Malnutrition at Age 3 Years and Externalizing Behavior Problems at Ages 8, 11, and 17 Years
Abstract
OBJECTIVE: Poor nutrition is thought to predispose to externalizing behavior problems, but to date there appear to have been no prospective longitudinal studies testing this hypothesis. This study assessed whether 1) poor nutrition at age 3 years predisposes to antisocial behavior at ages 8, 11, and 17 years, 2) such relationships are independent of psychosocial adversity, and 3) IQ mediates the relationship between nutrition and externalizing behavior problems. METHOD: The participants were drawn from a birth cohort (N=1,795) in whom signs of malnutrition were assessed at age 3 years, cognitive measures were assessed at ages 3 and 11 years, and antisocial, aggressive, and hyperactive behavior was assessed at ages 8, 11, and 17 years. RESULTS: In relation to comparison subjects (N=1,206), the children with malnutrition signs at age 3 years (N=353) were more aggressive or hyperactive at age 8 years, had more externalizing problems at age 11, and had greater conduct disorder and excessive motor activity at age 17. The results were independent of psychosocial adversity and were not moderated by gender. There was a dose-response relationship between degree of malnutrition and degree of externalizing behavior at ages 8 and 17. Low IQ mediated the link between malnutrition and externalizing behavior at ages 8 and 11. CONCLUSIONS: These results indicate that malnutrition predisposes to neurocognitive deficits, which in turn predispose to persistent externalizing behavior problems throughout childhood and adolescence. The findings suggest that reducing early malnutrition may help reduce later antisocial and aggressive behavior.
Despite decades of research into social and biological risk factors for childhood aggression, surprisingly little is known about the role of malnutrition in contributing to the development of childhood externalizing behavior (1, 2). Although deficiency in nutrition has been rarely studied in relation to externalizing behavior, several studies have demonstrated the effects of related factors, including food additives, hypoglycemia, and, more recently, cholesterol (2–4), on human behavior. In addition, epidemiological studies have shown associations between increased aggressive behavior and vitamin and mineral deficiency (5, 6). Several authors have also claimed links between iron-deficient anemia or low zinc level and externalizing behavior in childhood (7, 8). More recently, the male offspring of nutritionally deprived pregnant women were found to have 2.5 times the normal rate of antisocial personality disorder in adulthood (9). Effects were found for severe malnutrition during the first and second trimesters of pregnancy, but not the third trimester. Despite these findings, the research literature on malnutrition and externalizing behavior problems remains both limited and controversial (2, 10).
If malnutrition is linked to antisocial behavior, as some suggest, a key question concerns the mechanism of action. One possible, but so far untested, hypothesis is that early malnutrition predisposes to antisocial behavior because malnutrition impairs neurocognitive functioning, which in turn predisposes to externalizing behavior problems. There is now compelling evidence that externalizing behavior problems are characterized by lower IQ (11–14), and furthermore, there is evidence that these early neurocognitive deficits predict the onset of antisocial behavior (1, 15, 16). In addition, there is increasing evidence that malnutrition predisposes to lower IQ (17, 18). We recently observed that malnutrition at age 3 was related to lower IQ at age 3 and age 11 in a large longitudinal study in Mauritius (19), while similar findings have also been observed by others (17, 20). Despite the plausibility of the malnutrition-externalizing hypothesis, we know of no empirical tests of it to date.
Research on nutrition and antisocial behavior has five important limitations. First, there are simply very few studies that have assessed the relationship between nutritional deficits and externalizing behavior. Second, with the exception of the prenatal study by Neugebauer et al. (9), studies have not investigated prospectively the effect of early nutrition on later aggressive behavior; it is possible, for example, that antisocial behavior in the child could produce parental neglect and malnutrition, rather than vice versa. Third, there have been few, if any, studies on the relation between nutritional deficits and aggression in females as well as males. Fourth, to our knowledge, the possibility of mediating mechanisms, such as neurocognitive deficits, have not been tested. Fifth, prior studies have rarely controlled for the confounding effects of psychosocial adversity.
In this study we used longitudinal data from Mauritius in order to begin to address these gaps in the literature by testing the following hypotheses: 1) poor nutrition at age 3 years predisposes to antisocial behavior at ages 8, 11, and 17 years, 2) such relationships are independent of early psychosocial adversity, and 3) IQ mediates the nutrition-antisocial relationship. If controlling for childhood intelligence abolishes the relationship between early malnutrition and later externalizing behavior problems, this would provide evidence for the role of intelligence as a significant mediating mechanism (21).
Method
Participants
Participants were drawn from a birth cohort of 1,795 children from the island of Mauritius, which lies off the coast of Africa. On the basis of vaccination records, all children born in 1969 and 1970 in two main towns on the island were recruited into the study between September 1972 and August 1973 when they were 3 years old. The two towns (Vacoas and Quatre Bornes) were chosen because they were representative of the ethnic distribution of the whole island. The sample consisted of both boys (51.4%) and girls (48.6%). The ethnic distribution was as follows: Indian, 68.7%; Creole (African origin), 25.7%; and other (Chinese, English, and French), 5.6%. Census data for the island as a whole indicated 66% Indian, 29% Creole, and 5% other, indicating that the study largely achieved its goal of representing the ethnicity of the population. In keeping with previous work on this population (14, 22), the data analyses were restricted to Indians and Creoles because of the small number of subjects in the “other” ethnic category. Oral informed consent was obtained from the mothers of the participants in the early phases and from the participants themselves in the age 17 phase. Early research activities were conducted according to the principles outlined in the Declaration of Helsinki (23), which prevailed in 1972, when the research was initiated, while research activities in later years were conducted according to principles outlined in the Belmont Report (24). Institutional review board approval for the later research phases and retrospective data analyses was obtained from the University of Southern California and from the University of California, Los Angeles.
Signs of Malnutrition at Age 3
At age 3 years, four early signs of malnutrition (19) were assessed in a clinical examination of 1,559 of the children. Assessments of the children were conducted with a structured protocol by local pediatricians who had received their medical training in Europe. All assessments were conducted at the research unit. The four signs were as follows:
Angular stomatitis
Cracking in the lips and corners of the mouth is predominantly a sign of riboflavin deficiency (vitamin B2) but also reflects niacin deficiency (25, p. 97). The base rate for angular stomatitis in the sample was 7.0%.
Hair dyspigmentation
This condition reflects protein malnutrition (26) and is found in tropical regions, particularly in Africa (26), where children’s hair takes on a reddish-orange color. The base rate for red hair in the sample was 6.8%.
Sparse, thin hair
This indicator is a sign of protein-energy malnutrition in particular (27, 28) and malnutrition in general (29). Protein reduction impairs hair growth, while zinc and iron deficiency can also lead to thin hair. The base rate for this symptom in the sample was 5.8%.
Anemia
Anemia was indicated by a low hemoglobin level, which reflects iron deficiency. Hemoglobin level was assessed from a laboratory test of blood drawn from the child. Anemia was defined as a hemoglobin level below 8.5 g/dl. This definition of anemia was consistent with medical practice in Mauritius in the early 1970s. The base rate in this sample was 17.0%.
Definition of malnutrition
A participant was defined as suffering from nutritional deficits if at least one of the four preceding indicators was present; 22.6% of the assessed children met this definition. A participant with no indicator present was classified as having relatively normative nutrition; 77.4% fit this category. To assess for a dose-response relationship between malnutrition and externalizing behavior, each subject for whom behavior data were available was categorized into one of four groups: no malnutrition (N=766 at age 8, N=807 at age 11, N=422 at age 17), one indicator of malnutrition (N=160 at age 8, N=172 at age 11, N=90 at age 17), two indicators (N=45 at age 8, N=50 at age 11, N=25 at age 17), or three indicators (N=10 at age 8, N=13 at age 11, N=4 at age 17). Because only two individuals had all four nutrition indicators, this category could not be included in the dose-response analyses. Children thought to have potentially significant medical problems of any kind (including malnutrition, scabies, and parasitic worm) were referred to appropriate agencies for treatment (30), but neither these referrals nor the treatment outcomes were recorded or coded.
Intelligence and Cognitive Ability at Ages 3 and 11
Age 3
Measures of total cognitive ability were derived from six subtests of the Boehm Test of Basic Concepts—Preschool Version (14, 31, 32), which assesses basic verbal and visual-spatial concepts that are fundamental for early school achievement. Full details of measurement, factor structure, reliability, and validity in this sample are given elsewhere (14, 31). Data were available for 1,260 subjects.
Age 11
Estimates of full-scale IQ were assessed at age 11 years by using seven subtests of the WISC (33). The similarities and digit span subtests were used to form an estimate of verbal IQ, while the block design, object assembly, coding, mazes, and picture completion subtests were used to form an estimate of performance IQ. Data were available on 1,260 subjects for the preceding three measures.
Psychosocial Adversity at Ages 3 and 11
The age 3 index of psychosocial adversity (14, 22) was based on nine psychosocial variables assessed by social workers who visited the homes of the children at age 3 years (see reference 34 for full details). The index was created along lines similar to those described by Rutter (35) and Moffitt (36). A total adversity score was created by adding one point for each of the following nine variables: father uneducated, mother uneducated, semiskilled or unskilled parental occupation, single parent status, separation from parents, large family size, poor health of mother, teenage mother, and overcrowded home. Complete data for this construct were available for 1,795 participants.
The age 11 psychosocial adversity index (14, 19, 22) was based on 14 variables assessed by social workers who visited the homes of the children at age 11 years. A total adversity score was created by adding one point for each of the following 14 variables: living in rented accommodation, house without electricity or water, child with neither good toys nor good books, no television, poor housing, father uneducated, mother uneducated, parent psychiatrically ill, parent physically ill, teenage mother (age 19 or younger when child was born), single parent status, separation from both parents, five or more siblings, and overcrowded home (five or more family members per room). Complete data were available on 1,272.
Externalizing Behavior Problems
Age 8
Externalizing behavior was assessed by teacher ratings with the Children’s Behavior Questionnaire (37); see earlier reports (14, 22, 38) for full details of reliability and validity. Briefly, a factor analysis of this scale produced a factor of “aggression-hyperactivity” (38), with the four-item aggression scale having an internal reliability (coefficient alpha) of 0.79 and the six-item hyperactivity scale having a reliability of 0.64. Complete data were available for 1,130 participants on the aggression measure and for 1,128 on the hyperactivity measure.
Age 11
Externalizing behavior was assessed from parental ratings using the three externalizing subscales (aggression, delinquency, hyperactivity) of the Child Behavior Checklist (39), with item content common across boys and girls (22). The internal reliability values (coefficient alpha) for the scales were as follows: 0.72 for aggression, 0.66 for delinquency, 0.57 for hyperactivity, and 0.84 for total externalizing problems. Construct validity data are provided elsewhere (22, 34). Data were available for 1,206 children.
Age 17
Externalizing behavior was assessed by parent and teacher ratings using the Revised Behavior Problem Checklist (40); full details of reliability and validity have presented elsewhere (14, 22). All four checklist subscales that reflect externalizing behavior problems were included in the analyses: conduct disorder, socialized aggression, excessive motor activity, and attention problems. Complete data were available for 608 subjects.
Representativeness of Groups
Complete data on both the malnutrition and externalizing behavior variables were available on 982 subjects at age 8, 1,044 at age 11, and 541 at age 17. Those with and without complete data at each age were compared on gender and ethnicity, variables that were available on all subjects at age 3. Results of these analyses are shown in Table 1. There was a statistically significant overrepresentation of Indians at all ages among the participants with complete data and an overrepresentation of boys at age 11. Consequently, ethnicity and gender were entered into the subsequent analyses in order to assess their roles as moderator effects or confounds.
Statistical Analyses
In the comparisons of the malnourished and normal groups, separate analyses were conducted for each of the three ages (8, 11, and 17 years). To test for overall effects of malnutrition on externalizing behavior problems, we conducted a multivariate analysis of variance (MANOVA) on all dependent variables for each age (e.g., hyperactivity, aggression, and delinquency at age 11). Univariate F tests were then used to assess which specific subcomponents of externalizing behavior were associated with malnutrition. IQ and social adversity at ages 3 and 11 were identified as potential mediators, i.e., variables accounting for a significant portion of the relationship between the predictor (malnutrition) and the outcome variable (externalizing behavior) (21). To test for the mediating effects of cognition and psychosocial adversity, these variables were each entered separately as covariates in the MANOVAs. Gender and ethnicity were identified as potential moderators, i.e., factors that may reduce or enhance the influence of malnutrition on externalizing behavior, as indicated by an interaction between the independent variable (malnutrition) and a factor (gender, ethnicity) (21). To assess for moderating effects of gender and ethnicity, we entered these variables as factors in the MANOVA alongside the nutrition grouping. Any interactions were broken down by stratifying on the moderator variable and conducting two-way MANOVAs to test for simple interactions (41). These in turn were broken down by tests of simple main effects. To test for a dose-response relationship between degree of malnutrition and degree of externalizing behavior problems, we constructed four levels of the grouping factor (none, one, two, and three malnutrition indicators), repeated the preceding MANOVAs and univariate ANOVAs, and conducted tests for linear trends to assess for a linear fit between degree of malnutrition and degree of externalizing behavior. Two-tailed tests of significance with an alpha set at 0.05 were used throughout.
Results
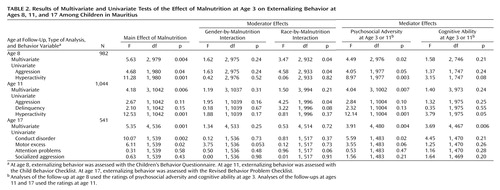
Detailed results of both the multivariate and univariate F tests of the effects of malnutrition on externalizing behavior at all three ages, including moderator and mediator effects, are shown in Table 2.
Externalizing Behavior Problems at Age 8
Effect of malnutrition
A MANOVA on the two dependent variables (aggression and hyperactivity) indicated a main group effect (Table 2), demonstrating that the malnourished children had higher overall externalizing behavior scores. Univariate F tests indicated that the malnourished group had significantly higher scores on both hyperactivity and aggression (Figure 1, Table 2).
Mediators
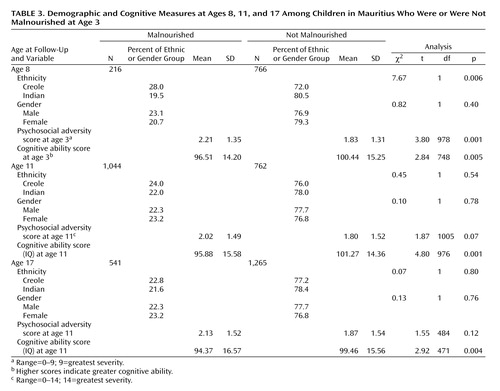
The malnourished children were more likely to have lower cognitive ability at age 3 than the normal children and were more likely to suffer psychosocial adversity at age 3 than the normal children (Table 3). Consequently, it is possible that poor cognition or greater psychosocial adversity could mediate the main effect of malnutrition on externalizing behavior. This possibility was tested by entering cognitive and adversity measures separately as covariates in the preceding MANOVA.
The main effect of malnutrition was abolished after we controlled for cognitive ability, indicating that cognitive ability mediates the link between malnutrition and externalizing behavior. In contrast, after we controlled for age 3 psychosocial adversity, the main effect of malnutrition remained significant (Table 2), indicating that the relationship between malnutrition and externalizing behavior was independent of psychosocial adversity.
Creoles were more likely to be malnourished than Indians (Table 3). After we controlled for ethnicity by entering it as a covariate, the effect of malnutrition on externalizing behavior remained significant (Table 2).
Moderators
There were no interactions between nutrition grouping and gender. However, there was a significant interaction between ethnicity and nutrition grouping. In order to clarify this two-way interaction, the sample was stratified by race and one-way MANOVAs were conducted separately on Creoles and Indians. The multivariate results indicated that in both groups, malnutrition was significantly associated with externalizing problems. For Creoles there was a significant effect of malnutrition on externalizing behavior (F=3.67, df=2, 236, p<0.03). Univariate F tests indicated that malnourished Creoles had significantly higher scores than normal Creoles on aggression (F=7.37, df=1, 237, p<0.008), but the effect for hyperactivity was not significant (F=2.92, df=1, 237, p=0.09). For Indians, there was a significant effect of malnutrition on externalizing behavior (F=3.43, df=2, 695, p<0.04), with higher scores for externalizing behavior among the malnourished Indians than among the normal Indians. Univariate F tests indicated that malnourished Indians had significantly higher scores than normal Indians on hyperactivity (F=4.85, df=1, 696, p<0.03), but the effect for aggression was not significant (F=0.15, df=1, 696, p=0.70). Consequently, these analyses indicate that malnutrition is more likely to predispose Creole children to aggression at age 8 but predispose Indian children to hyperactivity at age 8.
Externalizing Behavior Problems at Age 11
Effect of malnutrition
As shown in Table 2, the overall MANOVA indicated a main effect of malnutrition on externalizing behavior scores at age 11 years. The univariate F tests showed a significant effect of malnutrition on hyperactivity but not on aggression or delinquency (Figure 1).
Mediators
As shown in Table 3, the malnourished children had lower cognitive ability at age 11 than the nonmalnourished children. After we controlled for cognitive ability, the main effect of nutritional status was abolished, indicating a mediating effect of low cognitive ability. Although the malnourished and comparison children did not differ significantly on adverse psychosocial backgrounds at age 11, the difference approached significance. Consequently, to ensure that adversity did not mediate the findings, the age 11 total psychosocial adversity score was entered as a covariate in the preceding MANOVA. The main group effect remained significant.
Moderators
Multivariate results indicated that there were no significant moderator effects for gender at all ages and no moderator effects for ethnicity at ages 11 and 17, although ethnicity was a significant moderator at age 8 (Table 2).
Externalizing Behavior Problems at Age 17
Effect of malnutrition
A MANOVA conducted on conduct disorder, motor excess, attention problems, and socialized aggression showed a significant overall main effect of malnutrition (Table 2). Univariate F tests showed that the malnourished group had significantly higher scores on conduct disorder and motor excess but not on attention problems or socialized aggression (Figure 1, Table 2).
Mediators
After age 11 cognitive ability was entered as a covariate, the main effect of malnutrition remained significant. The main group effect also remained significant after we controlled for age 11 psychosocial adversity (Table 2).
Moderators
There was no significant moderator effect for gender or ethnicity (Table 2).
Dose-Response Relationships
Dose-response relationships between malnutrition and externalizing behavior are depicted in Figure 2. MANOVAs indicated a significant main effect of the degree of malnutrition on externalizing behavior at age 8 (F=2.53, df=6, 1954, p=0.02), and the linear term was also significant for both aggression (F=5.92, df=1, 977, p<0.02) and hyperactivity (F=11.96, df=1, 977, p<0.001). At age 17, there was also a main effect of the degree of malnutrition (F=2.44, df=12, 1608, p<0.004) and significant linear trends for conduct disorder (F=10.14, df=1, 537, p<0.002) and motor excess (F=8.58, df=1, 537, p<0.004). For age 11, the main effect of nutrition was nonsignificant (F=1.84, df=9, 3114, p=0.06), although the linear term was significant for hyperactivity (F=9.19, df=1, 1038, p<0.002). Univariate F tests showed significant group differences for age 8 hyperactivity (F=4.60, df=3, 977, p<0.003), age 11 hyperactivity (F=4.36, df=3, 1038, p<0.005), age 17 conduct disorder (F=3.53, df=3, 537, p<0.02), and age 17 motor excess (F=2.95, df=3, 537, p<0.04). The results of all other univariate tests (i.e., on aggression at age 8, aggression and delinquency at age 11, and attention problems and socialized aggression at age 17) were nonsignificant (p>0.11).
In order to assess whether poor cognition mediated the preceding dose-response relationships, the tests were repeated after we entered the cognitive measures as covariates. All effects of nutrition were abolished (age 8: F=1.14, df=6, 1488, p=0.34; age 17: F=1.69, df=12, 1401, p=0.07), indicating a mediating role of poor neurocognitive functioning.
Discussion
Key Findings
One key finding of this study is that malnutrition at age 3 years is associated with higher scores for externalizing behavior problems at ages 8, 11, and 17. A second key finding is that the relationship between malnutrition and externalizing behavior was not found to be an artifact of psychosocial adversity but was instead mediated by cognitive ability, indicating that malnutrition predisposes children to a lower IQ, which in turn predisposes them to externalizing behavior problems. These conclusions are supported by the finding of dose-response relationships between degree of malnutrition and degree of externalizing behavior problems at ages 8 and 17, relationships that were again found to be mediated by low IQ. To our knowledge, these are the first findings to show prospectively that malnutrition assessed in the early postnatal years is associated with externalizing behavior problems from childhood to late adolescence and also to show the mediating effects of cognitive ability. These findings in turn have potential implications for public health attempts to prevent the occurrence of externalizing behavior problems in children and adolescents.
The robustness of the findings is indicated in several ways. First, malnutrition predisposed to externalizing behavior problems across several ages from childhood (age 8) to late adolescence (age 17). Second, externalizing behavior problems were measured by three different instruments at the three different ages, indicating that the findings were replicated across sources and were largely invariant to the nature of measurement (42). Third, the fact that gender and ethnicity did not moderate the multivariate findings at ages 11 and 17 indicates that the nutrition-externalizing relationship is not specific to one gender or ethnic grouping, although it should be noted that at age 8 malnutrition was more likely to predispose to aggression in Creoles and to hyperactivity in Indians. It is possible that malnutrition predisposes to a general disinhibitory tendency and that broad cultural differences influence the precise manifestations of such disinhibition at a behavioral level. Fourth, the fact that dose-response relationships were found at ages 8 and 17 confirms and extends the findings based on comparisons of the malnourished and nonmalnourished children, although it is noted that the dose-response effect at age 11 was not statistically significant (p=0.06). For these reasons, we believe that the findings cannot be easily attributed to chance and that, instead, they reflect a reliable relationship between early malnutrition and later externalizing behavior problems.
Nutrition, Brain Development, and Externalizing Behavior
A critical question concerns the mechanism by which malnutrition predisposes to later externalizing behavior problems. We hypothesize that early malnutrition negatively affects brain growth and development and that brain impairments predispose to antisocial and violent behavior by affecting cognitive functions. The indicators of malnutrition in this study reflect deficits in protein (red hair, sparse/thin hair), iron (low hemoglobin level), and zinc (red hair, sparse/thin hair). There is extensive experimental evidence in animals both that zinc and protein deficiency impairs brain development (8, 43–45) and that protein, iron, and zinc deficiency predisposes to aggression (45–47). In humans, zinc deficiency during pregnancy has been linked to impaired DNA, RNA, and protein synthesis during brain development as well congenital brain abnormalities (48). There is also evidence in humans that antisocial behavior is related to protein deficiency (9) and iron-deficient anemia (7). Consequently, protein, iron, and zinc deficiencies may contribute to the brain impairments that have been found in aggressive adult offenders and that in turn are thought to predispose to aggressive antisocial behavior (3, 15, 46, 49).
While early malnutrition could thus relatively directly predispose to externalizing behavior problems by impairing brain mechanisms such as those in the prefrontal cortex that are thought to regulate emotion and inhibit impulsive aggressive behavior (for example, see reference 50), malnutrition could also predispose to externalizing behavior problems more indirectly by impairing cognitive functioning, which in turn predisposes to externalizing behavior problems. The findings from the present study provide partial (but not total) support for this possibility. Cognitive functioning was established as a mediator for the malnutrition-externalizing relationship at ages 8 and 11 years in that controlling for the effect of IQ on externalizing behavior abolished the malnutrition-externalizing relationship. Poor cognitive ability has been found consistently to predispose to externalizing behavior problems (51). Nevertheless, support for this cognitive explanation of the malnutrition-externalizing relationship is not entirely complete. While mediating effects were observed at ages 8 and 11 and while poor cognition mediated the dose-response relationship at age 17, it did not mediate overall differences between the malnourished and comparison groups in age 17 externalizing behavior, possibly because of the 6-year gap between the assessments of IQ (age 11) and externalizing behavior (age 17).
Clinical Implications and Limitations
Externalizing behavior problems are important predisposing factors in later adult violent offenses (52), and violence prevention and protection from victimization have become two of the most pressing issues facing society today (52, 53). One recent double-blind, placebo-controlled, randomized experimental trial showed that supplementation of adult prisoners’ diet with vitamins, minerals, and essential fatty acids significantly reduced antisocial and violent behavior in prison (54). Although dietary interventions for adults may prove helpful in reducing antisocial and violent behavior, identification of early risk factors for childhood and adolescent aggression is a critically important first step for developing successful prevention programs for such adult violence. Because nutrition is a malleable factor, it may be more practical and easier to prevent externalizing behavior through better early nutrition targeting at-risk populations than more complex and expensive psychosocial manipulations. The fact that several studies that have included the promotion of early nutrition as part of a larger prevention program have met with success (55, 56) argues for further attention to early malnutrition as a predisposing factor in externalizing behavior among children. It is possible, however, that malnutrition at age 3 years is correlated with poor prenatal malnutrition and that prenatal, rather than postnatal, interventions for malnutrition may be most effective (9, 55).
Finally, three potential limitations of the study should be acknowledged. First, the findings suggest but do not prove that early malnutrition predisposes to later externalizing behavior. Randomized, controlled designs that manipulate nutritional intake and evaluate diet in children are needed to support the role of nutrition as an etiological factor in externalizing behavior. Nevertheless, the fact that interventions that indirectly manipulate nutrition have been found to reduce later conduct disorder (55, 56) suggests that a possible etiological role of malnutrition in externalizing behavior should not be discounted. Second, because nutrition was assessed at only one time point (age 3 years) this study could not ascertain whether the effects on externalizing behavior were produced by transient malnutrition (i.e., the first 3 years only), by more sustained malnutrition, extending beyond the third year, or by maternal malnutrition during pregnancy (9). Third, there are cultural, ethnic, and social differences between Mauritius and the United States that highlight the importance of replicating the present findings in Europe and the United States. Nevertheless, the current findings from Mauritius may be a good model for externalizing problems in underserved subpopulations of American society, particularly since food insufficiency is relatively common in poor rural areas of the United States and has been associated with poor behavioral functioning in low-income children in American inner cities (57, 58).
 |
 |
 |
Received June 10, 2003; revision received Dec. 2, 2003; accepted Jan. 19, 2004. From the Social Science Research Institute and the Department of Psychology, University of Southern California; and the Department of Psychology, University of York, York, U.K. Address reprint requests to Dr. Raine, Department of Psychology, University of Southern California, Los Angeles, CA 90089-1061; [email protected] (e-mail). Supported by a predoctoral fellowship award (F31 NR-07518) and postdoctoral fellowship (F32 NR-08661) from the National Institute of Nursing Research to Dr. Liu; an NIMH Independent Scientist Award (K02 MH-01114), a grant from the Borchard Foundation, and a grant from NIMH (RO1 MH-46435) to Dr. Raine; grants from the Medical Research Council, Leverhulme Trust, and Mental Health Foundation to Dr. Venables; an NIMH Research Scientist Award to Dr. Mednick (5 K05 MH-00619); and a grant from the Ministry of Health of the Mauritian government. The authors thank Marie-Clare Calambay, Meena Calinghen, Athene Chiriaca, Cyril Dalais, Fazila Dinally, Devi Jaganathen, Goorah Rajah, and Charles Yip Tong for help in data collection and scoring.
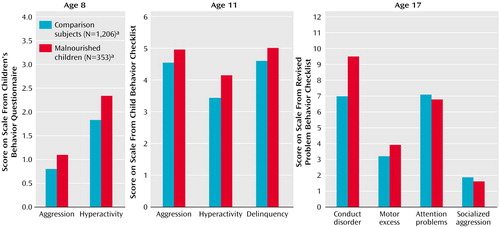
Figure 1. Scores for Externalizing Behaviors at Ages 8, 11, and 17 Among Children in Mauritius Who Were or Were Not Malnourished at Age 3
aNumber of subjects assessed at age 3.
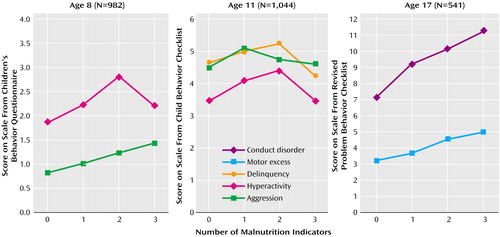
Figure 2. Dose-Response Relationships Between Number of Malnutrition Indicators at Age 3 and Externalizing Behaviors at Ages 8, 11, and 17 Among Children in Mauritiusa
aFour indicators of malnutrition were assessed: angular stomatitis, hair dyspigmentation, sparse/thin hair, and anemia.
1. Fishbein DH, Pease SE: Diet, nutrition, and aggression. J Offender Rehabilitation 1994; 21:117–144Crossref, Google Scholar
2. Rutter M, Giller H, Hagell A: Antisocial Behavior by Young People. New York, Cambridge University Press, 1998Google Scholar
3. Raine A: The Psychopathology of Crime: Criminal Behavior as a Clinical Disorder. San Diego, Academic Press, 1993Google Scholar
4. Kaplan JR, Muldoon MF, Manuck SB, Mann JJ: Assessing the observed relationship between low cholesterol and violence-related mortality: implications for suicide risk. Ann NY Acad Sci 1997; 836:57–80Crossref, Medline, Google Scholar
5. Breakey J: The role of diet and behaviour in childhood. J Paediatr Child Health 1997; 33:190–194Crossref, Medline, Google Scholar
6. Werbach MR: Nutritional influences on aggressive behavior. J Orthomolecular Med 1992; 7:45–51Google Scholar
7. Rosen GM, Deinard AS, Schwartz S, Smith C, Stephenson B, Grabenstein B: Iron deficiency among incarcerated juvenile delinquents. J Adolesc Health Care 1985; 6:419–423Crossref, Medline, Google Scholar
8. Peters DP: Effects of prenatal nutritional deficiency on affiliation and aggression in rats. Physiol Behav 1978; 20:359–362Crossref, Medline, Google Scholar
9. Neugebauer R, Hoek HW, Susser E: Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA 1999; 4:479–481Google Scholar
10. McGee R, Williams S, Anderson J, McKenzie-Parnell JM, Silva PA: Hyperactivity and serum and hair zinc levels in 11-year-old children from the general population. Biol Psychiatry 1990; 28:165–168Crossref, Medline, Google Scholar
11. Moffitt TE: Juvenile delinquency and attention-deficit disorder: developmental trajectories from age three to fifteen. Child Dev 1990; 61:893–910Crossref, Medline, Google Scholar
12. McCall RB, Beach SR, Lau S: The nature and correlates of underachievement among elementary schoolchildren in Hong Kong. Child Dev 2000; 71:785–801Crossref, Medline, Google Scholar
13. Noterdaeme M, Amorosa H: Evaluation of emotional and behavioral problems in language impaired children using the Child Behavior Checklist. Eur Child Adolesc Psychiatry 1999; 8:71–77Crossref, Medline, Google Scholar
14. Raine A, Yaralian P, Reynolds C, Venables P, Mednick S: Spatial but not verbal cognitive deficits at age 3 years in persistently antisocial individuals. Dev Psychopathol 2002; 14:25–44Crossref, Medline, Google Scholar
15. Moffitt TE: The neuropsychological studies of juvenile delinquency: a critical review, in Crime and Justice: An Annual Review of Research, vol 12. Edited by Tonry M, Morris N. Chicago, University of Chicago Press, 1990, pp 99–169Google Scholar
16. Fishbein DHE: Biobehavioral Perspectives in Criminology: Wadsworth Series in Criminological Theory. Belmont, Calif, Wadsworth/Thomson Learning, 2001Google Scholar
17. Grantham-McGregor S, Ani C: A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr 2001; 131 (2 suppl 2):649S-666SGoogle Scholar
18. Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW: Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 2000; 105:E51Google Scholar
19. Liu J, Raine A, Venables PH, Dalais C, Mednick SA.: Malnutrition at age 3 years and lower cognitive ability at age 11 years: independence from psychosocial adversity. Arch Pediatr Adolesc Med 2003; 157:593–600Crossref, Medline, Google Scholar
20. Grantham-McGregor SM, Walker SP, Chang S: Nutritional deficiencies and later behavioural development. Proc Nutr Soc 2000; 59:47–54Crossref, Medline, Google Scholar
21. Baron RM, Kenny DA: The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986; 51:1173–1182Crossref, Medline, Google Scholar
22. Raine A, Reynolds C, Venables PH, Mednick SA, Farrington DP: Fearlessness, stimulation-seeking, and large body size at age 3 years as early predispositions to childhood aggression at age 11 years. Arch Gen Psychiatry 1998; 55:745–751Crossref, Medline, Google Scholar
23. Declaration of Helsinki: Recommendations Guiding Doctors in Clinical Research Adopted by the 18th World Medical Assembly. Helsinki, World Medical Association, 1964Google Scholar
24. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research: The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Biomedical and Behavioral Research. Washington, DC, US Department of Health and Human Services, 1979Google Scholar
25. Wong DL, Hess CS: Clinical Manual of Pediatric Nursing. St Louis, Mosby, 2000Google Scholar
26. van den Biggelaar I, van den Broeck J: Nutrition-related hair signs in Zairian preschool children and associations with anthropometry. Trop Geogr Med 1995; 47:248–251Medline, Google Scholar
27. Rushton DH: Nutrition factors and hair loss. Clin Exp Dermatol 2002; 27:396–404Crossref, Medline, Google Scholar
28. Friedman M, Orraca-Tetteh R: Hair as an index of protein malnutrition. Adv Exp Med Biol 1978; 105:131–154Crossref, Medline, Google Scholar
29. Spencer LV, Callen JP: Hair loss in systemic disease. Dermatol Clin 1987; 5:565–570Crossref, Medline, Google Scholar
30. Bell B: A longitudinal psychophysiological study of 3-year-old Mauritian children: the Joint Child Health Project, in Primary Prevention of Schizophrenia in High-Risk Groups: Report on a Working Group, 9–12 June, 1975. Copenhagen, World Health Organization, 1977Google Scholar
31. Boehm A: Boehm Test of Basic Concepts—Preschool Version. San Antonio, Tex, Psychological Corp, 1986Google Scholar
32. Raine A, Reynolds C, Venables PH, Mednick SA: Stimulation seeking and intelligence: a prospective longitudinal study. J Pers Soc Psychol 2002; 82:663–674Crossref, Medline, Google Scholar
33. Wechsler D: Wechsler Preschool and Primary Scale of Intelligence. San Antonio, Tex, Psychological Corp, 1967Google Scholar
34. Raine A, Venables PH, Mednick SA: Low resting heart rate at age 3 years predisposes to aggression at age 11 years: evidence from the Mauritius Child Health Project. J Am Acad Child Adolesc Psychiatry 1997; 36:1457–1464Crossref, Medline, Google Scholar
35. Rutter M: Family, area, and school influences in the genesis of conduct disorder, in Aggression and Anti-Social Behavior in Childhood and Adolescence. Edited by Hersov LA, Shaffer D. Oxford, UK, Pergamon Press, 1978, pp 95–114Google Scholar
36. Moffitt TE: Juvenile delinquency and attention-deficit disorder: developmental trajectories from age three to fifteen. Child Dev 1990; 61:893–910Crossref, Medline, Google Scholar
37. Rutter M: A children’s behaviour questionnaire for completion by teachers: preliminary findings. J Child Psychol Psychiatry 1967; 8:1–11Crossref, Medline, Google Scholar
38. Venables PH, Fletcher RP, Dalais JC, Mitchell DA, Schulsinger F, Mednick SA: Factor structure of the Rutter Children’s Behavior Questionnaire in a primary school population in a developing country. J Child Psychol Psychiatry 1983; 24:213–222Crossref, Medline, Google Scholar
39. Achenbach TM, Edelbrock C: Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, University of Vermont, Department of Psychiatry, 1983Google Scholar
40. Quay HC, Peterson DR: Manual for the Revised Behavior Problem Checklist. Coral Gables, Fla, University of Miami, Department of Psychology, 1987Google Scholar
41. Maxwell SE, Delaney HD: Designing Experiments and Analyzing Data: A Model Comparison Approach. Belmont, Calif, Wadsworth, 1990Google Scholar
42. Moffitt TE: Measuring children’s antisocial behavior. JAMA 1996; 275:403–404Crossref, Medline, Google Scholar
43. Oteiza PI, Hurley L, Lonnerdal B, Keen C: Effects of marginal zinc deficiency on microtubule polymerization in the developing rat brain. Biol Trace Elem Res 1990; 23:13–23Crossref, Google Scholar
44. Bennis-Taleb N, Remacle C, Hoet JJ, Reusens B: A low-protein isocaloric diet during gestation affects brain development and alters permanently cerebral cortex blood vessels in rat offspring. J Nutr 1999; 129:1613–1619Crossref, Medline, Google Scholar
45. Halas ES, Reynolds GM, Sandstead HH: Intra-uterine nutrition and its effects on aggression. Physiol Behav 1977; 19:653–661Crossref, Medline, Google Scholar
46. Tikal K, Benesova O, Frankova S: The effect of pyrithioxine and pyridoxine on individual behavior, social interactions, and learning in rats malnourished in early postnatal life. Psychopharmacologia 1976; 46:325–332Crossref, Medline, Google Scholar
47. Munro N: A three year study of iron deficiency and behavior in rhesus monkeys. Int J Biosoc Res 1987; 9:35–62Google Scholar
48. Pfeiffer CC, Braverman ER: Zinc, the brain and behavior. Biol Psychiatry 1982; 17:513–532Medline, Google Scholar
49. Volavka J: Electroencephalogram among criminals, in The Causes of Crime: New Biological Approaches. Edited by Mednick SA, Moffitt TE, Stack S. Cambridge, UK, Cambridge University Press, 1987, pp 137–145Google Scholar
50. Raine A, Lencz T, Bihrle S, LaCasse L, Colletti P: Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch Gen Psychiatry 2000; 57:119–127Crossref, Medline, Google Scholar
51. Donnellan MB, Ge X, Wenk E: Cognitive abilities in adolescent-limited and life-course-persistent criminal offenders. J Abnorm Psychol 2000; 109:396–402Crossref, Medline, Google Scholar
52. Farrington DP, Hawkins JD: Predicting participation, early onset and later persistence in officially recorded offending. Crim Behav Ment Health 1991; 1:1–33Crossref, Google Scholar
53. Comerci GD: Efforts by the American Academy of Pediatrics to prevent and reduce violence and its effects on children and adolescents. Bull NY Acad Med 1996; 73:398–410Medline, Google Scholar
54. Gesch CB, Hammond SM, Hampson SE, Eves A, Crowder MJ: Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behaviour of young adult prisoners: randomised, placebo-controlled trial. Br J Psychiatry 2002; 181:22–28Crossref, Medline, Google Scholar
55. Olds D, Henderson CJ, Cole R, Eckenrode J, Kitzman H, Luckey D, Pettitt L, Sidora K, Morris P, Powers J: Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. JAMA 1998; 280:1238–1244Crossref, Medline, Google Scholar
56. Lally JR, Mangione PL, Honig AS: The Syracuse University Family Development Research Program: long-range impact of an early intervention with low income children and their families, in Parent Education as Early Childhood Intervention: Emerging Directions in Theory, Research, and Practice. Edited by Powell DR, Sigel IE. Norwood, NJ, Ablex Publishing Corp, 1988, pp 79–104Google Scholar
57. Murphy JM, Wehler CA, Pagano ME, Little M, Kleinman RE, Jellinek MS: Relationship between hunger and psychosocial functioning in low-income American children. J Am Acad Child Adolesc Psychiatry 1998; 37:163–170Crossref, Medline, Google Scholar
58. Smith J, Lensing S, Horton JA, Lovejoy J, Zaghloul S, Forrester I, McGee BB, Bogle ML: Prevalence of self-reported nutrition-related health problems in the Lower Mississippi Delta. Am J Public Health 1999; 89:1418–1421Crossref, Medline, Google Scholar



