Psychosis in the Community and in Prisons: A Report From the British National Survey of Psychiatric Morbidity
Abstract
OBJECTIVE: Reports of increased rates of psychosis in prisons could be due to sampling and ascertainment differences. The authors compared two samples of subjects 16–64 years of age: those from the general population of residents in Great Britain and prisoners in England and Wales. METHOD: A random sample of remanded and sentenced male and female prisoners (N=3,142) and a two-phase, cross-sectional random sample of household residents (N=10,108) were assessed with structured questionnaires and the semistructured Schedules for Clinical Assessment in Neuropsychiatry. RESULTS: The weighted prevalence of probable functional psychosis in the past year was 4.5 per thousand (95% CI=3.1 to 5.8) in the household survey. In the prison survey, the weighted prevalence was over 10 times greater: 52 per thousand (95% CI=45 to 60). One in four prisoners with a psychotic disorder had psychotic symptoms attributed to toxic or withdrawal effects of psychoactive substances. The proportion of subjects with specific types of hallucinations or delusions did not differ between prison and household psychosis cases. CONCLUSIONS: This large study using standardized comparisons showed that the prevalence of psychosis in prisons is substantially higher than in the community and is deserving of greater attention to treatment and prevention. Apart from a minority of prisoners with symptoms attributable to psychoactive substances, the clinical symptom profile of psychosis is the same in both settings. Longitudinal research is needed to better understand these prevalence differences.
In many different countries, severe mental disorders have been reported to occur 5–10 times more frequently among people in prison than in the general population (1, 2). However, it is unclear whether the high rates of psychotic mental disorders in prison are real or artifactual (3, 4). Alternative explanations should be considered. Differences in prevalence rates could be explained by 1) differences in sampling, which would affect for example sociodemographic characteristics of the populations studied (1); 2) differences in ascertainment methods (1); 3) differences in clinical syndromal profiles of cases (5); or 4) the toxic or withdrawal effects of psychoactive substances on mental functioning. People with psychosis live mainly in private households, but appreciable numbers are in temporary or homeless accommodations and in long-term institutions, including a range of different types of prison. In Great Britain, both primary healthcare and prison healthcare are funded from central taxation. A program of surveys assessing psychiatric morbidity and receipt of treatment and services was commenced during the 1990s in Great Britain (6) in order to determine progress toward health policy objectives. Nationally representative random samples of the private household and adult prison populations were selected from appropriate sampling frames. The aim of this study was to compare rates of psychotic mental disorder in these two national samples using identical methods of ascertainment and to seek explanation for the differences found.
Method
Psychiatric morbidity surveys were carried out in the general population throughout Great Britain (6). Interviewers with a minimum of 3 years experience with the Office for Population Censuses and Surveys (now the Office for National Statistics) carried out initial interviews. Delivery points (N=18,000) were drawn from the continuously updated Small Area Postcode Address File, stratifying for socioeconomic grouping within the English regions, Wales, and Scotland (7). Adults (N=12,730) were selected from 15,765 private households (Figure 1). Subjects selected for interview were those who 1) endorsed any of the five symptom groups (mania, thought disorder, paranoia, delusions, or auditory hallucinations) covered by questions from the self-report Psychosis Screening Questionnaire (8); 2) reported that they were taking antipsychotic medication; or 3) reported that they had been given a diagnosis of psychotic illness by a physician. Interviews were performed as soon afterward as possible by clinicians trained in the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) (9). Survey preparatory fieldwork had previously shown that psychosis cases identified by SCAN were not missed using these selection rules.
The SCAN is a semistructured interview covering axis I nonpsychotic and psychotic disorders, substance-related disorders, and organic brain disorders. Specific numbered sections of the SCAN cover particular syndromal groups or types of symptoms. For example, in the second part of the SCAN interview that covers psychotic symptoms, there are numbered sections covering clearcut hallucinations (section 17), subjectively described thought disorder and experiences of will replacement (section 18), and delusions (section 19) (9). The SCAN was developed by a joint task force of the World Health Organization and the U.S. Alcohol, Drug, and Mental Health Administration (9). Independently assessed agreement (using kappa) has been shown to exceed 0.8 for schizophrenia and affective psychosis (10, 11) and substance-related disorders (10). The SCAN consists of an interview guide providing the wording of questions about symptoms and a detailed glossary of symptoms. Every symptom and its threshold is defined in the glossary, and clinically experienced interviewers are trained to use question probes until the presence of each symptom can be confirmed or ruled out (12). In contrast to self-report questionnaires, in the SCAN the interviewer judges whether symptoms are present. Each type of psychotic symptom was rated individually for the year prior to interview. As part of the SCAN, clinicians also judged whether a symptom was attributable to any of a list of established toxic or withdrawal effects of alcohol or drug use listed in the SCAN glossary. We used published ICD-10 diagnostic algorithms (13) applied to SCAN symptom ratings to establish the presence of nonorganic psychosis in the year before interview, using ICD-10 codes F20–F31 (schizophrenia, delusional disorder, schizoaffective disorder, manic or bipolar affective disorder) and the ICD-10 F32–33 codes (depressive disorder) that require psychotic symptoms (14). Interviewers also coded any clearly established medical and organic causes such as epilepsy or brain damage according to ICD-10 criteria. In the absence of a SCAN interview in the household sample, a project diagnosis of probable functional psychosis was still made for anyone who reported taking antipsychotic medication and who also reported that they had a psychotic illness or that their doctor had told them that they had a psychotic illness, since this combination of responses was found to be most closely related to the presence of psychosis in those also clinically assessed (15).
All 131 prisons in England and Wales were visited during 1997. The Local Inmate Directory System—a computerized listing, updated daily, of all remanded and sentenced prisoners in England and Wales—was used to select prisoners according to the following sampling fractions: one in 34 male sentenced prisoners (1:50 in the final 4 weeks of the survey); one in eight remanded men (pretrial custody prisoners); and one in three of all women prisoners (16). Past research had shown different rates of disorder in these groups. These sampling fractions were therefore chosen in order to achieve sufficient numbers of interviews in these groups to provide percentages with standard errors of typically 1% and rarely more than 2%. A 1-in-5 random subsample of those who consented to participate were also interviewed with the SCAN (Figure 1). Symptoms in the past year were rated for diagnostic purposes as in the household survey. However, ratings for the past month were also made in order to register more transient symptoms of psychosis. In those not selected, a project diagnosis of probable functional psychosis (16) was made for anyone fulfilling any two of the following: a positive response to Psychosis Screening Questionnaire question “hearing voices”; a self-reported diagnosis of psychotic disorder; current antipsychotic medication; or a history of mental illness (admission to a mental hospital or mental illness in medical records), since this combination of responses was found to be most closely related to the presence of psychosis in those also assessed with the SCAN (16). The criteria for a project diagnosis of probable functional psychosis differed between the two surveys because, compared with those selected for assessment by a psychiatrist, the probability of being psychotic in those who were not selected for the SCAN interview was the same in the prison sample, whereas it was intended to be zero in the household sample.
In both surveys, written informed consent was obtained after the survey procedures had been fully explained. Standardized questions were asked covering employment and education, general health, access to health services, and treatment for general health and mental health problems. Respondents were asked the question: “In the past 12 months, have you spoken to a general practitioner or family doctor on your own behalf, either in person or by telephone, about being anxious or depressed or a mental, nervous, or emotional problem?” They were also asked “Are you taking any pills or tablets or any other medicine by mouth which have been prescribed for you?” Medicines were checked and coded during subsequent data entry according to the British National Formulary (17). In the prison survey, clinical interviewers also had access to prison health care records covering time in custody.
We compared the two samples in terms of sociodemographic profiles and the prevalence of probable functional psychosis in the past year. Such comparisons can be biased for two reasons: first, because of differences between the characteristics of a sample and those of the population from which it is drawn and second, because statistical adjustments made to correct for these differences can appear to be overprecise unless the method chosen for calculating standard errors takes into account the adjustment method. Prevalence estimates were adjusted by the use of weights calculated to reflect differences between the original characteristics of the populations studied and the interviewed samples. Replication (resampling) methods were used for analysis to produce valid estimates of variances for data with complex sampling structures including clustering and nonresponse (18). A finite population correction was made for the female prisoners, since more than 20% had been sampled. In order to explore factors possibly involved in prevalence differences between the two samples, we reexamined the prison sample after adjustment according to the household population characteristics. Differences between the two samples in clinical profile were evaluated by comparing the proportion of specific types of psychotic symptoms in prison and household respondents in whom the SCAN assessment had been completed. Use of health services and of treatments was also compared.
Results
Response rates in both surveys were good (7, 16) (Figure 1). Of 12,730 eligible households, 10,108 adults (79%) cooperated. Of 3,563 eligible sampled prisoners, 3,142 (88%) cooperated. Of 749 household residents who had positive psychosis screen results, 473 (63%) had a SCAN interview by a clinician. Of 661 prisoners who completed the initial survey interview and who were randomly selected for a follow-up clinical interview, 505 (76%) completed it.
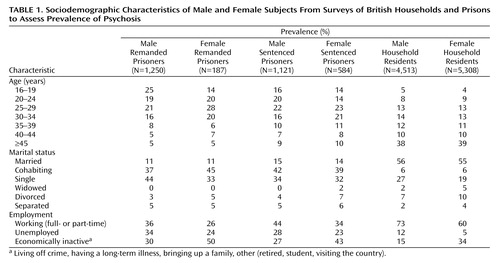
In mid-1997, the overall prison population of England and Wales (N=61,944) included 2,770 women prisoners and 12,302 male remanded prisoners, the remainder being sentenced males (16). Sociodemographic characteristics of the samples are presented in Table 1. Most prisoners were under 35 years of age, and one-quarter of the male remanded prisoners were 16 to 19 years of age, although a smaller proportion of sentenced males were in this age group (16%). Of the male remanded prisoners, 80% classified themselves as white, which was almost the same as among male sentenced prisoners (84%), female remanded prisoners (77%), and female sentenced prisoners (75%) but less than among household survey respondents (94%).
Prevalence of Psychosis
The prevalence of probable functional psychosis in the past year, adjusted for nonresponse and design clustering, was 4.5 per thousand (95% CI=3.1–5.8) in the household survey. In the prison survey, the adjusted rate was over 10 times greater: 52 per thousand (95% CI=45–60). Among male and female prisoners, rates were 50 (95% CI=42–57) and 110 (95% CI=100–120) per thousand, respectively.
Possible reasons for these prevalence differences were then considered. The prison population consisted substantially of younger adult male subjects. In order to take into account age and gender differences between the household and prison populations, we estimated the prison rate of probable functional psychosis, adjusted for the characteristics of the household population, as 70 per thousand (95% CI=60–80). Further adjustment for employment status did not change this.
Crude rates in subgroups of prison respondents undergoing the SCAN were also compared with rates of probable psychosis in the full samples. The unadjusted rate (per thousand) of psychotic mental disorder in 394 male prisoners who underwent a full SCAN clinical interview was 100 (95% CI=61–139) in remanded prisoners and 70 (95% CI=31–101) in sentenced prisoners. Unadjusted probable psychosis rates in 2,371 male remanded and sentenced prisoners were 90 (95% CI=70–110) and 40 (95% CI=20–60), respectively. Probable psychosis rates in prisoners who described themselves as black African, African Caribbean, and “black other” were low in male remanded prisoners (20 per thousand [95% CI=0–40]) and male sentenced prisoners (30 per thousand [95% CI=10–50]).
Frequency of Specific Psychotic Phenomena
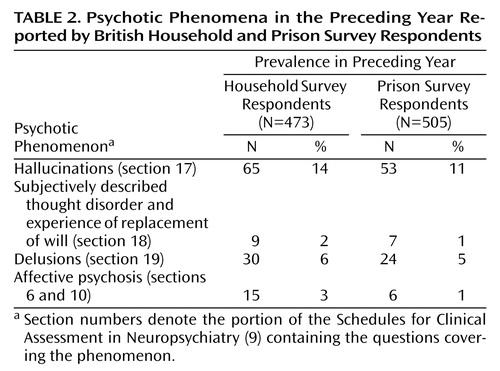
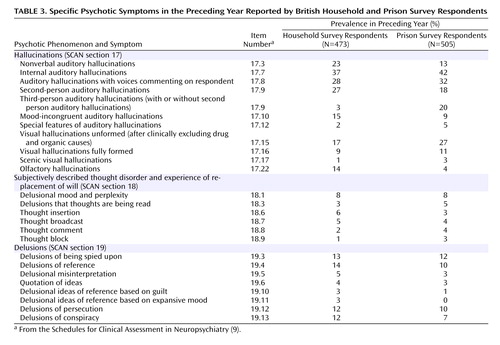
Although the small number of subjects with active clinically significant psychotic symptoms limited comparisons, unadjusted comparisons of clinical symptom profiles were carried out by using SCAN interview ratings from the two surveys. Approximately 8% of household survey respondents were selected for the SCAN, and 473 completed SCAN interviews were available (Figure 1); the 1-in-5 random subsample of prisoners (N=661) selected for a SCAN interview yielded 505 completed interviews. In general, we found remarkably similar frequencies of psychotic phenomena in prisoners and household residents (Table 2). Subjectively described thought disorder and experience of replacement of will (SCAN section 18) was infrequently rated but was no more common among prisoners than among household residents (Table 2). Organic factors were seldom judged to influence such symptoms.
Nonverbal and olfactory hallucinations appeared somewhat more prevalent in household residents with psychosis (Table 3). Visual hallucinations were found both in household residents and particularly in prisoners categorized with organic psychosis but, even when this was taken into account, it did not alter the small differences between household residents and prisoners (Table 3). No type of delusion occurred more often in prisoners (Table 3).
As expected, psychotic mental health problems attributed by the interviewers to toxic or withdrawal effects of alcohol or drug use were more common in the prison population. Among prisoners with SCAN-rated nonaffective psychotic symptoms (SCAN sections 17 to 19), 25% were judged to have such an origin. Two prisoners with nonaffective psychotic symptoms rated on the SCAN had ratings attributed to a possible organic cause. In only one prisoner whose psychotic mental health problems were attributable to alcohol or drug use was the organic cause judged clearly to be the major cause of those symptoms. No respondent in the household population with SCAN ratings of nonaffective psychotic symptoms received a clinician attribution of their psychosis to use of alcohol or drugs. Using the SCAN data, we found hardly any difference between the annual and 1-month psychosis estimate in prison.
Prison survey respondents who did not undergo a SCAN interview were classified as having probable functional psychosis if they endorsed two criteria: current psychotic medication and history of mental hospital admission (or history of mental illness). When we examined these cases, we found that hardly any were abusing stimulants or opiates in the year before entering prison or since detention.
Probable Psychosis and the Use of Services and Medication
Of adults from the household survey with a project diagnosis of probable functional psychosis, 63% had consulted a general practitioner (primary care physician) for a mental health problem during the previous year; the rates among the prison populations were 40% for remanded male prisoners, 37% in sentenced male prisoners, and 57% in sentenced female prisoners. Across all samples, female remanded prisoners were most likely to report having been admitted to a mental hospital (22%); only 8% of male sentenced prisoners had ever been admitted to a mental hospital. These proportions are substantially higher than those reported in the general population (19). Use of prescribed medication for psychosis and related conditions was remarkably similar in the two groups with probable psychosis: 34% among household residents and 38% and 34% in male remanded and sentenced prisoners, respectively. However, in the much smaller female prison population, the rates were 53% and 62% in remanded and sentenced prisoners, respectively.
Discussion
Reasons for the substantially higher prevalence of psychosis in the prison population need to be examined critically. Prevalence estimates based on the smaller number of prisoners interviewed clinically confirmed the high estimates made in those not selected for interview with the SCAN. In the two-phase household survey, respondents whose psychosis screen results were negative were not clinically evaluated (Figure 1). If 200 of the over 9,000 negative screen results had been clinically assessed, the discovery of 10 missed psychosis cases would have been necessary to explain the excess prevalence of prison psychosis. This number of false negatives seems unlikely, given that the selection rule was derived from an extensive presurvey fieldwork study (15). However, a second British household survey has since been completed that included the same selection questions and a modified design in which SCAN interviews were also carried out in a random sample who would not have been selected; this design did yield some initially missed positive cases. The report of this second household survey includes a detailed discussion of the psychosis prevalence estimate (20): taking into account the subjects with negative initial screen results, the psychosis prevalence estimate for household residents was 11.1 per thousand (95% CI=5.2–17.0), which was still well below the rate found in the present sample of prisoners randomly selected to undergo a SCAN assessment.
Another explanation for higher rates of psychosis in the prison population might lie in between-group differences in age and socioeconomic status (Table 1). Out of interest, we reweighted the prison data to have the same age, gender, and socioeconomic status as the general population, but this did not explain the increased prevalence in the prisons. Drug misuse and dependency may be significant prior risk factors for the development of severe mental disorder in vulnerable persons (21). In the present prison survey we found that a history of first use of amphetamines or cocaine before the age of 16 and severe cannabis or cocaine dependence were related to an increased risk of probable functional psychosis (22). However, our clinical interviewers could only attribute the presence of psychotic symptoms to the effects of such substances in approximately 1 in 4 psychosis cases. The relationship between psychoactive substance misuse and the development of nonorganic psychotic mental disorder appears to be associated with earlier age at initiation of drug use and with severity of dependence (22), possible indicators of prolonged heavy use. To date, it is not clear how the effects of chronic cannabinoid and psychostimulant use, the main substances implicated, contribute to or aggravate psychotic disorders.
Some differences in receipt of services and treatments for psychosis were found, but again these were not sufficient to explain the overall difference in psychosis prevalence. The use of this information could be limited by the uncertain reliability of self-report data on treatment and service use. Our detailed examination of individual psychosis syndromes and types of symptoms did not point to between-group differences in the proportion of case types for the two populations. It only served to confirm the much higher frequency of equivalent, recognizable psychotic phenomena in prisoners.
Previous Survey Comparisons
Other general population surveys that used similar assessment techniques have found similar prevalence rates to the Great Britain household study included here. For example, using the SCAN Jablensky and colleagues found a 1-year prevalence rate of psychosis between 4 and 7 per thousand in the adult population of urban Australia (2). Prison surveys have generally found higher rates but have used different assessment approaches. A systematic review of 62 surveys from 12 countries found a psychotic illness rate of 37 per thousand (95% CI=33–41) in 18,530 male prisoners, with a combined estimate of 4 times the general population rate (1). Unfortunately, the different time periods used in this combined estimate were not specified (1). Only one previous systematic direct comparison of prison and community data has been made (23): as determined with a fully structured interview, the lifetime rate of manic episodes for the prison population of Chicago was significantly higher than the community rate (Epidemiologic Catchment Area survey [24]), but the lifetime rate for schizophrenia/schizophreniform disorder was not significantly higher. However, doubts about the high rate of psychosis in prisons have persisted since the influential study of 2,070 adults in prisons throughout England in 1988 by Gunn et al. (25), who reported the prevalence (in the past month) of psychosis “warranting hospital treatment” to be 2% in 1,769 sentenced men and in 301 women. Case finding was based on ICD-9, a clinician rating of psychotic phenomena, and a consensus case conference for randomly sampled respondents and difficult cases. However, other work in prisons in England is in line with our findings: a consecutive series of 569 subjects remanded to one prison (26), evaluated with a structured clinical interview covering psychosis criteria in detail, found 70 lifetime cases per 1,000. Our psychosis cases may also include a wider range of psychotic disorders than the detailed SCAN clinical interview has identified. The prison psychosis rate may also have risen in the past decade because of the considerable expansion of prison places in England, the attendant closure of acute psychiatric inpatient beds, and the inadequacy during the intervening decade of court diversion and prison reception health screening (27).
Implications
Comparison of psychosis prevalence rates obtained from prison and household population surveys that used a similar ascertainment approach and involved 13,250 adults confirms that rates in prison are about 10 times higher. It appears unlikely that this excess can simply be attributed to the lower socioeconomic status and age of prisoners. Psychotic episodes in prison have the same form and clinical presentation of illness as those in the community, dispelling the notion that their clinical presentations are spurious or due to a putatively distinct “prison-psychosis” (5). The present British comparison provides firmer evidence that the substantially higher prevalence of psychotic disorder in prisons, which is also found in many other countries (1), is genuine and deserving of the full range of medical treatments and social care known to improve functioning and outcome. Policy makers and researchers now need to take these findings into account.
The public health policy implications of the high rate of severe mental illness in prisons and the lack of appropriate specialized care for this group have been commented upon (1, 28). When we compared adults with psychosis in the community with those in prison, fewer prisoners had consulted a doctor about their mental health problem in the last year. Good quality prison healthcare or mental health “in reach” services could provide effective treatment in many such cases. Elsewhere we have reported on a follow-up study of the prisoners with probable psychosis, most of whom had returned to the community at least once during the following year: less than a quarter had appointments with psychiatric professionals. For those with violent or sexual offenses, the rate only rose to 41% (29). Health and social care reforms to address this through closer links between prison and primary health care and specialist services are said to be underway in England and Wales (30), but there seems to be little attention to the problem elsewhere.
A crucial question is what health care and risk management are provided for severely mentally disturbed adults, particularly those who have committed serious and violent offenses, following release into the community. This is a priority for future research. We also require more detailed studies of drug misuse in populations with a high prevalence of psychotic symptoms, such as prisons. A growing body of longitudinal research (31) will also help to clarify factors that might contribute to these prevalence differences, including previous history of drug use and dependence, the response of services, and the widespread introduction of effective treatments.
 |
 |
 |
Received July 25, 2002; revisions received July 10, 2003, and March 31, 2004; accepted April 23, 2004. From the Clinical Division of Psychiatry, Department of Health Sciences, University of Leicester; Office for National Statistics, London; the Institute of Psychiatry, London; the London School of Hygiene and Tropical Medicine and Green College, Oxford, U.K.; the Department of Mental Health Sciences, University College London Medical School, London; the Forensic Psychiatry Research Unit, St. Bartholomew’s Hospital, London; the Department of Public Health and Primary Care, University of Cambridge, Cambridge, U.K.; and the Division of Psychiatry, Bristol University, Bristol, U.K. Address correspondence and reprint requests to Dr. Brugha, University of Leicester, Department of Health Sciences, Brandon Mental Health Unit, Leicester General Hospital, Gwendolen Rd., Leicester LE5 4PW, U.K.Both surveys were funded by Department of Health (England) contracts to the Office for National Statistics, Social Survey Division, London, which carried out fieldwork.
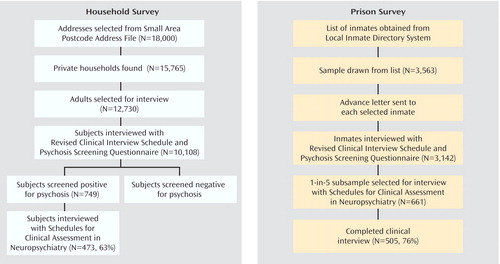
Figure 1. Procedures for Surveys of British Households and Prisons to Assess Prevalence of Psychosis
1. Fazel S, Danesh J: Serious mental disorder in 23,000 prisoners: a systematic review of 62 surveys. Lancet 2002; 359:545–550Crossref, Medline, Google Scholar
2. Jablensky A, McGrath JJ, Herrman H, Castle DJ, Gureje O, Morgan V, Korten A: People Living With Psychotic Illness: An Australian Study 1997–1998. Canberra, Commonwealth of Australia, National Survey of Mental Health and Wellbeing, 1999Google Scholar
3. Brooke D, Taylor C, Gunn J, Maden A: Point prevalence of mental disorder in unconvicted male prisoners in England and Wales. BMJ 1996; 313:1524–1527Crossref, Medline, Google Scholar
4. Coid J: How many psychiatric patients in prison? Br J Psychiatry 1984; 145:78–86Crossref, Medline, Google Scholar
5. Arboleda-Florez J: Post-homicide psychotic reaction. Int J Offender Ther Comp Criminol 1980; 24:47–52Google Scholar
6. Jenkins R, Bebbington P, Brugha T, Farrell M, Gill B, Lewis G, Meltzer H, Petticrew M: The National Psychiatric Morbidity Surveys of Great Britain—strategy and methods. Psychol Med 1997; 27:765–774Crossref, Medline, Google Scholar
7. Jenkins R, Lewis G, Bebbington P, Brugha T, Farrell M, Gill B, Meltzer H: The National Psychiatric Morbidity Surveys of Great Britain—initial findings from the household survey. Psychol Med 1997; 27:775–789Crossref, Medline, Google Scholar
8. Bebbington PE, Nayani T: The Psychosis Screening Questionnaire. Int J Methods Psychiatr Res 1995; 5:11–20Google Scholar
9. Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, Jablenski A, Regier D, Sartorius N: SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry 1990; 47:589–593Crossref, Medline, Google Scholar
10. Wing JK, Sartorius N, Der G: International field trials: SCAN-0, in Diagnosis and Clinical Measurement in Psychiatry: A Reference Manual for SCAN/PSE-10. Edited by Wing JK, Sartorius N, Ustün TB. Cambridge, Cambridge University Press, 1998, pp 86–109Google Scholar
11. Brugha TS, Nienhuis FJ, Bagchi D, Smith J, Meltzer H: The survey form of SCAN: the feasibility of using experienced lay survey interviewers to administer a semi-structured systematic clinical assessment of psychotic and non psychotic disorders. Psychol Med 1999; 29:703–712Crossref, Medline, Google Scholar
12. Ustün TB, Harrison GL, Chatterji S: Training in the use of SCAN, in Diagnosis and Clinical Measurement in Psychiatry: A Reference Manual for SCAN/PSE-10. Edited by Wing JK, Sartorius N, Ustün TB. Cambridge, Cambridge University Press, 1998, pp 68–85Google Scholar
13. Der G, Wing JK: CATEGO-5: The ICD 10 Program. Geneva, World Health Organization, 1992Google Scholar
14. World Health Organization Division of Mental Health: Mental and behavioural disorders (including disorders of psychological development): diagnostic criteria for research, in International Classification of Diseases, 10th ed. (May 1990 draft for field trials). Geneva, WHO, 1990Google Scholar
15. Meltzer H, Gill B, Petticrew M, Hinds K: OPCS Surveys of Psychiatric Morbidity in Great Britain, Report 1: The Prevalence of Psychiatric Morbidity Among Adults Living in Private Households. London, Her Majesty’s Stationary Office, 1995Google Scholar
16. Singleton N, Meltzer H, Gatward R, Coid J, Deasy D: Psychiatric Morbidity Among Prisoners in England and Wales: A Survey Carried Out in 1997 by the Social Survey Division of ONS on Behalf of the Department of Health. London, Her Majesty’s Stationary Office, 1998Google Scholar
17. British National Formulary, 40th ed. London, British Medical Association and the Royal Pharmaceutical Society of Great Britain, 2000Google Scholar
18. Westat: WesVar Complex Samples, Version 3.0: User’s Guide. Chicago, SPSS, 1998Google Scholar
19. Bebbington P, Brugha T, Meltzer H, Jenkins R, Ceresa C, Farrell M, Lewis G: Neurotic disorders and the receipt of psychiatric treatment. Psychol Med 2000; 30:1369–1376Crossref, Medline, Google Scholar
20. Singleton N, Bumpstead R, O’Brien M, Lee A, Meltzer H: Psychiatric Morbidity Among Adults Living in Private Households: National Statistics, 154. London, Her Majesty’s Stationary Office, 2001Google Scholar
21. Kwapil TR: A longitudinal study of drug and alcohol use by psychosis-prone and impulsive-nonconforming individuals. J Abnorm Psychol 1996; 105:114–123Crossref, Medline, Google Scholar
22. Farrell M, Boys A, Bebbington P, Brugha T, Coid J, Jenkins R, Lewis G, Meltzer H, Marsden J, Singleton N, Taylor C: Psychosis and drug dependence results from a national survey of prisoners. Br J Psychiatry 2002; 181:393–398Crossref, Medline, Google Scholar
23. Teplin LA, Abram KM, McClelland GM: Prevalence of psychiatric disorders among incarcerated women, I: pretrial jail detainees. Arch Gen Psychiatry 1996; 53:505–512Crossref, Medline, Google Scholar
24. Robins LE, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD, Regier DA: Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 1984; 41:949–957Crossref, Medline, Google Scholar
25. Gunn J, Maden A, Swinton M: Treatment needs of prisoners with psychiatric disorders. BMJ 1991; 303:338–341Crossref, Medline, Google Scholar
26. Birmingham L, Mason D, Grubin D: Prevalence of mental disorder in remand prisoners: consecutive case study. BMJ 1996; 313:1521–1524Crossref, Medline, Google Scholar
27. Birmingham L, Mason D, Grubin D: Health screening at first reception into prison. Am J Forensic Psychiatry 1997; 8:435–439Crossref, Google Scholar
28. Fryers T, Brugha T, Grounds A, Melzer D: Severe mental illness in prisoners: a persistent problem that needs a concerted and long term response. BMJ 1998; 317:1025–1026Crossref, Medline, Google Scholar
29. Melzer D, Tom B, Brugha TS, Fryers T, Grounds A, Johnson A, Meltzer H, Singleton N: Prisoners with psychosis in England and Wales: a one year national follow-up study. Howard J Criminal Justice 2002; 41:1–13Crossref, Google Scholar
30. Department of Health: National Service Frameworks for Mental Health: Modern Standards and Service Models. London, United Kingdom Department of Health, 1999Google Scholar
31. Williams A, Farrell M: Substance misuse and psychosis. Psychiatry 2004; 3:52–54Crossref, Google Scholar



