, infections of the central nervous system (CNS). Dalman et al. (p. Original article: 59 ) analyzed hospitalizations for CNS infections before age 13 and psychotic illnesses from age 14 onward in children born during 1973–1985. Psychosis risk was almost tripled by childhood mumps exposure and was over 16 times as high after cytomegalovirus exposure. Using blood samples collected routinely by the U.S. military, Niebuhr et al. (p. Original article: 99 ) confirmed a relationship between schizophrenia and toxoplasmosis. IgG antibodies to Toxoplasma gondii were compared in service members medically discharged with schizophrenia between 1992 and 2001 and matched healthy subjects. The antibody level was nearly 25% higher for the subjects with schizophrenia in the 6 months preceding the diagnosis or after it. Dr. Alan Brown examines these two studies in an editorial on p. Original article: 7 . Veling et al. (p. Original article: 66 ) identified social isolation as a risk factor for psychotic disorders among immigrants in The Hague . City records provided the ethnic backgrounds and locations of residents who received a first diagnosis of psychotic disorder over 7 years. Immigrants in neighborhoods with high densities of immigrants from the same country had a rate of psychotic illness similar to that of native Dutch residents, but those in neighborhoods with low densities of the same ethnic group had a rate more than double that for the Dutch.
Perimenopausal Depression
The likelihood of major depression increases during perimenopause, generally ages 45–49. Women with histories of premenstrual syndrome or postpartum depression are at particular risk. Parry (CME, p. Original article: 23 ) summarizes the findings from studies showing an association between depressive episodes and higher levels of follicle-stimulating hormone. Estrogen alone has not been shown consistently to be efficacious in perimenopausal depression. It may, however, be valuable when added to a selective serotonin reuptake inhibitor (SSRI) for women whose depression is refractory to an SSRI alone.
Antidepressant Warning Did Not Increase Monitoring by Physicians
The 2003 Food and Drug Administration (FDA) advisory about antidepressants’ suicidal risk for children recommended close supervision after new prescriptions, yet contact between health care providers and patients taking antidepressants was no more likely after the advisory. Morrato et al. (p. Original article: 42 ) analyzed more than 200,000 records from 1998 to 2005 in a national claims database, comparing the percentage of patients with various frequencies of contact in the periods before and after the FDA warning. Neither of two standards for adequate supervision showed an increase for either children or adults. Dr. Graham Emslie discusses this issue in an editorial on p. Original article: 1 .
Substance Use Disorders in ADHD Families
Attention deficit hyperactivity disorder (ADHD) appears to share some familial determinants with drug, but not alcohol, dependence. Biederman et al. (CME, p. Original article: 107 ) found that boys with ADHD were more likely than comparison boys to develop drug dependence over 10 years and they had more relatives with drug dependence and with ADHD. Relatives’ risk for drug dependence was higher for boys with ADHD, and relatives’ risk of ADHD was higher for boys with drug dependence. However, risk for alcohol dependence in relatives was seen only in relatives of boys who had both alcohol dependence and ADHD. An editorial on these findings by Dr. Lenard Adler appears on p. Original article: 11 .



