Impulse Control Disorders in Adult Psychiatric Inpatients
Abstract
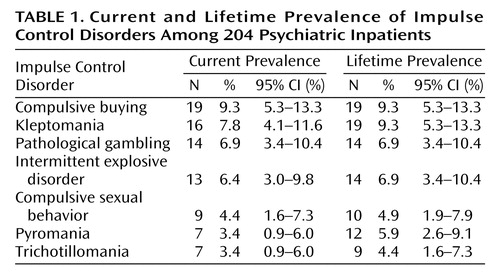
OBJECTIVE: The authors’ goal was to examine the prevalence of impulse control disorders in psychiatric inpatients. METHOD: They used the Minnesota Impulsive Disorders Interview, a semistructured clinical interview assessing pathological gambling, trichotillomania, kleptomania, pyromania, intermittent explosive disorder, compulsive buying, and compulsive sexual behavior, to screen 204 consecutively admitted psychiatric inpatients. One hundred twelve of the inpatients were women (54.9%), and the mean age of the 204 inpatients was 40.5 years (SD=13.2, range=18–83). Patients whose screen was positive for an impulse control disorder were evaluated with structured clinical interviews. RESULTS: Sixty-three patients (30.9%) were diagnosed with at least one current impulse control disorder. The most common impulse control disorders were compulsive buying (N=19 [9.3%]), kleptomania (N=16 [7.8%]), and pathological gambling (N=14 [6.9%]). Patients with and without co-occurring impulse control disorders did not differ significantly from each other on demographic measures or number or type of psychiatric diagnoses other than impulse control disorders. CONCLUSIONS: Impulse control disorders appear common among psychiatric inpatients. Additional, larger studies are needed to examine the prevalence of impulse control disorders in the general population and specific psychiatric groups.
Impulsivity, defined as a predisposition to rapid, unplanned reactions to internal or external stimuli without regard to the negative consequences of these reactions to the impulsive individual or to others (1), is a core feature of many psychiatric disorders, including attention deficit hyperactivity disorder, bipolar disorder, and substance use disorders. Disorders characterized by an impaired ability to resist impulses to engage in ultimately self-destructive behavior (or behavior with deleterious long-term consequences) have been categorized in DSM as impulse control disorders not elsewhere classified. These disorders, currently including pathological gambling, kleptomania, intermittent explosive disorder, trichotillomania, pyromania, and impulse control disorder not otherwise specified, have historically received little clinical and research attention. Diagnostic criteria for compulsive sexual behavior and compulsive buying have been proposed because preliminary data suggest that these behaviors may be linked to other impulse control disorders (2, 3).
Data suggest that impulse control disorders are relatively common, carry substantial morbidity and mortality, and may be treated effectively with behavioral and pharmacological therapies (4). Although pathological gambling has prevalence estimates similar to those for bipolar disorder and schizophrenia (5), few investigations have examined the prevalence of other impulse control disorders. Two French studies involving 107 depressed and 79 alcoholic inpatients (6, 7) found that 19% and 38%, respectively, had positive screens for a co-occurring impulse control disorder.
The co-occurrence of impulse control disorders and other psychiatric disorders has treatment implications. Individuals with co-occurring impulse control disorders and other psychiatric disorders generally have more severe symptoms, suggesting that untreated impulse control disorders may complicate treatment of the identified psychiatric disorder (8). Since empirically validated treatments for impulse control disorders are available, it is important for psychiatrists to identify and treat people with these disorders.
Our goal in this study was to examine the frequency of co-occurring impulse control disorders in voluntarily hospitalized psychiatric patients using structured diagnostic measures. On the basis of earlier studies, we hypothesized that impulse control disorders would be common.
Method
The study and consent forms were reviewed and approved by the institutional review boards of the two hospitals whose inpatients were studied. All patients provided written informed consent. Two hundred four consecutive patients presenting for admission to an inpatient unit at a private psychiatric (N=103) or public university (N=101) hospital participated. The group included 112 women (54.9%), and the mean age of the 204 patients was 40.5 years (SD=13.2, range=18–83).
Inclusionary criteria included voluntary admission and ability to read and understand the consent form. To avoid possible consent under duress, patients admitted involuntarily were not approached for participation. No patient refused participation. Demographic variables (age, gender, race, ethnicity, marital status, and education) and admission psychiatric diagnoses were taken from patients’ charts.
Two psychiatrists trained on the study instruments and in the phenomenology of impulse control disorders (L.L. and D.K.) evaluated all subjects for current and lifetime impulse control disorders with the Minnesota Impulsive Disorders Interview (9). This instrument is used to screen for pathological gambling, trichotillomania, kleptomania, pyromania, intermittent explosive disorder, compulsive buying, and compulsive sexual behavior (9–12). It evaluates each disorder beginning with a general question, which, if answered affirmatively, allows the interviewer to ask a series of questions mirroring DSM criteria. For compulsive buying and compulsive sexual behavior, the questions in the Minnesota Impulsive Disorders Interview reflect the impulse control disorder criteria of increasing tension before the related act followed by relief after act performance and subsequently evaluate related distress and impairment. A subject’s Minnesota Impulsive Disorders Interview screen is positive for a disorder if all questions are answered affirmatively (except the pathological gambling screen, which requires five positive responses, and compulsive sexual behavior screen, which requires an affirmative answer to one of two questions). The psychiatrist performing the screening interview scored the instrument.
Subjects with a positive screen for an impulse control disorder were evaluated in a structured clinical interview conducted by a different psychiatrist with expertise in impulse control disorders (J.E.G.), who was unaware of the impulse control disorder(s) for which the subject had a positive screen. This second assessment involved administration of all of the following instruments: the Structured Clinical Interview for Pathological Gambling (13), a valid and reliable diagnostic instrument based on the Structured Clinical Interview for DSM-IV (SCID); proposed diagnostic criteria for compulsive buying (2) and compulsive sexual behavior (3); the Structured Clinical Interview for Kleptomania (14), a diagnostic interview with good psychometric properties; and SCID-compatible modules based on DSM-IV diagnostic criteria for pyromania, trichotillomania, and intermittent explosive disorder.
The percentages of patients with current and lifetime impulse control disorders were determined, along with 95% confidence intervals. Between-group differences were tested by using Pearson chi-square tests and two-sided Fisher exact tests for categorical variables and two-tailed independent samples t tests for continuous variables. Because multiple pairwise comparisons were made, a Bonferroni correction was used, resulting in a significance threshold of p=0.008.
Results
Frequencies of individual impulse control disorders are presented in Table 1. Compulsive buying was the most common current and lifetime impulse control disorder and trichotillomania the least common. Sixty-three (30.9%) of the 204 patients were diagnosed with at least one impulse control disorder. Forty-two patients (20.6%) reported current symptoms of two impulse control disorders, 20 (9.8%) three impulse control disorders, and one (0.5%) more than three impulse control disorders. Sixty-seven patients (32.8%) were diagnosed with at least one lifetime impulse control disorder. Only four patients had a previous impulse control disorder; they reported no symptoms of an impulse control disorder within the last year.
Participants were admitted for multiple psychiatric reasons. Only three of the patients were admitted for an impulse control disorder (two for pathological gambling and one for intermittent explosive disorder). One hundred ten patients (53.9%) suffered from two or more psychiatric disorders, not including an impulse control disorder. Mood disorders, seen in 148 patients (72.5%), were the most common. Other psychiatric disorders included substance use disorders (N=90 [44.1%]), anxiety disorders (N=27 [13.2%]), psychotic disorders (N=23 [11.3%]), eating disorders (N=9 [4.4%]), adjustment disorders (N=7 [3.4%]), and somatization disorders (N=2 [1.0%]).
Patients with co-occurring impulse control disorders did not significantly differ from those without impulse control disorders on demographic measures (Table 2). The two groups also did not differ significantly with respect to the number or type of other psychiatric diagnoses, although the group with impulse control disorders was marginally more likely than those without to report two or more psychiatric diagnoses other than impulse control disorders (Table 2). No significant differences in demographic or diagnostic characteristics were observed between patients admitted to the private versus public hospitals (data not shown).
The Minnesota Impulsive Disorders Interview demonstrated classification accuracy based on the subsequent structured clinical interviews as follows: compulsive buying (sensitivity 100%, specificity 96.2%); kleptomania (sensitivity 89.5%, specificity 93.0%); pathological gambling (sensitivity 100%, specificity 98.4%); intermittent explosive disorder (sensitivity 100%, specificity 97.4%); compulsive sexual behavior (sensitivity 80.0%, specificity 96.9%); pyromania (sensitivity 100%, specificity 100%); and trichotillomania (sensitivity 100%, specificity 98.5%).
Discussion
We found that approximately one-third of the adult patients admitted for inpatient psychiatric treatment suffered from a co-occurring impulse control disorder. Only 1.5% of the inpatients carried an admission diagnosis for an impulse control disorder, however, suggesting that these disorders frequently go unrecognized. The current and lifetime estimates found here (30.9% and 32.8%, respectively) are consistent with findings of two earlier French studies that assessed impulse control disorders in smaller groups of psychiatric inpatients with alcohol use disorders and depression (6, 7). Together, the findings suggest that impulse control disorders occur commonly across cultures in inpatient psychiatric populations. Unlike the studies in France, the results from our larger study also suggest that impulse control disorders are common among psychiatric inpatients with a broad range of disorders, including anxiety disorders and psychotic disorders. Prevalence estimates of impulse control disorders did not differ between patients admitted to the private and public hospitals, suggesting that impulse control disorders are common in different inpatient treatment settings.
The range of impulse control disorders identified extends beyond those currently included in the DSM category of impulse control disorders not otherwise classified. Compulsive buying, currently not a formal DSM-IV-TR diagnosis, was the most common current and lifetime impulse control disorder, suggesting the need for consideration of formal criteria for the disorder in the next DSM revision. Previous studies (15, 16) have suggested that kleptomania and pyromania are rare. This study, however, found kleptomania to be one of the most common lifetime impulse control disorders; estimates of pyromania were only slightly less than those for pathological gambling, an impulse control disorder that has received more clinical and research attention.
Because impulse control disorders appear common in inpatients with other psychiatric disorders, it seems important to screen for impulse control disorders in this population. The fact that estimates of lifetime impulse control disorders (32.8%) were not notably different from those of current impulse control disorders (30.9%) suggests that these disorders may become chronic if left untreated. Treatment of either an impulse control disorder or another psychiatric disorder could be complicated or compromised by the presence of the other untreated condition. Treating one disorder alone may not be effective if a co-occurring disorder is exerting a causal or maintaining influence on the treated condition. To our knowledge, no research has been published on the treatment of co-occurring impulse control disorders in patients with other psychiatric disorders. Research on effective treatments for psychiatric patients with co-occurring impulse control disorders is needed.
This study has several limitations. First, impulse control disorder diagnoses were based on subject report—supporting collateral information was not obtained. Because behaviors associated with impulse control disorders are often denied, the observed frequencies probably underestimate those of actual impulse control disorders among psychiatric inpatients. Second, other disorders characterized by impaired impulse control (compulsive computer use, binge eating disorder) were not assessed; consequently, the rates of impulse control disorders might be higher than reported here. Conversely, studies done in clinical settings bias toward finding high rates of co-occurrence (due to Berkson’s bias [17] and clinical biases). Third, it is unclear how generalizable our results are to patients admitted to psychiatric facilities against their will, psychiatric outpatients, or individuals in the community. Fourth, the instruments used to screen for and diagnose impulse control disorders (Minnesota Impulsive Disorders Interview, Structured Clinical Interview for Pathological Gambling, Structured Clinical Interview for Kleptomania, criteria for compulsive buying and compulsive sexual behavior, and the SCID-compatible modules for pyromania, trichotillomania, and intermittent explosive disorder) lack rigorously tested psychometric properties, particularly when used as a group. Comprehensive testing of a diagnostic battery of impulse control disorders is needed.
Although impulse control disorders appear common among psychiatric inpatients, these results should be considered tentatively and as preliminary. No empirically validated diagnostic instruments for these disorders currently exist, and this represents a research need. Additional research requirements include large prevalence investigations, identification of clinical correlates of impulse control disorders in psychiatric groups, studies on the relationship between impulse control disorders and other disorders, and treatment trials to identify safe and efficacious treatments for patients with both impulse control disorders and other psychiatric disorders.
 |
 |
Received June 3, 2004; revision received July 21, 2004; accepted Sept. 13, 2004. From Brown Medical School and Butler Hospital, Providence, R.I.; and Yale University Medical School, New Haven, Conn. Address correspondence to Dr. Grant, Department of Psychiatry, University of Minnesota, 2450 Riverside Ave., Minneapolis, MN 55454; [email protected] (e-mail). Supported in part by National Institute on Drug Abuse grant MNP-K12 DA-00167 from the Clinician Scientist Training Program.
1. Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC: Psychiatric aspects of impulsivity. Am J Psychiatry 2001; 158:1783–1793Link, Google Scholar
2. McElroy SL, Keck PE Jr, Pope HG Jr, Smith JM, Strakowski SM: Compulsive buying: a report of 20 cases. J Clin Psychiatry 1994; 55:242–248Medline, Google Scholar
3. Black DW, Kehrberg LLD, Flumerfelt DL, Schlosser SS: Characteristics of 36 subjects reporting compulsive sexual behavior. Am J Psychiatry 1997; 154:243–249Link, Google Scholar
4. Grant JE, Potenza MN: Impulse control disorders: clinical characteristics and pharmacological management. Ann Clin Psychiatry 2004; 16:27–34Crossref, Medline, Google Scholar
5. Shaffer HJ, Hall MN, Vander Bilt J: Estimating the prevalence of disordered gambling behavior in the United States and Canada: a research synthesis. Am J Public Health 1999; 89:1369–1376Crossref, Medline, Google Scholar
6. Lejoyeux M, Arbaretaz M, McLoughlin M, Ades J: Impulse control disorders and depression. J Nerv Ment Dis 2002; 190:310–314Crossref, Medline, Google Scholar
7. Lejoyeux M, Feuche N, Loi S, Solomon J, Ades J: Study of impulse-control disorders among alcohol-dependent patients. J Clin Psychiatry 1999; 60:302–305Crossref, Medline, Google Scholar
8. Potenza MN, Fiellin DA, Heninger GR, Rounsaville BJ, Mazure CM: Gambling: an addictive behavior with health and primary care implications. J Gen Intern Med 2002; 17:721–732Crossref, Medline, Google Scholar
9. Christenson GA, Faber RJ, de Zwaan M, Raymond NC, Specker SM, Ekern MD, Mackenzie TB, Crosby RD, Crow SJ, Eckert ED, Mussel MP, Mitchell JE: Compulsive buying: descriptive characteristics and psychiatric comorbidity. J Clin Psychiatry 1994; 55:5–11Medline, Google Scholar
10. Raymond NC, Coleman E, Miner MH: Psychiatric comorbidity and compulsive/impulsive traits in compulsive sexual behavior. Compr Psychiatry 2003; 44:370–380Crossref, Medline, Google Scholar
11. Black DW, Belsare G, Schlosser S: Clinical features, psychiatric comorbidity, and health-related quality of life in persons reporting compulsive computer use behavior. J Clin Psychiatry 1999; 60:839–844Crossref, Medline, Google Scholar
12. Black DW, Moyer T: Clinical features and psychiatric comorbidity of subjects with pathological gambling behavior. Psychiatr Serv 1998; 49:1434–1439Link, Google Scholar
13. Grant JE, Steinberg MA, Kim SW, Rounsaville BJ, Potenza MN: Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatr Res 2004; 128:79–88Crossref, Medline, Google Scholar
14. Grant JE, Kim SW, McCabe J: A Structured Clinical Interview for Kleptomania (SCI-K): preliminary validity and reliability testing. Int J Methods Psychiatr Res (in press)Google Scholar
15. Ritchie EC, Huff TG: Psychiatric aspects of arsonists. J Forensic Sci 1999; 44:733–740Medline, Google Scholar
16. Goldman MJ: Kleptomania: making sense of the nonsensical. Am J Psychiatry 1991; 148:986–996Link, Google Scholar
17. Berkson S: Limitations of the application of fourfold table analysis to hospital data. Biometrics Bulletin 1946; 2:47–53Crossref, Google Scholar



