In This Issue
Predicting Alzheimer’s Disease
Some elderly people have memory problems beyond those expected for their age. Is this mild cognitive impairment a harbinger of Alzheimer’s disease? The answer could lead to early drug therapy of mild Alzheimer’s disease and slow its progression. Modrego et al. (p. 667) measured several chemical compounds in the brains of patients with mild cognitive impairment, using magnetic resonance spectroscopy. After 3 years, 29 of the 53 patients had developed probable Alzheimer’s disease. The only baseline value that predicted this conversion was the ratio of N-acetylaspartate to creatine in the left occipital lobe. The demented patients’ average ratio was 1.46, whereas for nondemented patients it was 1.64. If confirmed in larger studies, this finding would provide an objective tool for predicting conversion of mild cognitive impairment to probable Alzheimer’s disease.
Wider Antidepressant Use by the Elderly
With the development of newer medications, use of antidepressants began to increase in the late 1980s. That coincided with the start of a long-term study of 4,162 elderly community residents in North Carolina. Blazer et al. (p. 705) report characteristics in 1986/1987 that predicted use of antidepressants 3 years later, in 1989/1990, and features in 1992/1993 that were associated with antidepressant use in 1996/1997. The relationships for the two intervals showed some similarities and some differences. Negative affect and previous antidepressant use predicted current use in both intervals. Somatic problems were a stronger predictor in the first interval than in the second, whereas chronic illness, cognitive dysfunction, and low positive affect were stronger factors in the second interval. Over the study period, antidepressant use rose from 4.5% of respondents to 8.1%, but the rates were lower for blacks than for whites, and this discrepancy grew over time.
Crossover of Eating Disorders
Many patients with anorexia nervosa or bulimia nervosa eventually develop the other eating disorder. To help identify who is likely to switch disorders, Tozzi et al. (p. 732) assessed 88 girls or women with anorexia nervosa, restricting subtype, and 350 with bulimia nervosa, purging subtype. Of those with anorexia nervosa, 36% developed bulimia nervosa over 15 years. Of those with bulimia nervosa, 27% developed anorexia nervosa. The crossover usually occurred within the first 5 years. For subjects who switched from anorexia nervosa to bulimia, perceived parental criticism was a salient predictor. Crossover from bulimia to anorexia nervosa was linked to less novelty seeking and less alcohol abuse/dependence. Both types were associated with a low level of self-directedness. Providing a treatment that bolsters self-directedness and family communication, therefore, may stabilize the diagnosis as well as address core psychological issues.
Affective Psychosis: Another Neurodevelopmental Disorder?
Schizophrenia has been dubbed a neurodevelopmental disorder, and many patients and their relatives have brain, neurological, and neuropsychological disturbances. Schizophrenia shows some genetic connection to affective psychosis, and patients with affective psychosis also have neurological abnormalities and neuropsychological impairment. To determine whether these deficits are associated with risk for the disorder, Schubert and McNeil (p. 758) examined young adult offspring of mothers with schizophrenia, mothers with affective psychosis, and healthy mothers. There was only one neuropsychological test on which both groups of high-risk offspring differed from the normal-risk offspring. Also, the affective-risk group was less likely than the schizophrenia-risk group to score above the normal subjects’ 90th percentile on multiple tests, and their level of neurological abnormalities was similar to that of the normal-risk offspring. These findings suggest that schizophrenia and affective psychosis belong to different biological categories.
Psychosis Goes to Prison
Are the high rates of psychosis found among prisoners real, or do they reflect prisoner drug abuse or unrepresentative surveys? They are real, according to Brugha et al. (p. 774). National samples totaling 13,250 adults in British households and prisons were screened for psychosis, and a diagnostic interview was administered to those with positive results. The prevalence of psychosis was more than 10 times higher among the prisoners than among the community subjects, 52 per 1,000 versus 4.5 per 1,000. The difference could not be explained by the prisoners’ lower socioeconomic status or age and was minimally related to alcohol and drugs. Psychotic symptoms were similar in the two groups, and the rates of antipsychotic medication in the community and in male prisoners were the same (34%). Fewer prisoners had seen primary care physicians about mental health problems during the previous year, however, suggesting a need for greater recognition and treatment for these prisoners.

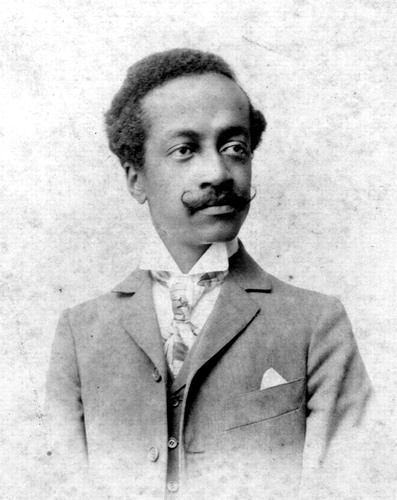
Images in Psychiatry
Juliano Moreira (1873–1933) (p. 666)