Child Murder by Mothers: A Critical Analysis of the Current State of Knowledge and a Research Agenda
Abstract
OBJECTIVE: Maternal filicide, or child murder by mothers, occurs more frequently in the United States than in other developed nations. However, little is known about factors that confer risk to children. The authors review the literature to identify predictors of maternal filicide and identify gaps in knowledge about maternal filicide. METHOD: Databases were systematically searched for studies of maternal filicide and neonaticide (murder in the first day of life) that were conducted in industrialized countries and were published in peer-reviewed, English-language publications after 1980. RESULTS: Women who committed filicide varied greatly by the type of sample studied. Neonaticide was often committed by young, poor, unmarried women with little or no prenatal care. CONCLUSIONS: The results of the review suggest that little is known about the predictors of maternal filicide and that a systematic, focused program of research on reliable markers for maternal filicide is needed to better prevent these events.
Among children under age 5 years in the United States who were murdered in the last quarter of the 20th century, 61% were killed by their own parents: 30% were killed by their mothers, and 31% by their fathers (1). Estimates by the Centers for Disease Control and Prevention for 1994 indicated that homicide was the fourth leading cause of death for preschool children and the third leading cause of death among children from ages 5–14 years (2). In the United States, the incidence of homicide of children less than 1 year old has increased over the past quarter-century (1). Compared to other developed nations, the United States has the highest rate of child homicide: 8.0/100,000 for infants, 2.5/100,000 for preschool-age children (age 1–4 years), and 1.5/100,000 for school-age children (age 5–14 years) (3). In contrast, Canada’s reported rate for homicide of infants was less than half that of the United States: 2.9/100,000 (3). Furthermore, multiple authors have suggested that rates of child murder by parents are underestimated in epidemiological studies of child death (4–6).
Maternal filicide, defined as child homicide by mothers, is a problem that transcends national boundaries. However, little is known about the circumstances and factors associated with its commission, and this lack of knowledge makes prevention difficult. Two early seminal works, by Resnick in the United States and d’Orban in the United Kingdom, are often cited. In 1969, Resnick (7) reviewed the world psychiatric literature on filicide and found a high frequency of depression, psychosis, prior use of psychiatric services, and suicidality (suicidal behavior or suicidal thoughts, intent, or plan) among mothers who commit filicide. Resnick (8) later coined the term “neonaticide” to describe murder of a neonate within the first 24 hours of life. Mothers committing neonaticide were typically younger and unmarried. They had unwanted pregnancies and no prenatal care. In 1979, d’Orban (9) studied filicide by mothers admitted for psychiatric observation to the hospital ward of a prison. The findings suggested an association between maternal filicide and the presence of certain stressors in the mother’s life, such as being a survivor of domestic violence, early parental separation, and suicidality. In the case of neonaticide, d’Orban confirmed an association with unmarried status and younger mean maternal age and found a lack of association with depression or psychosis. Although women who kill their children are often labeled as “mad” (mentally ill) or “bad” (chronically abusive) (10), no consistent approach exists for defining the population of offenders. Data have rarely been collected on the basis of a priori theories. Nevertheless, theories regarding the psychological bases for filicide are abundant (7, 11, 12).
To advance the knowledge base about the predictors of maternal filicide and neonaticide, we addressed three questions through a critical analysis of the extant research literature: 1) What are the predictors or risk factors for maternal neonaticide and filicide? 2) How do these risk factors vary by the type of population studied? and 3) Which mentally ill mothers are at risk for committing neonaticide or filicide?
Method
The analyses were based on extensive database searches, including searches through PubMed (Medline), PsychINFO, the Psychology and Behavioral Sciences Collection, and Sociological Abstracts. Search terms included “filicide,” “infanticide,” “neonaticide,” and “fatal child maltreatment.”
Study Inclusion Criteria
The studies that were selected for review had the following characteristics:
| 1. | They dealt with maternal filicide only or separated maternal filicide offenders for some portion of analysis. This distinction was made in the selection because of the likelihood that different risk factors exist for paternal and maternal filicide. | ||||
| 2. | They were conducted in industrialized countries. We focused on these settings because of the likelihood that different risk factors for infant homicide exist in underdeveloped countries (13). In underdeveloped countries, varying cultural, legal, and/or economic factors could constitute an external incentive for filicide unrelated to the mothers’ psychological state. For example, a preference for male rather than female offspring in certain societies could influence filicide. | ||||
| 3. | They were published in English-language, peer-reviewed journals or books after 1980, and they included contemporary samples. | ||||
Study Organization
The selected studies were grouped according to population type, age of child victims, and geographic location.
Population type
General population studies may yield different results than studies of specialized populations, such as prison or psychiatric populations. Administrative record samples were defined as being more generalized, often including both psychiatric and correctional populations, as well as cases of maternal filicide-suicide, and were not weighted toward subjects who were adjudicated guilty or those with psychiatric dispositions. These studies cited coroners’ records, newspaper reports, home office reports, or national statistics as data sources. Populations classified as corrections samples were diverse, ranging from women who were incarcerated (14, 15) to those described in judicial papers (16). Psychiatric populations were defined as mothers who were psychiatrically hospitalized or who were sampled from a setting that was likely to include subjects with psychiatric disorders, such as mothers referred for psychiatric evaluations subsequent to neonaticide or filicide.
Age of child victims
We distinguished between children killed when they were neonates and those killed when they were infants (within the first year of life), because neonaticide and infanticide may be influenced by different factors, compared to other filicides (8).
Geographic location
Geographic locations were classified as those inside or outside the United States. Rates of homicide and of filicide vary by country (17) and by culture. Furthermore, more than 20 countries have legislation that makes special provisions for maternal infanticide (18).
Search Results
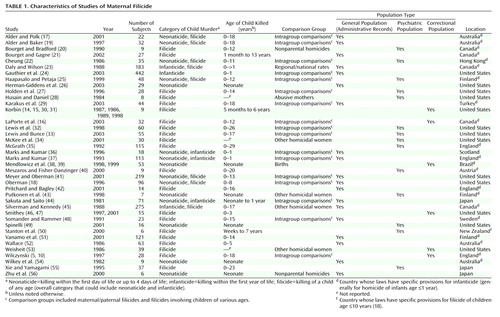
The database search yielded more than 250 references in the extant literature. The majority consisted of case reports, reports on series of filicide cases, and conceptual theoretical papers, and these publications were excluded. Eighty-three studies of child homicide were identified (4, 5, 10, 14–99 [some studies were described in more than one publication]). Forty-two of these 83 studies reported on child homicide but did not distinguish maternal filicide from paternal filicide or murder by a stepparent or a nonparent (4, 57–81, 83–89, 91–99). Those studies were not included in our analysis because they did not yield specific information about maternal perpetrators. Two studies of maternal filicide were excluded because they presented data that were primarily historical (dating to 1850 or the early 1900s) and did not separately consider more recent data (82, 90). After exclusions, there remained 39 studies that were appropriate for use in our analysis. The characteristics of those 39 studies (5, 10, 14–56 [some studies were described in more than one publication]) are listed in Table 1.
Results
All 39 studies we reviewed were retrospective in design. Ten included retrospective interviewing of mothers. Twenty-six included a comparison group. Many of the studies included intragroup comparisons.
Of the 39 studies specifically reporting on maternal child homicide, 13 were conducted in the United States and 26 were conducted in other countries. Thirteen other nations were represented: Canada (five studies), nations within the United Kingdom (five studies), Australia (four studies), Finland (three studies), Japan (three studies), with one study each conducted in Austria, Brazil, Hong Kong, New Zealand, Sweden, and Turkey. Four U.S. studies addressed neonaticide; three analyzed data from samples of administrative records, and one analyzed data from a psychiatric population (Table 1). Of the studies conducted outside of the United States, 11 addressed neonaticide; seven of those studies were based on administrative records, three examined data from psychiatric populations (either hospitalized or psychiatrically evaluated women), and one analyzed data from a correctional population. With regard to maternal infanticide (maternal filicide within the first 12 months of life, often defined by statute in countries outside the United States), one study of an administrative records sample was conducted in the United States and five were done in other countries.Studies of maternal filicide had various inclusion criteria for the child’s age. Many studies combined analysis of neonaticide with that of other filicides. Ten such studies of maternal filicide were conducted within the United States: two with administrative records, five in psychiatric populations, and three in correctional populations. Nineteen such studies were conducted outside the United States: 10 with administrative records, seven in psychiatric populations, and two in correctional populations.
Neonaticide
The three administrative record sample studies of neonaticide in the United States revealed that maternal perpetrators were likely to be unmarried, to have a mean and modal age in the late teenage years, to have low socioeconomic status, and to reside with parents or other relatives. The perpetrators had high rates of denied or concealed pregnancy and a relative lack of prenatal care. In the single U.S. study of a psychiatric population of women who committed neonaticide (49), the mothers had an older mean age (24 years) and middle to low socioeconomic status. The subjects in this study exhibited denial of pregnancy and frequently reported depersonalization, dissociative hallucinations, and intermittent amnesia.
Multiple studies of neonaticide from outside the Untied States were based on administrative records samples. They revealed that the maternal perpetrators were largely unmarried young mothers who lived with their parents, lacked prenatal care, concealed or denied their pregnancies, and showed no evidence of premorbid axis I psychiatric disorders.
In non-U.S. studies of psychiatric populations of mothers who committed neonaticide, the samples consisted primarily of unmarried women with an older mean age (20–26 years) and infrequent prenatal care. Some studies of non-U.S. psychiatric populations of mothers who committed neonaticide reported a relative lack of mental illness after psychiatric evaluation in the mothers (9, 22, 25), while another reported a high rate of personality disorders or psychosis in the mothers (43).
The non-U.S. correctional studies (including historical data correlated with current data) revealed that neonaticidal mothers generally were single, illiterate, nulliparous, younger (mean age=22 years), and without prior mental illness. In a study in Japan, neonaticide was further classified into cases of “anomie,” in which the mothers had the general characteristics just described, and “mabiki” (“thinning out”), in which impoverished married women or couples killed neonates because of poverty (44). The mothers in cases of mabiki did not deny their pregnancies.
Infanticide
The single U.S. study that presented separate data concerning infanticide (filicide in first 12 months of life) was a macro-level study that revealed a relationship of maternal infanticide to economic stress (25). The non-U.S. administrative records sample studies of infanticide revealed that the mothers had a mean age in the early 20s and low rates of employment. Many mothers had psychiatric disorders. For example, 72% of the mothers in the study conducted in Japan had psychiatric disorders (44). There was a high frequency of physical anomalies among the child victims in the study conducted in Japan (44).
Filicide
Studies based on administrative records samples of maternal filicide occasionally included cases of filicide-suicide, and these mothers, for obvious reasons, would not be part of psychiatric or prison samples. The two U.S. administrative records sample studies of filicide (reported separately from neonaticide) found that the mothers were often poor, full-time caregivers who were socially isolated and may themselves have been victims of domestic abuse. Neglectful and abusive mothers often had problems with substance abuse as well.
Certain studies divided mothers into groups on the basis of a proposed typology. This strategy found groups of mothers with variable rates of both mental illness and previous abuse of the child. Groups of mothers who committed “purposeful homicide” often killed their children in the context of mental illness, failed relationships, and “devotion” to the child (41).
Studies of maternal filicide offenders drawn from psychiatric populations in the United States noted high rates of psychosis, depression, suicidality, prior use of psychiatric services, and, in some studies, decreased intelligence. Mothers who committed filicide were more frequently married, compared with neonaticidal mothers, and had a high frequency of unemployment, alcohol use, and personal history of abuse.
Maternal filicide offenders in the studies of U.S. correctional populations were frequently victims of abuse themselves. Many had limited education, poor social support, and a history of substance abuse. In addition, they were often unmarried and unemployed, and some viewed the child they killed as abnormal.
Administrative records sample studies of maternal filicide conducted outside the United States found mental illness (psychosis, depression with suicidality) in approximately one-half of the mothers. Some of these studies noted histories of child abuse and domestic violence, and some noted child-related factors, such as persistent crying, as precipitants of the mothers’ violence. Mothers who committed filicide were frequently socioeconomically disadvantaged and had primary responsibility for their children. Studies of psychiatric samples conducted outside the United States noted high rates of psychiatric symptoms, particularly depression and psychosis, as well as prior use of psychiatric services, prior psychiatric admissions, and suicidality. The mothers often experienced considerable life stress, including being abused themselves. Filicidal mothers in non-U.S. correctional populations were also likely to have a history of previous use of psychiatric services and high rates of mental illness (depression and psychosis). The mothers in these cases of filicide were likely to have social and economic stresses, a history of abuse, unsupportive partners, primary caregiver status, and difficulties caring for the child.
In this critical analysis, we used these studies to identify factors that distinguish mentally ill mothers who are more likely to kill their children. We reconsidered the 14 studies of filicide in samples from psychiatric populations to identify studies that used control groups that were appropriate for the determination of possible risk factors. Although many of these studies included comparison groups, such as other female homicide offenders, there were no studies that compared mentally ill filicidal mothers with mentally ill mothers of similar socioeconomic status who did not kill their children. In the study with the most suitable design, which compared abusive mothers with mothers who committed filicide, data for only eight maternal filicides were analyzed (28). Because of the limitations of the available studies, we were unable to identify the situational or personal factors that put mentally ill mothers at risk for filicide.
Discussion
We found that the research on child murder by mothers, especially within the United States, was sparse. Studies of neonaticide that used administrative records samples and correctional populations both inside and outside the United States had fairly consistent findings. They frequently showed a pattern of powerlessness, poverty, and alienation in the lives of the women studied. However, the common factors, such as being young, poor, and undereducated and living with one’s parents, describe a huge segment of the female population. There were virtually no distinguishing features to suggest which young, poor, and undereducated women with poor prenatal care were at risk for neonaticide. It is not surprising that the samples of neonaticide offenders from psychiatric populations differed from those in administrative records samples regarding the presence of mental illness, but data on this characteristic were sparse, and the results differed across countries.
Some of these studies noted that women who committed neonaticide had a high probability of denying or concealing their pregnancy. Denial or concealment of pregnancy may indeed be a predictor of neonaticide, but such behavior would be difficult to identify prospectively. The lack of prenatal care may also be a valid predictor of neonaticide. Additional, careful study is needed to elucidate factors related to denial of pregnancy in women who receive no prenatal care.
Knowledge about maternal filicide after the first day of life is even more meager. Offenders in psychiatric populations in the United States and other nations had high rates of previous mental health services use, depression, suicidality, and psychosis, as expected of psychiatric patients. Studies of maternal filicide in corrections populations noted social disadvantage in offenders. Studies conducted outside of the United States documented more mental illness in offenders.
England’s Infanticide Act, the modern version of which became law in 1938, was based on the concepts of puerperal and lactational insanity (18). The Act reduced the charge from murder to manslaughter for a woman who killed her infant under age 1 year if “the balance of her mind was disturbed by reason of her not having fully recovered from the effect of giving birth to a child or by reason of the effect of lactation” (100). More than 20 countries currently have such legislation, including Canada and much of Australia, but not the United States (18). In these countries, infanticide laws often result in the woman’s receiving probation or referral to mental health treatment rather than incarceration (18). It is noteworthy that such legislation does not require that the mother have a formally diagnosable mental illness. Therefore, a nondepressed and nonpsychotic mother who commits neonaticide may be shown greater lenience than a psychotic and depressed mother who kills her 13-month-old child. Many severely mentally ill mothers may not be considered under legislation that applies only to death of children under age 1 year; a recent study found that the mean age of child victims of mothers found not guilty by reason of insanity in two states was older than 3 years (101). We would expect findings to be somewhat skewed when considering study results from various countries. However, samples in these studies often included mothers who killed children older than age 1 year. Specifically, one might expect that women in the United States who successfully plead insanity and procure a psychiatric disposition would be more psychiatrically ill than those with a psychiatric disposition in countries with infanticide laws. Likewise, women who had criminal dispositions in countries with infanticide laws might be less likely to be mentally ill. However, other things being equal, results from the more general administrative records samples may be similar.
Maternal filicide studies based on samples of the general population within the United States are sorely needed to develop strategies for prevention. Several studies of maternal filicide separated results on the basis of proposed typologies of motivations among mothers who commit filicide. In some studies, the age of the child that was killed was reported, but there was no discussion of the child’s age in relation to the common factors in the lives of their mothers. The inclusion criteria for the age of the child victims varied drastically across studies, making the development of conclusions difficult. Because of the differing legal definition of infanticide among countries, comparison to U.S. incidence rates of filicide may be difficult. Based on our understanding of childhood abuse, we hypothesize that after the first day of life, risk factors for filicide are related to the age of the child. The literature supports the supposition that fatal abuse may be more likely to occur in younger children and that older children are more at risk from purposeful homicides. However, the existing research on filicide cannot be used to affirm this supposition.
The nature of filicide varies within the population of women studied. Consideration must be given to the appropriateness of the questions asked about the population and the selection of comparison groups. For example, within a mentally ill population, data should be sought to help inform clinicians why one mother with psychotic depression is more likely to kill her child than another mother with psychotic depression.
What we know about maternal filicide is specific to the population studied. Few factors are consistent across populations; thus overall, we know very little about which children are at risk for death at the hands of their mothers. All of the studies reviewed here were retrospective, and most were descriptive. None of the studies included calculation of relative risks for filicide in women with specific disorders or maternal characteristics strongly associated with filicide. However, they did provide general descriptions of mothers who had committed filicide, and from these descriptions we can extrapolate some potential risk factors. Women at risk for neonaticide are often young and unmarried, deny or conceal the pregnancy, and lack prenatal care. The factors associated with maternal filicide appear to be nonspecific but seem likely to include past use of psychiatric services and a history of suicidality and depression or psychosis. However, the factors associated with maternal filicide are likely to be different for women who are psychiatrically ill, compared to those who are not psychiatrically ill.
Investigators who conducted research in psychiatric populations often had access to detailed psychological information about the maternal perpetrators of filicide, but their conclusions are limited in generalizability. Maternal mental illness appears to play a varying role in filicide. Descriptions of filicidal mothers were highly dependent on the source of the sample. Imprisoned U.S. perpetrators of maternal filicide were understandably less likely to be mentally ill than mothers who were psychiatrically hospitalized. These differences in study populations make it difficult to draw general conclusions about which mothers are at risk. Furthermore, although there were few studies, some were difficult to categorize because they were based on very specific populations that may have had some overlap. For example, a study of women referred for psychiatric evaluation after commission of neonaticide (49) was classified as a psychiatric population study because it would have included a preselected group of women who were more likely to have psychiatric disorders than would a general correctional population, although it could be argued that such a population should be considered a correctional population because the women were pretrial detainees at the time.
This critical analysis suggests that clearer parameters are needed for research in this area. There is a lack of standardization in filicide research regarding the age of children who constitute filicide victims. The children in the studies we reviewed ranged from neonates to young adults as old as age 29 years. We propose that future filicide research consider including only children under age 18 years, because they are minors and still of school age. The existing studies did not examine the possibility that contextual factors may vary according to the age of the child victim. No study reported on characteristics of the mothers based on the age of the child who was killed, other than in cases of neonaticide or infanticide. It is interesting to note that when study population samples were separated by country, different factors appeared to emerge. Less variability occurred in the findings of neonaticide studies among nations than among population sample types.
Very few American general population studies were conducted. The epidemiological studies that do exist do not differentiate maternal filicide from other child homicides (69, 93). American infants at risk of homicide are known to be born to young, undereducated mothers with low socioeconomic status who do not obtain timely prenatal care. However, this research is limited by lack of classification of the homicide perpetrator as the mother, the father, or a nonparent. Psychiatric diagnoses are frequently made after the homicide, when women may develop depression or posttraumatic stress disorder in reaction to commission of the filicide. These diagnoses may not necessarily reflect the women’s psychiatric status before the filicide. Furthermore, it is often unclear how rigorously the psychiatric diagnostic criteria were applied.
In a closely related area of research, two studies found a high incidence of filicidal thoughts in mentally ill women (102, 103). The study by Chandra et al. (103) of postpartum severely mentally ill women in India found that 43% had infanticidal ideation and 36% exhibited infanticidal behavior. Infanticidal behavior was associated with female gender of the infant, adverse maternal reaction to separation from the infant, and psychotic ideas relating to the infant. These findings are a step toward developing a profile of mentally ill mothers who may be at risk for filicidal deeds. Further descriptive research is needed to explore the character and quality of parenting by mentally ill women (104). This area of research is important because approximately one-quarter of the women referred to psychiatric services have a child under age 5 years (104). Similar studies of women who are not mentally ill—particularly women who are young, poor, and undereducated and who fail to obtain prenatal care—are also critical. For example, a study in a nonpsychiatric population found that 70% of mothers of colicky infants had explicit aggressive thoughts toward their infants, and 26% of these mothers had infanticidal thoughts during the infant’s episodes of colic (105). Development of intervention strategies depends on a better understanding of the prevalence of these thoughts and the characteristics of mothers who are likely to act on these thoughts.
Research Agenda for Maternal Filicide Studies
Given that the reported incidence of filicide is increasing and given the limitations of the research literature, what are the most important research needs in this area? Although prospective studies are considered stronger than retrospective studies for establishing risk relationships, the rarity of filicide makes such studies impractical. However, well-conceptualized cross-sectional studies, with contemporaneous investigation of the circumstances surrounding all child deaths in a given catchment area, are feasible. These investigations could examine factors associated with different types of filicide (e.g., filicide resulting from negligence, recklessness, or intentional acts). In addition, case-control studies examining features of filicide victims whose mothers were reported to child protective services for abuse could be compared to those of abused children who are not killed. The findings could point to characteristics that may identify women who are at high risk for killing their children.
Future studies of filicide in the United States should build on the knowledge gained from studies in other nations and should strive to meet the following criteria. First, the studies should contain comparison groups, such as mentally ill mothers or abusive mothers who do not kill their children. We need well-controlled studies comparing mothers in the general population who did and did not commit filicide, as well as mentally ill mothers who did and did not commit filicide.
Second, future studies should examine specific perpetrator subpopulations that would include mothers with and without key risk factors. An optimal strategy would be to examine such factors across the children’s life span. Groups that should be targeted for study include women with no prenatal care, abusive mothers, and mentally ill mothers. These focused studies might allow the construction of risk profiles for filicide.
Third, future studies should investigate a large number of possible risk factors. Some factors, such as depression and social problems, have a widespread presence in the general population. Therefore, for mothers who commit filicide, a constellation of risk factors is likely to be more important than the presence of a single factor. Clusters of significant risk factors for filicide may include demographic factors, social milieu, psychiatric history, victim characteristics, specific situational factors, prior family conflict and violence, and a history of contact with social service agencies. All of these factors have all been suggested as candidates needing further study in the context of filicide risk (5). In future studies, researchers should seek to delineate which abusive mothers are most at risk for committing filicide.
Fourth, studies in the national U.S. population would be optimal to gain a sufficient sample size for this relatively infrequent crime. Although some potentially informative trends have been noted from international studies, different homicide and filicide rates across nations make inferences about risk factors somewhat problematic.
Finally, an important area of research concerns mothers who kill their children and themselves (filicide-suicide), because these mothers are not included in either correctional or psychiatric samples. Historically, they represent a significant proportion (16%–29%) of filicidal mothers (23, 48, 106). To facilitate such studies, death records of filicide victims should be augmented with information about perpetrators. This goal would be accomplished by examining the records of all filicide deaths reported to coroners.
Future Data Sources
Standard reporting systems often do not provide specific data regarding filicide. Although current state and national databases link infant birth and death records, information about the identity of the homicide perpetrator is not similarly linked. Also, there is no current linkage of birth and death records for children over the age of 12 months. This limitation effectively eliminates critical information from the database in the case of older filicide victims. The Centers for Disease Control and Prevention is developing the National Violent Death Reporting System, which is funded in some states (107). When this system is in operation, it will link coroner, judicial, and law enforcement records, which will facilitate study in this area of homicide. Also, the U.S. Federal Bureau of Investigation has begun examining data for a large sample of mothers who have killed their children; this project makes use of information from the investigating law enforcement agencies and prosecutors’ offices (K. Beyer, personal communication, 2004).
To facilitate understanding and to potentially intervene in this public health issue, certain states are also taking an active role. All 50 states have Child Fatality Review teams (108). In Ohio, for example, an interdisciplinary team evaluates the deaths of children age ≤18 years and examines factors that may relate to prevention. However, the teams do not necessarily investigate the child’s death until after prosecution of the perpetrator, which could delay review of many maternal filicide cases. For optimal data collection, every filicide case that is evaluated by coroners should be contemporaneously investigated by coroners’ inquests. Also, a survey given to new mothers, PRAMS (the Pregnancy Risk Assessment Monitoring System) (109), does not routinely include questions about mental health concerns, although states may opt to add such questions.
The office of the U.S. Surgeon General is planning prevention strategies for child maltreatment (110, 111). Psychiatry, public health, and the social sciences should collaborate across the traditional disciplinary boundaries to share approaches and resources that would improve our knowledge of the determinants of filicide. Without adequate data about who is at risk, preventive interventions cannot be developed. With the exception of data for neonaticide, public health data supporting targets for intervention to prevent filicide are lacking. Researchers in public health should be guided to modify data collection and organization to include specific data about perpetrators of child homicide. Their efforts should also include follow-up of cohorts of mentally ill mothers, with inquiry about filicidal intentions as an indicator. More data must be gathered before more appropriate prevention efforts can be targeted to avert these family tragedies.
 |
Received Aug. 29, 2004; revision received Jan. 7, 2005; accepted Feb. 23, 2005. From the Department of Psychiatry, Case Western Reserve University and University Hospitals of Cleveland. Address correspondence and reprint requests to Dr. Friedman, Department of Psychiatry/Hanna Pavilion, University Hospitals of Cleveland/Case Western Reserve University, 11100 Euclid Ave., Cleveland, OH 44106; [email protected] (e-mail). The authors thank Dr. Penelope Friedman and Dr. Jill Korbin for their insights. No financial support was given for this review.
1. US Department of Justice: Homicide Trends in the United States: Infanticide. http://www.ojp.usdoj.gov/bjs/homicide/children.htm [updated 2001]Google Scholar
2. Rates of homicide, suicide, and firearm-related death among children—26 industrialized countries. MMWR Morb Mortal Wkly Rep 1997; 46:101–105Medline, Google Scholar
3. Finkelhor D: The homicides of children and youth: a developmental perspective, in Out of the Darkness: Contemporary Perspectives on Family Violence. Edited by Kantor GK, Jasinski JL. Thousand Oaks, Calif, Sage Publications, 1997, pp 17–34Google Scholar
4. Ewigman B, Kivlahan C, Land G: The Missouri Child Fatality Study: underreporting of maltreatment fatalities among children younger than five years of age. Pediatrics 1993; 91:330–337Medline, Google Scholar
5. Wilczynski A: Child Homicide. London, Oxford University Press/Greenwich Medical Media, 1997Google Scholar
6. Botash AS, Blatt S, Meguid V: Child abuse and sudden infant death syndrome. Curr Opin Pediatr 1998; 10:217–223Crossref, Medline, Google Scholar
7. Resnick PJ: Child murder by parents: a psychiatric review of filicide. Am J Psychiatry 1969; 126:325–334Link, Google Scholar
8. Resnick PJ: Murder of the newborn: a psychiatric review of neonaticide. Am J Psychiatry 1970; 126:1414–1420Link, Google Scholar
9. d’Orban PT: Women who kill their children. Br J Psychiatry 1979; 134:560–571Crossref, Medline, Google Scholar
10. Wilczynski A: Mad or bad? child killers, gender and the courts. Br J Criminol 1997; 37:419–436Crossref, Google Scholar
11. Rodenburg M: Child murder by depressed parents. Can J Psychiatry 1971; 16:41–48Google Scholar
12. Harder T: The psychopathology of infanticide. Acta Psychiatr Scand 1967; 43:196–245Crossref, Medline, Google Scholar
13. Oberman M: Mothers who kill: cross-cultural patterns in and perspectives on contemporary maternal filicide. Int J Law Psychiatry 2003; 26:493–514Crossref, Medline, Google Scholar
14. Korbin JE: Incarcerated mothers’ perceptions and interpretations of their fatally maltreated children. Child Abuse Negl 1987; 11:397–407Crossref, Medline, Google Scholar
15. Korbin JE: Childhood histories of women imprisoned for fatal child maltreatment. Child Abuse Negl 1986; 10:331–338Crossref, Medline, Google Scholar
16. Laporte L, Poulin B, Marleau J, Roy R, Webanck T: Filicidal women: jail or psychiatric ward? Can J Psychiatry 2003; 48:94–109Crossref, Medline, Google Scholar
17. Alder C, Polk K: Child Victims of Homicide. Cambridge, UK, Cambridge University Press, 2001Google Scholar
18. Oberman M: Mothers who kill: coming to terms with modern American infanticide. Am Crim Law Rev 1996; 34:2–109Google Scholar
19. Alder CM, Baker J: Maternal filicide: more than one story to be told. Women Crim Justice 1997; 9:15–39Crossref, Google Scholar
20. Bourget D, Bradford JM: Homicidal parents. Can J Psychiatry 1990; 35:233–238Crossref, Medline, Google Scholar
21. Bourget D, Gagne P: Maternal filicide in Quebec. J Am Acad Psychiatry Law 2002; 30:345–351Medline, Google Scholar
22. Cheung PTK: Maternal filicide in Hong Kong, 1971–1985. Med Sci Law 1986; 26:185–192Crossref, Medline, Google Scholar
23. Daly M, Wilson M: Killing children: parental homicide in the modern West, in Homicide. Edited by Daly M, Wilson M. New York, Aldine de Gruyter, 1988, pp 61–93Google Scholar
24. Gauthier DK, Chaudoir NK, Forsyth CJ: A sociological analysis of maternal infanticide in the United States 1984–1996. Deviant Behav 2003; 24:393–405Crossref, Google Scholar
25. Haapasalo J, Petaja S: Mothers who killed or attempted to kill their child: life circumstances, childhood abuse, and types of killing. Violence Vict 1999; 14:219–239Crossref, Medline, Google Scholar
26. Herman-Giddens ME, Smith JB, Mittal M, Carlson M, Butts JD: Newborns killed or left to die by a parent: a population-based study. JAMA 2003; 189:1425–1429Crossref, Google Scholar
27. Holden CE, Burland AS, Lemmen CA: Insanity and filicide: women who murder their children. New Dir Ment Health Serv 1996; 69:25–34Crossref, Medline, Google Scholar
28. Husain A, Daniel A: A comparative study of filicidal and abusive mothers. Can J Psychiatry 1984; 29:596–598Crossref, Medline, Google Scholar
29. Karakus M, Ince H, Ince N, Arican N, Sozen S: Filicide cases in Turkey, 1995–2000. Croat Med J 2003; 44:592–595Medline, Google Scholar
30. Korbin JE: Fatal maltreatment by mothers: a proposed framework. Child Abuse Negl 1989; 13:481–489Crossref, Medline, Google Scholar
31. Korbin JE: “Good mothers,” “babykillers,” and fatal child maltreatment, in Small Wars: The Cultural Politics of Childhood. Edited by Scheper-Hughes N, Sargent C. Berkeley, University of California Press, 1998, pp 253–276Google Scholar
32. Lewis CF, Baranoski MV, Buchanan JA, Benedek EP: Factors associated with weapon use in maternal filicide. J Forensic Sci 1998; 43:613–618Medline, Google Scholar
33. Lewis CF, Bunce SC: Filicidal mothers and the impact of psychosis on maternal filicide. J Am Acad Psychiatry Law 2003; 31:459–470Medline, Google Scholar
34. McKee GR, Shea SJ, Mogy RB, Holden CE: MMPI-2 profiles of filicidal, mariticidal, and homicidal women. J Clin Psychol 2001; 57:367–374Crossref, Medline, Google Scholar
35. McGrath PG: Maternal filicide in Broadmoor Hospital. J Forensic Psychiatry 1992; 3:271–297Crossref, Google Scholar
36. Marks MN, Kumar R: Infanticide in Scotland. Med Sci Law 1996; 36:201–204Google Scholar
37. Marks MN, Kumar R: Infanticide in England and Wales. Med Sci Law 1993; 33:329–339Crossref, Medline, Google Scholar
38. Mendlowicz MV, Jean-Louis G, Gekker M, Rapaport MH: Neonaticide in the city of Rio de Janeiro: forensic and psycholegal perspectives. J Forensic Sci 1999; 44:741–745Medline, Google Scholar
39. Mendlowicz MV, Rapaport MH, Mecler K, Golshan S, Moraed TM: A case-control study on the socio-demographic characteristics of 53 neonaticidal mothers. Int J Law Psychiatry 1998; 21:209–219Crossref, Medline, Google Scholar
40. Meszaros K, Fisher-Danzinger D: Extended suicide attempt: psychopathology, personality and risk factors. Psychopathology 2000; 33:5–10Crossref, Medline, Google Scholar
41. Meyer CL, Oberman M: Mothers Who Kill Their Children: Understanding the Acts of Moms From Susan Smith to the “Prom Mom.” New York, New York University Press, 2001Google Scholar
42. Pritchard C, Bagley C: Suicide and murder in child murderers and child sexual abusers. J Forensic Psychiatry 2001; 12:269–286Crossref, Google Scholar
43. Putkonen H, Collander J, Honkasalo ML, Lönnqvist J: Finnish female homicide offenders 1982–92. J Forensic Psychiatry 1998; 9:672–684Crossref, Google Scholar
44. Sakuta T, Saito S: A socio-medical study on 71 cases of infanticide in Japan. Keio J Med 1981; 30:155–168Crossref, Medline, Google Scholar
45. Silverman RA, Kennedy LW: Women who kill their children. Violence Vict 1988; 3:113–127Crossref, Medline, Google Scholar
46. Smithey M: Maternal infanticide and modern motherhood. Criminal Justice 2001; 13:65–83Google Scholar
47. Smithey M: Infant homicide at the hands of mothers: toward a sociological perspective. Deviant Behav 1997; 18:255–272Crossref, Google Scholar
48. Somander LK, Rammer LM: Intra- and extra-familial child homicide in Sweden 1971–1980. Child Abuse Negl 1991; 15:45–55Crossref, Medline, Google Scholar
49. Spinelli MG: A systematic investigation of 16 cases of neonaticide. Am J Psychiatry 2001; 158:811–813Link, Google Scholar
50. Stanton J, Simpson A, Wouldes T: A qualitative study of filicide by mentally ill mothers. Child Abuse Negl 2000; 24:1451–1460Crossref, Medline, Google Scholar
51. Vanamo T, Kauppo A, Karkola K, Merikanto J, Rasanen E: Intra-familial child homicide in Finland 1970–1994: incidence, causes of death and demographic characteristics. Forensic Sci Int 2001; 117:199–204Crossref, Medline, Google Scholar
52. Wallace A: Homicide: The Social Reality. Sydney, Australia, New South Wales Bureau of Crime Statistics and Research, 1986Google Scholar
53. Weisheit RA: When mothers kill their children. Soc Sci J 1986; 23:439–448Crossref, Google Scholar
54. Wilkey I, Pearn J, Petrie G, Nixon J: Neonaticide, infanticide, and child homicide. Med Sci Law 1982; 22:31–34Crossref, Medline, Google Scholar
55. Xie L, Yamagami A: How much of child murder in Japan is caused by mentally disordered mothers? Intern Med J 1995; 2:309–313Google Scholar
56. Zhu BL, Oritani S, Ishida K, Quan L, Sakoda S, Fujita MQ, Maeda H: Child and elderly victims in forensic autopsy during a recent 5 year period in the southern half of Osaka city and surrounding areas. Forensic Sci Int 2000; 113:215–218Crossref, Medline, Google Scholar
57. Abel EL: Childhood homicide in Erie County, New York. Pediatrics 1986; 77:709–713Medline, Google Scholar
58. Anderson R, Ambrosino R, Valentine D, Lauderdale M: Child deaths attributed to abuse and neglect: an empirical study. Child Youth Serv Rev 1983; 5:75–89Crossref, Google Scholar
59. Berkowitz CD: Fatal child neglect. Adv Pediatr 2001; 48:331–361Medline, Google Scholar
60. Brenner RA, Overpeck MD, Trumble AC, DerSimonian R, Berendes H: Deaths attributed to injuries in infants. Pediatrics 1999; 103:968–974Crossref, Medline, Google Scholar
61. Brewster AL, Nelson JP, Hymel KP, Dolby DR, Lucas DR, McCanne TR, Milner JS: Victim, perpetrator, family and incident characteristics of 32 infant maltreatment deaths in the United States Air Force. Child Abuse Negl 1998; 22:91–101Crossref, Medline, Google Scholar
62. Briggs CM, Cutright P: Structural and cultural determinants of child homicide: a cross-national analysis. Violence Vict 1994; 9:3–16Crossref, Medline, Google Scholar
63. Chew KSY, McCleary R, Lew MA, Wang JC: The epidemiology of child homicide: California, 1981–1990. Homicide Studies 1999; 3:151–169Crossref, Google Scholar
64. Christoffel KK, Anzinger NK, Amari M: Homicide in childhood: distinguishable patterns of risk related to developmental levels of victims. Am J Forensic Med Pathol 1983; 4:129–137Crossref, Medline, Google Scholar
65. Christoffel KK, Liu K: Homicide death rates in childhood in 23 developed countries: US rates atypically high. Child Abuse Negl 1983; 7:339–345Crossref, Medline, Google Scholar
66. Christoffel KK: Homicide in childhood: a public health problem in need of attention. Am J Public Health 1984; 74:68–70Crossref, Medline, Google Scholar
67. Crimmins S, Langley S, Brownstein HH, Spunt BJ: Convicted women who have killed children: a self-psychology perspective. J Interpers Violence 1997; 12:49–69Crossref, Google Scholar
68. Crittenden P, Craig S: Developmental trends in nature of child homicide. J Interpers Violence 1990; 5:202–216Crossref, Google Scholar
69. Cummings P, Theis MK, Mueller BA, Rivara FP: Infant injury death in Washington State, 1981 through 1990. Arch Pediatr Adolesc Med 1994; 148:1021–1026Crossref, Medline, Google Scholar
70. DeSilva S, Oates RK: Child homicide: the extreme of child abuse. Med J Aust 1993; 158:300–301Crossref, Medline, Google Scholar
71. Dowdy ER, Unnithan NP: Child homicide and the economic stress hypothesis. Homicide Studies 1997; 1:281–290Crossref, Google Scholar
72. Emerick SJ, Foster LR, Campbell DT: Risk factors for traumatic infant death in Oregon, 1973 to 1982. Pediatrics 1986; 77:518–522Medline, Google Scholar
73. Farooque R, Ernst FA: Filicide: a review of eight years of clinical experience. J Natl Med Assoc 2003; 95:90–94Medline, Google Scholar
74. Goetting A: When parents kill their young children: Detroit 1982–1986. J Fam Violence 1988; 3:339–346Crossref, Google Scholar
75. Goetting A: Child victims of homicide: a portrait of their killers and the circumstances of their deaths. Violence Vict 1990; 5:287–295Crossref, Medline, Google Scholar
76. Goetting A: Patterns of homicide among women. J Interpers Violence 1988; 3:3–20Crossref, Google Scholar
77. Hargrave DR, Warner DP: Study of child homicide over two decades. Med Sci Law 1992; 32:247–250Crossref, Medline, Google Scholar
78. Hodgins S, Dube M: Parents who kill their children: a cohort study, in Lethal Violence: Proceedings of the 1995 Meeting of the Homicide Research Working Group. Edited by Riedel M, Boulahanis J. Washington DC, US Department of Justice, 1996, pp 141–144Google Scholar
79. Jason J, Gilliland JC, Tyler CW: Homicide as a cause of pediatric mortality in the United States. Pediatrics 1983; 72:191–197Medline, Google Scholar
80. Jason J, Carpenter MM, Tyler CW: Underrecording of infant homicide in the United States. Am J Public Health 1983; 73:195–197Crossref, Medline, Google Scholar
81. Jason J: Child homicide spectrum. Am J Dis Child 1983; 137:576–581Google Scholar
82. Kaspersson M: Homicide and infanticide in Stockholm 1920–1939. J Scandinavian Studies in Criminology and Crime Prevention 2002; 3:135–153Crossref, Google Scholar
83. Krugman ED: Fatal child abuse: analysis of 24 cases. Pediatrician 1985; 12:68–72Google Scholar
84. Kunz J, Bahr SJ: A profile of parental homicide against children. J Fam Violence 1996; 11:347–362Crossref, Google Scholar
85. Lucas DR, Wezner KC, Milner JS, McCanne TR, Harris IN, Monroe-Posey C, Nelson JP: Victim, perpetrator, family, and incident characteristics of infant and child homicide in the United States Air Force. Child Abuse Negl 2002; 26:167–186Crossref, Medline, Google Scholar
86. McClain PW, Sacks JJ, Froehlke RG, Ewigman BG: Estimates of fatal child abuse and neglect, United States, 1979 through 1988. Pediatrics 1993; 91:338–343Medline, Google Scholar
87. McCleary R, Chew KSY: Winter is the infanticide season. Homicide Studies 2002; 6:228–239Crossref, Google Scholar
88. McKee GR, Shea SJ: Maternal filicide: a cross-national comparison. J Clin Psychol 1998; 54:679–687Crossref, Medline, Google Scholar
89. Meadow R: Unnatural sudden infant death. Arch Dis Child 1999; 80:7–14Crossref, Medline, Google Scholar
90. Mulryan N, Gibbons P, O’Connor A: Infanticide and child murder—admissions to the Central Mental Hospital 1850–2000. Ir J Psychol Med 2002; 19:8–12Crossref, Medline, Google Scholar
91. Nersesian WS, Petit MR, Sharper R, Lemieux D, Naor E: Childhood death and poverty: a study of all childhood deaths in Maine. Pediatrics 1985; 75:41–50Medline, Google Scholar
92. Child protection, in Progress on ACS Reform Initiatives, Status Report 3. New York, New York City Administration for Children’s Services, 2001, pp 18–46Google Scholar
93. Overpeck MD, Brenner RA, Trumble AC, Trifiletti LB, Berendes HW: Risk factors for infant homicide in the United States. N Engl J Med 1998; 339:1211–1216Crossref, Medline, Google Scholar
94. Rodriguez SF, Smithey M: Infant and adult homicide. Homicide Studies 1999; 3:170–184Crossref, Google Scholar
95. Schloesser P, Pierpont J, Poertner J: Active surveillance of child abuse fatalities. Child Abuse Negl 1992; 16:3–10Crossref, Medline, Google Scholar
96. Schmidt P: Child homicide in Cologne. Forensic Sci Int 1996; 79:131–144Crossref, Medline, Google Scholar
97. Siegel CD, Graves P, Maloney K, Norris JM, Calonge BN, Lezotte D: Mortality from intentional and unintentional injury among infants. Arch Pediatr Adolesc Med 1996; 150:1077–1083Crossref, Medline, Google Scholar
98. Smithey M: Infant homicide: victim/offender relationship and causes of death. J Fam Violence. 1998; 13:285–298Google Scholar
99. Winpisinger KA, Hopkins RS, Indian RW, Hostetler JR: Risk factors for child homicide in Ohio. Am J Public Health 1991; 81:1052–1054Crossref, Medline, Google Scholar
100. Marks MN: Infanticide in Britain, in Infanticide: Psychosocial and Legal Perspectives on Mothers who Kill. Edited by Spinelli MG. Washington, DC, American Psychiatric Publishing, 2003, pp 185–197Google Scholar
101. Hatters Friedman S, Hrouda D, Holden CE, Noffsinger SG, Resnick PJ: Child murder committed by severely mentally ill mothers: an examination of mothers found not guilty by reason of insanity. J Forensic Sci (in press)Google Scholar
102. Jennings KD, Ross S, Popper S, Elmore M: Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord 1999; 54:21–28Crossref, Medline, Google Scholar
103. Chandra PS, Venkatasubramanian G, Thomas T: Infanticidal ideas and infanticidal behavior in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis 2002; 190:457–461Crossref, Medline, Google Scholar
104. Mowbray CT, Oyserman D, Bybee D, MacFarlane P, Rueda-Riedle A: Life circumstances of mothers with serious mental illnesses. Psychiatr Rehabil J 2001; 25:114–123Crossref, Medline, Google Scholar
105. Levitzky S, Cooper R: Infant colic syndrome: maternal fantasies of aggression and infanticide. Clin Pediatr 2000; 39:395–400Crossref, Medline, Google Scholar
106. Marzuk P, Tardiff K, Hirsch CS: Epidemiology of murder-suicide. JAMA 1992; 267:3179–3183Crossref, Medline, Google Scholar
107. National Center for Injury Prevention and Control: National Violent Death Reporting System. http://www.cdc.gov/ncipc/profiles/nvdrs/default.htmGoogle Scholar
108. Langstaff J, Sleeper T: The National Center on Child Fatality Review: OJJDP Fact Sheet, April 2001. Washington, DC, US Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention, 2001. http://www.ncjrs. org/pdffiles1/ojjdp/fs200112.pdfGoogle Scholar
109. Centers for Disease Control Reproductive Health Information Source: Surveillance and Research: Pregnancy Risk Assessment Monitoring System. http://www.cdc.gov/reproductivehealth/srv_prams.htmGoogle Scholar
110. Lehmann C: Government plans strategy to prevent child abuse. Psychiatr News, May 21, 2004, p 18Google Scholar
111. Carmona RH: Stopping the Heartbreaking Cycle of Child Maltreatment: Improving Prevention and Protection. Washington, DC, US Department of Health and Human Services, April 2004. http://www.surgeongeneral.gov/news/speeches/childmaltreat04012004.htmGoogle Scholar



