In This Issue
Bipolar Disorder Recurrence in Pregnancy
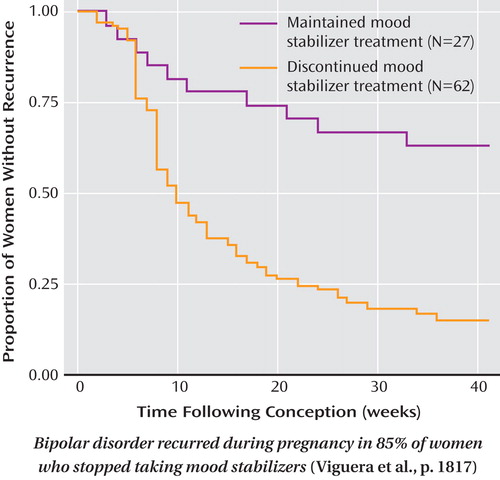
Women with bipolar disorder who stopped mood stabilizer treatment before becoming pregnant had an 85% rate of recurrence during pregnancy, compared with 37% of women who continued treatment. Rapid discontinuation produced a median time to recurrence of 2 weeks, compared to 22 weeks for gradual discontinuation. In their prospective study of 89 pregnant women with bipolar disorder, Viguera et al. (CME, p. Original article: 1817 ) also observed a striking predominance of depressive, rather than manic, episodes among the recurrences. Antidepressant treatment was not protective; it actually increased the risk of recurrence. The episodes of recurring illness spanned an average of more than 40% of the pregnancy for women who discontinued mood stabilizer treatment, but only 9% for women who continued treatment. Dr. Marlene Freeman discusses these findings in an editorial on p. Original article: 1771 .
Psychiatrists and Patients’ Religion
Survey results indicate that psychiatrists are less religious than other physicians but are more likely to discuss religion with patients and to encourage patients’ religious beliefs and practices. The survey of 1,144 physicians by Curlin et al. (p. Original article: 1825 ) also revealed that psychiatrists and other physicians share many perceptions about the positive influences of religion and spirituality, such as coping ability and positive outlook. However, psychiatrists were more likely to believe that religion and spirituality can cause negative emotions in patients. Dr. Burr Eichelman comments in an editorial on p. Original article: 1774 .
Brain Dysfunction in Borderline Personality Disorder
The behavioral dyscontrol of patients with borderline personality disorder when feeling negative emotions is associated with abnormal activity in several brain regions. Silbersweig et al. (p. Original article: 1832 ) report neural differences between borderline patients and healthy subjects while they performed a task involving motor inhibition and words they judged to have negative connotations. In relation to the comparison subjects, the patients had less activation of the subgenual anterior cingulate cortex, which helps modulate emotions. Lower activity also occurred in the medial orbitofrontal cortex, a brain region subserving behavioral responses; this deficit correlated with a measure of decreased constraint. An editorial by Dr. Greg Siegle on p. Original article: 1776 examines these results.
Depressive States and Stable Traits
Finding a long-term characteristic common to people who develop major depression could clarify who is at risk and how the illness arises. Two investigations focused on serotonin transport and on depressive personality disorder. Bhagwagar et al. (p. Original article: 1858 ) used positron emission tomography with a recently developed, more selective radioactive tracer to measure the protein regulating serotonin transport in the brain. The availability of the serotonin transporter protein in eight brain regions was similar in 24 healthy men and 20 medication-free men recovered from major depression, suggesting that it returns to normal after recovery. Ørstavik et al. (CME, p. Original article: 1866 ) investigated possible overlap between major depression and depressive personality disorder, which is characterized by pervasive depressive thoughts and behaviors. Of 2,801 twins from monozygotic and dizygotic pairs, 14% had a lifetime history of major depression and 2% met criteria for depressive personality disorder. Major depression was common among those with depressive personality disorder, but not vice versa. Although they shared a substantial proportion of genetic and environmental risk factors, major depression was influenced by additional genetic factors.



