Pervasive Developmental Disorders in Preschool Children: Confirmation of High Prevalence
Abstract
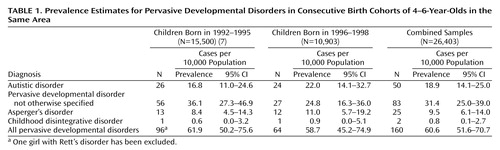
OBJECTIVE: The rate of reported pervasive developmental disorders has increased, and the authors found a rate of 62.6 per 10,000 in a previous study of preschoolers in Stafford, U.K. They conducted another survey in 2002 to estimate the prevalence in children in a later birth cohort and to compare it to previous findings from the same area. METHOD: Screening for developmental problems included 10,903 children ages 4.0 to 6.0 years who were living in a Midlands town on the survey date. Children with symptoms suggestive of pervasive developmental disorders were intensively assessed by a multidisciplinary team using standardized diagnostic interviews, psychometric tests, and medical workups. RESULTS: Sixty-four children (85.9% boys) were diagnosed with pervasive developmental disorders. The prevalence was 58.7 per 10,000, with a 95% confidence interval (CI) of 45.2–74.9, for all pervasive developmental disorders, 22.0 per 10,000 (95% CI=14.1–32.7) for autistic disorder, and 36.7 per 10,000 (95% CI=26.2–49.9) for other variants. These rates were not significantly different from the previous rates. The mean age at diagnosis was 37.8 months, and 53.1% of the children were originally referred by health visitors. Of the 64 children with pervasive developmental disorders, 29.8% had mental retardation, but this rate varied by disorder subtype. Few children had associated medical conditions. CONCLUSIONS: The rate of pervasive developmental disorders is higher than reported 15 years ago. The rate in this study is comparable to that in previous birth cohorts from the same area and surveyed with the same methods, suggesting a stable incidence.
Pervasive developmental disorders are characterized by marked impairments in reciprocal social interaction, language, and communication and by the presence of repetitive/stereotypic patterns of behavior and interests (DSM-IV). The exact causes of pervasive developmental disorders are yet unknown, although genetic factors play a strong role (1). There is no cure for autism, but research on the efficacy of early, intensive behavioral interventions suggests that developmental trajectories can be positively altered, particularly with respect to language and cognitive development. Expert committees recommend at least 25 hours/week of educational programming for preschool children with pervasive developmental disorders (2). The total societal costs incurred by these interventions are high (3) and influenced by the prevalence of pervasive developmental disorders in preschoolers.
In the last 15 years, epidemiological surveys of pervasive developmental disorders have shown increasing prevalence estimates that reflect a broadening of the concept and diagnostic criteria for autism as well as increased awareness and improved detection of pervasive developmental disorders at all ages and all levels of intellectual ability (4). Whether or not a secular increase in the incidence of pervasive developmental disorders also contributes to the higher prevalence figures cannot be adequately answered from the existing data (4, 5). A conservative estimate for the prevalence of all pervasive developmental disorders is around 30 per 10,000 (5, 6). However, more recent surveys characterized by case-finding methods focusing on the whole spectrum of pervasive developmental disorders (as opposed to autistic disorder), by sampling of young age groups, by proactive and repeated screening, and by up-to-date standardized diagnostic instruments have yielded rates around 60 per 10,000 (1, 4). One of the first of these surveys was our study in Stafford (Midlands, U.K.) that yielded a rate of 62.6 per 10,000 children (with a 95% confidence interval [CI] of 50.8–76.3) in the population (N=15,500) of children born in the years 1992–1995 (7). As these results occurred in a context of public concerns about the putative etiologic role of environmental factors, such as immunizations, which could drive up the rates of pervasive developmental disorders, it was critical to follow up these initial findings in cohorts of children born in subsequent years. We therefore set out to study the prevalence of pervasive developmental disorders in the same area and with the same methods among a more recent birth cohort.
The specific aims of this study were 1) to repeat the survey in the same area while holding constant the design features of our investigation in order to examine if our previous findings could be replicated and 2) to test whether the rate of pervasive developmental disorders was higher in these younger children, which would suggest a real increase in the incidence of the disorder.
Method
Site and Target Population
The study was conducted at the Child Development Centres in Stafford and Cannock in the Midlands (England). The target population was all children born from Jan. 1, 1996, to Dec. 31, 1998 (N=10,903) and living within the target area on April 1, 2002. This area is covered by one National Health Service Trust. Clinical and research data were collected on eligible children from January 1999 to July 2003.
Case Identification and Definition
As in our previous study, children with pervasive developmental disorders were identified in four different stages, shown in Figure 1.
Stage 1
The national framework of child health surveillance in the United Kingdom, which recommends screening of all children at birth, at 6 weeks, between 6 and 9 months, at 18–24 months, and at 3–3 years, was used to identify children with actual or potential developmental problems needing further evaluation. Apart from the screenings at birth and at 6 weeks, which were both done by doctors and concentrated mainly on identifying medical problems in the newborn and during the neonatal period, the screening at subsequent ages was done by “health visitors,” who, in the United Kingdom, are nurses with general and midwifery training followed by specialist children’s training and usually wide experience of working with families with young children.
The health visitor screenings at 6–9 months, 18–24 months, and 3–3 years concentrated mainly on identifying developmental, sensory (specifically hearing), and behavior or adjustment problems in children as well as providing health education, advice for healthy living, and accident prevention for children and families. Apart from these scheduled screenings, the health visitor often had more ongoing contact with families who had more than one young child and with families in which an earlier problem or potential problem had been identified, e.g., mothers with postnatal depression, families lacking adequate social support, or children who were born prematurely or had a medical problem. The health visitor was also available to listen to and advise about any specific worries or concerns parents had about their child outside the scheduled program of contacts, especially during the nationally recommended preschool immunization sessions when the children were 2, 3, 4, and 13 months and 3 years old.
Besides the health visitors, two other groups of professionals, speech and language therapists and pediatricians, constituted the main referrers of children for further evaluation. The referrers underwent training sessions on early identification of specific and pervasive developmental problems and received written guidelines for referral of children. The guidance for these initial referrals was left purposefully general to provide maximum sensitivity for finding cases of pervasive developmental disorders.
The criterion for initial referral of a preschool child was moderate to severe impairment in one area of development or mild to moderate impairment in two or more areas. The areas of development comprised motor development, speech and language development, socialization and play, behavior, vision, and hearing. The referrers were also advised to refer any child about whom either parents or professionals had concern, even if the concern could not be described in more specific developmental terms. Referrals were sought as soon as any problem was identified, usually by age 2 years. Over 90% of the child population participated in the surveillance; children with pervasive developmental disorders not participating in screening could be identified by other routes (speech therapists, etc.). A total of 659 children were referred at stage 1 during the study period.
Stage 2
Children referred at this initial stage underwent a second screen carried out by a developmental pediatrician (S.C.) or by a child development team, consisting of a pediatrician, a specialist health visitor, a speech and language therapist, and physical, occupational, and play therapists. The parents or main caretakers of the children were involved in each stage of the screening. Any urgent referral was forwarded to the developmental pediatrician or a multidisciplinary team on a fast-track basis. Of the 659 children initially referred, 342 passed this second screen satisfactorily and had only mild problems. They received appropriate services, and at follow-up 319 children were discharged with no further concern. However, the progress of 23 children was deemed unsatisfactory at follow-up, and they entered stage 3 for further assessment alongside the remaining 317 children shown by the second screen to have moderate or severe problems.
Stage 3
The 340 children who entered stage 3 were selected for a 2-week assessment (10 daily sessions of 2 hours each) conducted by the multidisciplinary team. During this assessment, a play therapist led a group of four children with their participating parents; usually these were mothers but in some cases included both parents, with the fathers attending at least some sessions of structured activities as well as free play.
The groups were constituted so that the children were reasonably close in age to each other, mostly between the ages of 2 and 3 years; a few children were under 2 or over 4 years. During these play sessions, particular note was taken of the children’s general behavior, social skills, interaction with the peer group and with the adults, and language and communication in a more naturalistic setting than a formal individual assessment session. The children were also observed for their motor skills, attention, listening, distractibility, and biddability, and note was made of any unusual behavior, particularly sensory stimulation, repetitive behaviors, or motor stereotypies.
A developmental pediatrician took a detailed developmental history and conducted a comprehensive medical and neurodevelopmental examination. Children were assessed by a speech and language therapist, a pediatric physical therapist, an occupational therapist, a dietician, a dental nurse, and a nurse specialist trained in behavioral intervention for children with pervasive developmental disorders and other learning problems. Hearing was assessed by an audiological physician, and vision was screened by an orthoptist. At the end of this assessment, a clinical diagnostic formulation of the child’s problem was made by the lead pediatrician. Of the 340 children assessed, 83 had developmental problems suggestive of a diagnosis of pervasive developmental disorder and were therefore entered into the next stage to confirm that diagnosis.
Stage 4
Children strongly suspected of having pervasive developmental disorders were further assessed with standardized diagnostic measures (Autism Diagnostic Interview—Revised) and, if possible, psychometric assessments (Wechsler Preschool and Primary Scale of Intelligence or Merrill-Palmer Scale of Mental Tests). The Autism Diagnostic Interview—Revised is a semistructured diagnostic interview for use with caregivers of children who may have a pervasive developmental disorder (8–10). The Autism Diagnostic Interview was administered by the developmental pediatrician (S.C.), who has been trained in its use. The interview algorithm generates scores for the areas of social interaction, communication (verbal and nonverbal), repetitive behaviors, and age at first recognition of abnormalities, for which appropriate cutoff points are available. The algorithm is compatible with the DSM-IV diagnostic criteria for autistic disorder. Children diagnosed as having pervasive developmental disorder subsequently underwent a formal psychometric assessment. The Wechsler Preschool and Primary Scale of Intelligence (11) and the Merrill-Palmer Scale of Mental Tests (12) were used as psychometric tools for verbal and nonverbal children, respectively. Intellectual functioning was estimated according to performance on the full IQ measure of the Wechsler Preschool and Primary Scale of Intelligence, the quotient derived from the Merrill-Palmer Scale of Mental Tests, or in a few cases, the Griffiths Mental Development Scales (Test Agency, Oxford, U.K.). Mental retardation was defined according to conventional levels of severity based on IQ, i.e., mild, 50–69; moderate, 35–49; severe, 20–34; and profound, <20.
The final diagnostic determination was derived from a review of all existing data by the pediatrician, who knew all the children well. Diagnosis was made with the DSM-IV diagnostic criteria for pervasive developmental disorders, including autistic disorder, Asperger’s disorder, Rett’s disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified.
Comparison Data
Data from this new survey were compared to those obtained in the survey we conducted in the same area among children born from 1992 to 1995. In brief, in the earlier study we identified 97 children with pervasive developmental disorders, including one girl with Rett’s syndrome, who has been excluded in the comparisons of the previous and current studies because no cases of Rett’s syndrome were identified in the current study. We used data about prevalence and diagnostic subtypes, age at diagnosis, age, and source of referral to test for systematic differences between the two surveys. Full details about the original survey can be found elsewhere (7).
Reliability Study
In our previous study, a subset of 38 videotaped interviews obtained with the Autism Diagnostic Interview were selected at random and blindly rated by three trained raters (including E.F.). The interrater reliability for domain scores as measured by the intraclass correlation coefficient was 0.82 for social interaction, 0.87 for nonverbal communication, 0.85 for verbal communication (based on a subset of 28 children with sufficient language level), 0.59 for repetitive behaviors, and 0.86 for the total Autism Diagnostic Interview score. Agreement on the proportion of subjects scoring higher than each of the predetermined cutoffs was high for all domains. Blinded raters were also asked to provide an independent global judgment about the presence or absence of a pervasive developmental disorder based on the parental interview, and they confirmed the presence of pervasive developmental disorders in all 38 children, yielding a 100% agreement with the original pediatrician’s diagnosis (7).
Biological Investigations
All children with a possible diagnosis of pervasive developmental disorder underwent biological investigations according to a previously established standard protocol. This included a full blood count; plasma chemistry; serum levels of calcium, thyrotropin, thyroxine, and creatine kinase; plasma and urine levels of amino acids and organic acids; chromosome karyotyping; and electroencephalogram. The skin of children with suggestive birth marks was examined with ultraviolet light to detect markers of tuberous sclerosis.
Statistical Analyses
Conventional statistical tests were performed for categorical and continuous variables. When assumptions for parametric tests were not met, we performed nonparametric analyses, i.e., Kruskal-Wallis analyses of variance (ANOVAs) and Mann-Whitney tests. Throughout, a conventional p value of 0.05 was retained as the level of statistical significance. For prevalence estimates, asymptotic 95% CIs were calculated. Comparisons of prevalence rates in the two surveys were performed by calculating rate ratios and their associated 95% CIs. Statistically significant differences in prevalence rates were thus identified when the value 1 was not included in the 95% CI of the ratio.
Results
Prevalence
The details of the case-finding procedure are summarized in Figure 1. A total of 83 children entered stage 4 with a suspicion of a pervasive developmental disorder. Follow-up medical and developmental examinations indicated that a diagnosis of pervasive developmental disorder was very unlikely in 17 children, and no Autism Diagnostic Interview was sought for them. Of the 66 remaining children, Autism Diagnostic Interviews could be obtained from 57 parents (86.4%), and a pervasive developmental disorder diagnosis was confirmed in 55 of these children. For the other nine children, we obtained detailed follow-up developmental and diagnostic assessments that all confirmed the presence of a pervasive developmental disorder. Overall, a diagnosis of a pervasive developmental disorder was thus confirmed in 64 children, yielding a combined prevalence of pervasive developmental disorder of 58.7 per 10,000 (95% CI=45.2–74.9). The prevalence estimates for the diagnostic subtypes are shown in Table 1. The overall prevalence for pervasive developmental disorders other than autistic disorder was 36.7 per 10,000 (95% CI=26.2–49.9). No child with Rett’s disorder was identified. Table 1 provides the results for both this survey and our previous survey. Comparisons of prevalence rates were performed for the two surveys. There were no statistical differences in the five estimates between the two samples. The prevalence rate ratios were 1.31 (95% CI=0.75–2.28) for autistic disorder, 0.69 (95% CI=0.43–1.08) for pervasive developmental disorder not otherwise specified, 1.31 (95% CI=0.60–2.87) for Asperger’s disorder, 1.42 (95% CI=0.04–55.40) for childhood disintegrative disorder, and 0.95 (95% CI=0.69–1.30) for all pervasive developmental disorders. As no statistically significant difference could be detected, we pooled the two samples together (Table 1) in order to provide more robust and precise prevalence estimates. The prevalence of all pervasive developmental disorders, excluding Rett’s disorder, for the combined samples was 60.6 per 10,000 (95% CI=51.6–70.7).
Autism Diagnostic Interview Scores
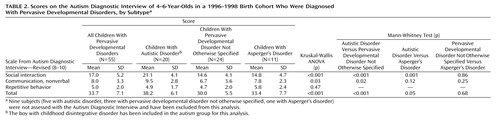
Table 2 displays the scores on the Autism Diagnostic Interview obtained during the stage 4 standardized assessments. The mean age at which the Autism Diagnostic Interview was conducted was 59.5 months (SD=13.8). Consistent with those in our previous study, the total scores and the social interaction scores were significantly higher in the autistic disorder group than in either the group with Asperger’s disorder or the group with pervasive developmental disorder not otherwise specified. The communication scores (based on the nonverbal domain) were also indicative of worse impairments in the autistic disorder group than in the group with pervasive developmental disorder not otherwise specified, and there was a similar but nonsignificant difference from the Asperger’s disorder group. By contrast, there were no differences for repetitive behavior scores across the three diagnostic subtypes. The groups with Asperger’s disorder and pervasive developmental disorder not otherwise specified were remarkably similar for all Autism Diagnostic Interview scores.
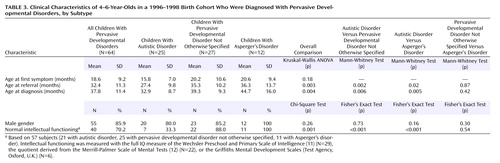
Clinical Characteristics
On average, the first symptoms to arouse parental concerns occurred at 18.6 months of age, with few differences between diagnostic subtypes (Table 3). However, the mean age at referral was 32.4 months, i.e., 14 months on average after the occurrence of the first symptoms. For both age at referral and age at diagnosis, the autistic group had lower ages by at least 6 months than the other two groups. The difference was highly significant for pervasive developmental disorder not otherwise specified and of borderline significance for the Asperger’s disorder group because of its much smaller size.
A typical male preponderance was found for all diagnostic subtypes and was even more marked for the Asperger’s disorder group. Intellectual functioning could be estimated in 57 subjects (Wechsler Preschool and Primary Scale of Intelligence, N=29; Merrill-Palmer Scale of Mental Tests, N=22; Griffiths Mental Development Scales, N=6). Significant differences emerged between the three groups. The rate of mental retardation in the autistic disorder group was 66.7%, compared to 12.0% in the group with pervasive developmental disorder not otherwise specified and 0.0% in the Asperger"s disorder group. In the group with pervasive developmental disorder not otherwise specified, all three subjects with intellectual delays scored in the mild mental retardation range. In the autistic disorder group, six subjects (28.6%) had mild mental retardation and eight subjects (38.1%) had moderate to severe mental retardation.
The prenatal and birth histories of most children were unremarkable. The mean gestational age was 39.0 weeks (range=27–42), and seven children (10.9%, all boys) were born before week 38; these included one child born at week 27 and one child born at week 28. The mean birth weight of the 64 children was 3,370 g (SD=664), and four children (6.3%, all boys) had a birth weight less than 2,500 g; these four included two children (3.1%) with birth weights below 1,000 g. Two children (one boy, one girl) suffered from seizures. There was no instance of fragile X disorder, tuberous sclerosis, congenital rubella, or fetal alcohol syndrome in the sample.
Referral Pathways
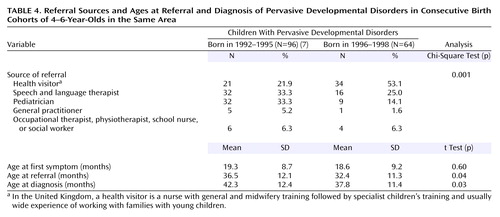
We were interested in assessing differences between the two samples in key referral characteristics (Table 4). A significant difference was found for the distribution of referral sources in the two surveys (χ2=19.2, df=3, p<0.001). Of the 64 children with diagnoses of pervasive developmental disorders in the present study, over one-half were referred by health visitors, compared to only 21.9% in the previous study. The increase in the proportion of children referred by health visitors went hand in hand with a corresponding reduction of referrals from pediatricians and general practitioners and a smaller reduction of referrals from speech therapists. However, as in the previous study, a closer look at the pathway of referrals showed that most of the initial referrals to pediatricians and speech therapists had been in fact initiated by health visitors. When we included the proportions for these two groups, we calculated that 85.9% (N=55) of the 64 children with eventual diagnoses of pervasive developmental disorders were first identified by health visitors as having problems needing further evaluation.
As expected, there was no difference between the two samples for the mean age at which parents first became concerned. However, when age at referral and age at diagnosis were compared in the two samples, there were significant decreases in the most recent survey of 4.1 and 4.5 months, respectively, suggesting that the efficiency of detection of pervasive developmental disorders in our community had improved over time. We then computed the difference between the age at referral and both the age at diagnosis and the age at first symptom. No difference was found between the average delays from referral to diagnosis for the 1992–1995 and 1996–1998 samples, which were closely comparable (5.8 months versus 5.5 months) (t=0.27, df=158, n.s.). By contrast, a difference was found for the average delay from the first symptom to referral between the two surveys (17.2 months versus 13.8 months) (t=1.72, df=158, p=0.09), although this suggestion of faster response of the clinical service fell short of statistical significance. Nevertheless, this gain illustrates the improvement over time that we achieved in early identification of pervasive developmental disorders in our community in the study interval.
Discussion
Consistent with research (7, 13–16) and review (4) data, the prevalence for all pervasive developmental disorders was near 60 per 10,000. Pervasive developmental disorder not otherwise specified was the most frequent subtype, and it occurred at about 1.7 times the rate of autistic disorder in the combined samples from the two surveys. Consistent with the findings in many other studies (17), Asperger’s disorder was less frequent than the two other subtypes. Similarly, as found in other surveys (18), childhood disintegrative disorder was extremely rare. In light of the consistency of estimates obtained in independent studies, an overall prevalence figure of 0.6% should now be retained as the best estimate for the spectrum of autistic disorders. It should be remembered that the concept of pervasive developmental disorders and of a spectrum of autistic disorders is relatively new. Previous epidemiological investigations mostly concentrated on autistic disorder, often on a much narrower definition of autistic disorder than that currently employed. In prior surveys, a relatively high number of children described with different labels (i.e., atypical autism, autistic features, etc.) (4) did not meet the full criteria for autism and were usually not incorporated in prevalence calculations. Therefore, a direct comparison of current rates of pervasive developmental disorders with prevalence estimates from past surveys should not be performed, as they relate to different case definitions. However, one of the few studies conducted more than 30 years ago that yielded useful information for such a comparison is that by Wing and Gould (19) in the United Kingdom, who identified a group of children encompassing more than just those with classical autism and referred to as exhibiting a “triad of impairments.” The prevalence of this broader disorder was 20 per 10,000, and if we take the data from that study as a baseline, recent prevalence figures point therefore toward a threefold increase in the prevalence of pervasive developmental disorders (5). Nevertheless, one must remain aware that the “triad of impairments” described by Wing and Gould tapped into more severe clinical presentations than the current conceptualizations of pervasive developmental disorders, especially as autism (and Asperger’s disorder) were usually underrecognized at that time among children with normal intelligence. It could well be that the threefold increase is entirely accounted for by this shift in diagnostic concepts and criteria, although no direct verification of this hypothesis can be obtained.
One of the goals of this repeat survey was to apply rigorously the same methods to identify in the same population children with pervasive developmental disorders born in consecutive birth cohorts. If the prevalence figure for our new sample had increased from that in the previous study, that might have pointed toward an increase in the incidence of pervasive developmental disorders, consistent with the various claims of an “epidemic of autism” (4, 5). We did not find such an increase, and there was no statistical difference between the two prevalence rates, not even a trend in that direction. It can therefore be safely concluded that, in this area and for children born over the period 1992 through 1998, there was no evidence of a secular change in the incidence of pervasive developmental disorders. In investigations where upward trends in prevalence rates were observed, changes over time in diagnostic criteria and detection of autism could not be ruled out as explanatory factors. When these factors were specifically investigated, evidence was found in some studies that changes in diagnostic practices have occurred over time, with diagnostic switching between autism and diagnostic categories such as mental retardation (20) and language disorders (21). Similarly, period and cohort effects that correspond to changes in the organization and accessibility of services in various countries have been identified and appear to account for some of the rise in the rates of diagnoses of pervasive developmental disorders (16, 22).
There were some nonsignificant differences in the rates of different subtypes of pervasive developmental disorders; the rates of autism and Asperger’s disorder went up slightly at the expense of the rate for pervasive developmental disorder not otherwise specified. However, the meaning of these trends is unclear. As shown in our previous study (7) and others (6, 13, 14), the differentiation between subtypes of pervasive developmental disorders along the autistic spectrum is much less reliable than the judgment about the presence or absence of a pervasive developmental disorder, particularly in this young age group. On the basis of the results of our standardized assessments, no difference was found in symptom scores and severity between pervasive developmental disorder not otherwise specified and Asperger’s disorder. As a consequence, the possibility of generating separate algorithms or cutoffs with instruments such as the Autism Diagnostic Interview in order to differentiate between different subtypes of pervasive developmental disorders appears to be remote. Rather than signaling a technical difficulty with our instrumentation, this limitation is consistent with the growing tendency to dimensionalize the autism phenotype.
The lower mean ages at referral and diagnosis in this sample than in the earlier one were a source of satisfaction. Most certainly, this is a result of an increasing awareness about developmental deviance and autism in general and of our own efforts to train first-line professionals in the early detection of developmental problems in young children. The evidence that has accumulated in the last 10 years showing the efficacy of early, intensive behavioral and educational programs supports earlier detection and treatment of pervasive developmental disorders (2, 23). However, there was a relatively long delay between the first symptom and referral, and this delay should be targeted in order to improve early detection. It is nevertheless worth noting that both the age at first symptom and age at referral had substantial variance and that, for sizable proportions of the subjects, symptom recognition and referral occurred well after the second birthday. Previous studies on the age at the first symptom to arouse parental concerns have shown similar distributional characteristics (24). Recognition of this spread has important implications for screening efficiency in populations of preschoolers, and detection efforts should be repeated over a developmental period rather than at one point in time. Efforts to screen at 18 months of age have been met with poor sensitivity (14), probably because the emergence of developmental autistic deviance is a gradual process that stretches over a long interval, from birth to the third birthday. In our opinion, research on screening for autism should lose its predominant focus on the psychometric properties of a screening tool administered at one age or another (e.g., Checklist for Autism in Toddlers, Modified Checklist for Autism in Toddlers) and, rather, concentrate on evaluating the performance of population screening programs that would involve the repeated administration of ad hoc screening instruments at several time points during the preschool period.
There were two main reasons for the increase in health visitor referrals since the last study. The first reason was simply an administrative change whereby the 18–24-month preschool surveillance, instead of being carried out by a doctor, was delegated to the health visitor from the latter part of the first study onward. Along with this change in personnel, timing of the assessment was also changed from 18 months to 24 months. Not surprisingly, the bulk of the referrals for the stage 2 assessments were generated from the 18–24-month surveillance examinations, hence by health visitors. The other possible contributory reason was that as health visitors became more confident in their assessment and had easier access to the multidisciplinary group, they shifted toward referring children directly to this group, without going through the surrogate route of having their concerns validated by another group of professionals, namely pediatricians or speech therapists. We have therefore shown in our study that specifically in the United Kingdom, there is a way of consistently and comprehensively identifying young children with pervasive developmental disorders by using the resources of an important group of primary care workers for children and families, i.e., the “health visitors,” in the context of the national program of preschool surveillance of all children. In our study, 85.9% of the children who were eventually diagnosed with pervasive developmental disorders were initially identified by the health visitors as needing further screening and assessment and were referred either to speech and language therapists, pediatricians, and general practitioners or directly to the multidisciplinary developmental team. It is the systematic screening of these children in close consultation with the parents by a multidisciplinary group of professionals with expertise in pervasive developmental disorders and other complex developmental disorders of young children that resulted in the comprehensiveness of case identification in our study.
One of the important attendant benefits of this particular strategy for case identification is that it may also identify children with other early developmental difficulties, such as specific language impairments, and children with learning problems (e.g., mental handicap), early externalizing behavior, developmental coordination disorder, suboptimal or dysfunctional care at home, etc., whose need for and benefit from early intervention may be as great as that for children with pervasive developmental disorders. Whether this strategy will work in other countries without a similar group of primary care workers for young children, such as the health visitors in the United Kingdom, remains to be established.
 |
 |
 |
 |
Received Jan. 19, 2004; revision received June 23, 2004; accepted July 8, 2004. From the Child Development Centre, Central Clinic, Stafford, U.K.; and the Department of Psychiatry, McGill University, Montreal, and the Department of Psychiatry, Montreal Children’s Hospital. Address reprint requests and correspondence to Dr. Fombonne, Department of Psychiatry, Montreal Children’s Hospital, 4018 Ste-Catherine West, Montreal, QC H3Z 1P2, Canada; [email protected] (e-mail). Funded by the First Community Health Trust and subsequently by the South Staffs Healthcare National Health Service Trust. The authors thank the parents and the children in the research group for their cooperation; the staff of the Child Development Centres; the clinicians who referred the children, especially the health visitors and speech and language therapists; Linyan Meng for her contribution to data analysis; and Mrs. Sally Williams and Mrs. Penny Hickling for the psychometric assessment of the children.
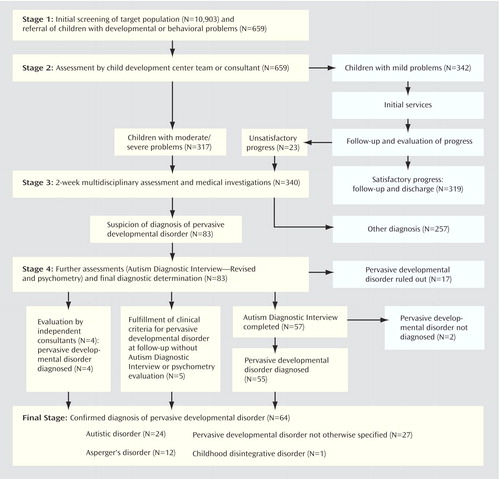
Figure 1. Process for Identifying Cases of Pervasive Developmental Disorders Among 4–6-Year-Olds in a 1996–1998 Birth Cohort
1. Volkmar FR, Lord C, Bailey A, Schultz RT, Klin A: Autism and pervasive developmental disorders. J Child Psychol Psychiatry 2004; 45:135–170Crossref, Medline, Google Scholar
2. National Research Council: Educating Children With Autism. Washington, DC, National Academy Press, 2001Google Scholar
3. Jarbrink K, Knapp M: The economic impact of autism in Britain. Autism 2001; 5:7–22Crossref, Medline, Google Scholar
4. Fombonne E: Epidemiological surveys of autism and other pervasive developmental disorders: an update. J Autism Dev Disord 2003; 33:365–382Crossref, Medline, Google Scholar
5. Fombonne E: The prevalence of autism. JAMA 2003; 289:1–3Crossref, Google Scholar
6. Yeargin-Allsopp M, Rice C, Karapurkar T, Doernberg N, Boyle C, Murphy C: Prevalence of autism in a US metropolitan area. JAMA 2003; 289:49–55Crossref, Medline, Google Scholar
7. Chakrabarti S, Fombonne E: Pervasive developmental disorders in preschool children. JAMA 2001; 285:3093–3099Crossref, Medline, Google Scholar
8. Le Couteur A, Rutter M, Lord C, Rios P, Robertson S, Holdgrafer M, McLennan J: Autism Diagnostic Interview: a standardized investigator-based instrument. J Autism Dev Disord 1989; 19:363–387Crossref, Medline, Google Scholar
9. Lord C, Rutter M, Le Couteur A: Autism Diagnostic Interview—Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 1994; 24:659–685Crossref, Medline, Google Scholar
10. Fombonne E: Diagnostic assessment in a sample of autistic and developmentally impaired adolescents. J Autism Dev Disord 1992; 22:563–581Crossref, Medline, Google Scholar
11. Wechsler D: Manual for Wechsler Preschool and Primary Scale of Intelligence—Revised (British amendments). Kent, UK, Psychological Corp, 1990Google Scholar
12. Stutsman R: Merrill-Palmer Scale of Mental Tests: Preprints of Part III, Mental Measurement of Preschool Children. Chicago, Stoelting, 1948Google Scholar
13. Bertrand J, Mars A, Boyle C, Bove F, Yeargin-Allsopp M, Decoufle P: Prevalence of autism in a United States population: the Brick Township, New Jersey, investigation. Pediatrics 2001; 108:1155–1161Crossref, Medline, Google Scholar
14. Baird G, Charman T, Baron-Cohen S, Cox A, Swettenham J, Wheelwright S, Drew A: A screening instrument for autism at 18 months of age: a 6-year follow-up study. J Am Acad Child Adolesc Psychiatry 2000; 39:694–702Crossref, Medline, Google Scholar
15. Scott FJ, Baron-Cohen S, Bolton P, Brayne C: Brief report: prevalence of autism spectrum conditions in children aged 5–11 years in Cambridgeshire, UK. Autism 2002; 6:231–237Crossref, Medline, Google Scholar
16. Gurney JG, Fritz MS, Ness KK, Sievers P, Newschaffer CJ, Shapiro EG: Analysis of prevalence trends of autism spectrum disorder in Minnesota. Arch Pediatr Adolesc Med 2003; 157:622–627Crossref, Medline, Google Scholar
17. Fombonne E, Tidmarsh L: Epidemiologic data on Asperger disorder. Child Adolesc Psychiatr Clin North Am 2003; 12:15–21, v-viCrossref, Medline, Google Scholar
18. Fombonne E: Prevalence of childhood disintegrative disorder. Autism 2002; 6:149–157Crossref, Medline, Google Scholar
19. Wing L, Gould J: Severe impairments of social interaction and associated abnormalities in children: epidemiology and classification. J Autism Dev Disord 1979; 9:11–29Crossref, Medline, Google Scholar
20. Croen LA, Grether JK, Hoogstrate J, Selvin S: The changing prevalence of autism in California. J Autism Dev Disord 2002; 32:207–215Crossref, Medline, Google Scholar
21. Jick H, Kaye JA, Black C: Epidemiology and possible causes of autism: changes in risk of autism in the UK for birth cohorts 1990–1998. Pharmacotherapy 2003; 23:1524–1530Crossref, Medline, Google Scholar
22. Lingam R, Simmons A, Andrews N, Miller E, Stowe J, Taylor B: Prevalence of autism and parentally reported triggers in a north east London population. Arch Dis Child 2003; 88:666–670Crossref, Medline, Google Scholar
23. Rogers S: Empirically supported comprehensive treatments for young children with autism. J Clin Child Psychol 1998; 27:168–179Crossref, Medline, Google Scholar
24. De Giacomo A, Fombonne E: Parental recognition of developmental abnormalities in autism. Eur Child Adolesc Psychiatry 1998; 7:131–136Crossref, Medline, Google Scholar



