In This Issue
Rescue Workers in Need of Rescue
The events of Sept. 11, 2001, highlighted rescue workers’ personal involvement in disasters. To identify predictors of psychiatric disorders among emergency personnel, Fullerton et al. (p. 1370) examined responders to a crash of a large passenger jet. By 13 months after the crash, more than 40% of the workers had experienced a psychiatric disorder. The rates of posttraumatic stress disorder (PTSD) and depression at that time were 17% and 22%, respectively, compared to 2% and 13% in responders who handled only ordinary emergencies. PTSD was nearly seven times as likely among those with previous disaster experience. Other risk factors were depression and a higher number of dissociative symptoms (e.g., feeling of numbness or unreality) during the week following the crash. Acute stress disorder in the first week predicted both PTSD and depression and is thus a cause for both short- and long-term concern.
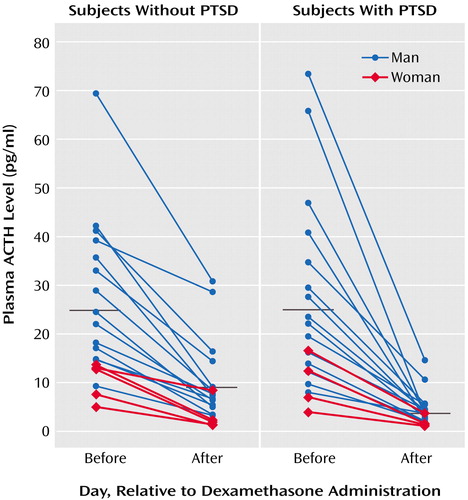
Endocrine Origins of PTSD
Patients with posttraumatic stress disorder (PTSD) have numerous endocrine abnormalities. Several involve the “stress hormone” cortisol, but the hypothalamic-pituitary-adrenal (HPA) system includes internal feedback, and it is difficult to pinpoint where problems begin. Yehuda et al. (p. 1397) tested two possibilities: one, that negative feedback within the HPA axis is exaggerated in PTSD, thereby inhibiting overall activity, and two, that the adrenal glands of PTSD patients produce reduced amounts of cortisol. The findings supported the first hypothesis. The cortisone-like agent dexamethasone decreased both cortisol and adrenocorticotropic hormone (ACTH) more in PTSD patients than in healthy subjects. ACTH is thought to respond to dexamethasone upstream of the adrenal glands, and so the parallel responses of ACTH and cortisol suggest an overall effect, rather than adrenal insufficiency, which would affect cortisol only.
Grief at an Early Age
A teenager who commits suicide leaves behind young friends and acquaintances who are affected in different ways and to different degrees. Knowledge about normal and pathological grief mostly comes from studies of adults who have lost spouses. Among adolescents who knew someone who committed suicide, however, Melhem et al. (p. 1411) describe a syndrome resembling the traumatic grief of adults. The teens were interviewed 6 months after the suicide and were followed up at 12–18 and 36 months. Traumatic grief was present in 25% at 6 months and predicted depression and posttraumatic stress disorder (PTSD) at follow-up. Traumatic grief co-occurred with PTSD. However, they did not always overlap, so the two appear to be distinct. One characteristic that may differentiate grieving adolescents from adults is the course of traumatic grief, which decreased greatly after 6 months among these teenagers but affects many adults with conjugal bereavement for 2 years or more.
Therapist Distress After Patient Suicide
Surveys have shown that about half of psychiatrists and one-quarter of psychologists have had patients who committed suicide. Some therapists react more intensely than others, and Hendin et al. (p. 1442) explored these emotional responses among psychiatrists, psychologists, and a psychiatric social worker. Of the 34 therapists, 38% rated their distress as 7 or higher on a 10-point scale. For each of these therapists the distress was attributed to one of four factors: failure to hospitalize a suicidal patient, treatment decisions felt to contribute to the suicide, blame by the therapist’s institution, and fear of a lawsuit. Grief and guilt feelings were described as intense by almost all of the severely distressed therapists. Each of those with severe reactions reported that the experience lasted at least 1 year after the suicide.
Predicting the Future for Bipolar Patients
Relapse is common among patients with bipolar disorder. Besides obtaining treatment, is there anything they can do to improve their prospects? A 1-year survey by Nolen et al. (p. 1447) suggests that reducing substance abuse could help, since a history of substance abuse was associated with more severe mania in patients with bipolar disorder. Also, a family history of drug abuse was related to a higher number of episodes in the 1-year follow-up. Surprisingly, a family history of mood disorders was not related to outcome. Nor was earlier onset. Other characteristics that did predict a higher number of episodes or greater severity were 10 or more previous manic episodes at the beginning of the study, 10 or more previous depressive episodes, prior rapid cycling between mania and depression, a history of child abuse, and poor occupational functioning at baseline. Even these historical factors may help guide treatment and set goals.
Images in Psychiatry
Theodor Ziehen, M.D., Ph.D., 1862–1950 (p. 1369)