Relationship of Birth Cohort and Early Age at Onset of Illness in a Bipolar Disorder Case Registry
Abstract
OBJECTIVE: Utilizing data from a previously characterized registry of subjects with bipolar illness, the authors examined age at onset of the first illness episode in cohorts of subjects born from 1900 through 1939 and from 1940 through 1959. METHOD: Demographic and clinical characteristics at the first full episode of bipolar disorder of subjects in a diagnostically validated voluntary bipolar disorder registry (N=1,218) were reviewed and subjected to statistical analyses. RESULTS: The median age at onset of the first episode of bipolar illness was lower by 4.5 years in subjects born during or after 1940 (median age=19 years), compared with subjects born before 1940 (median age=23.5 years). The proportion of subjects with bipolar disorder presenting with a prepubertal onset was significantly higher in the later birth-year cohort than in the earlier birth-year cohort. More than 50% of male and female subjects in both cohorts had a depressive episode as the first episode of bipolar illness. Subjects in each cohort who had a parent with major depression, bipolar disorder, or schizophrenia experienced their first episode nearly 4 to 5 years earlier than the other subjects in the cohort. CONCLUSIONS: Prospective epidemiological studies conducted with bipolar disorder subjects are needed to either affirm or refute these data on age at illness onset. If the results are affirmed, the early recognition of prepubertal bipolar disorder will be important, so that the condition can be treated with appropriate medications and medications that could potentially worsen the illness course can be avoided. Similarly, early recognition of bipolar illness is important, especially in women, to minimize use of antidepressant monotherapy for patients with bipolar illness. Among young people presenting with major depression as the first illness episode, a parental history of major depression, bipolar disorder, or psychosis may be a useful pointer to future bipolar disorder. Early recognition and appropriate treatment of bipolar illness may prevent the development of chronicity and serious functional impairment.
Age at onset for any illness may be a marker of etiologic and genetic heterogeneity. For this reason, the study of age at onset has been useful in evaluating phenotypes of a disorder to assist in diagnosis, in determining the etiology or prognosis of the disorder, and possibly in preventing and treating the disorder.
Some epidemiological reports have indicated that subjects with bipolar illness born in 1940 or later (hereafter referred to as subjects born after 1940) have an earlier age at onset (1, 2) than those born before 1940. In pooled data from 22 studies conducted from 1907 to 1988, a weighted mean of 28.1 years for the age at onset of bipolar illness was found (3). The Epidemiologic Catchment Area (ECA) study, conducted from 1978 to 1985, noted that the mean age at onset for patients with bipolar I disorder was 18 years (4, 5). Until recently, a diagnosis of prepubertal mania was relatively rare, but the frequency of this diagnosis appears to have increased rather quickly.
The evaluation of age at the first episode of bipolar illness may be particularly important for several clinical reasons. One issue is whether attention deficit hyperactivity disorder (ADHD) is comorbid with prepubertal bipolar disorder or whether ADHD is sometimes misdiagnosed as bipolar disorder (6–8). Investigators have suggested that the prevalence of prepubertal bipolar illness in the United States is different from that in the Netherlands (9). In addition, clinicians have expressed concern about the widespread use of stimulants and the newer antidepressants in prepubertal children and adolescents, some of whom may develop bipolar illness later in life (9–11). An interesting question is whether the use of such medications in children and adolescents changes the course of bipolar illness for the worse. Finally, recent surveys conducted by the National Depressive and Manic Depressive Association in the United States have suggested that more than one-third of participants waited more than 10 years for an accurate diagnosis (12).
We report data from the Stanley Center Bipolar Registry, a voluntary case registry that includes a relatively large number of self-identified subjects with bipolar disorder and provides details of the first illness episode for the majority of subjects. Data were obtained for subjects added to the registry in 1995–1999. Details about recruitment of subjects to the Stanley Center Bipolar Registry and the demographic and clinical characteristics of the registry participants whose data were used in this study have been reported elsewhere (13).
We used this data set to examine the following questions about age at onset of the first episode of bipolar illness:
| 1. | Was the cohort effect (i.e., an earlier age at onset reported by subjects born after 1940) still evident for age at onset in bipolar disorder subjects toward the end of the 20th century? | ||||
| 2. | Was there evidence to support the clinical impression that age at onset of the first episode had decreased even further in recent years (i.e., to encompass prepubertal onset) in the cohort born after 1940? | ||||
| 3. | Were there gender differences in age at onset of the first episode for the cohort born either before or after 1940? | ||||
| 4. | Were there differences between the two birth-year cohorts in whether the first episode manifested as major depression, mania, or a mixed state (symptoms of both major depression and mania experienced during the same episode)? | ||||
| 5. | Were there differences between men and women in the two birth-year cohorts in whether the first episode manifested as major depression, mania, or a mixed state? | ||||
| 6. | Did age at onset differ in bipolar disorder subjects if either parent had major depression, bipolar disorder, or schizophrenia, either in the entire sample or separately in each birth-year cohort? | ||||
Method
Sample Recruitment and Ascertainment of the First Episode of Illness
As detailed descriptions of the recruitment for and diagnostic validation of the Stanley Center Bipolar Registry have been reported elsewhere (13, 14), only a brief description will be provided in this report. Persons self-identified with bipolar disorders were recruited through Stanley Center staff presentations at patient and family organization meetings and at meetings with health care professionals (in community mental health clinics, office-based psychiatry practices, general hospitals with psychiatric services, university psychiatric departments, and state psychiatric hospitals); newspaper, radio, and television advertisements; and an Internet web site. The period of recruitment extended from 1995 to 1999. Subjects who signed an informed consent document (approved by the University of Pittsburgh Institutional Review Board) completed an interviewer-administered and -directed questionnaire over the phone. Demographic, clinical, and treatment characteristics, including details of the first illness episode, were obtained. For the most part, the self-identification of the subjects with bipolar disorder was based on their having been given the diagnosis by a psychiatrist. It is pertinent that the diagnostic validity of these self-identified bipolar disorder subjects was verified in a subset of 100 randomly selected individuals who were assessed by trained master’s- or doctoral-level psychiatric clinicians in a face-to-face interview with the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID) (15). These SCID diagnoses were verified by a supervising psychiatrist, the first author, or a senior research coordinator. Ninety-three percent of these subjects met the criteria for a DSM-IV bipolar disorder (14), which affirmed that the majority of self-identified bipolar disorder subjects accurately reported their diagnosis.
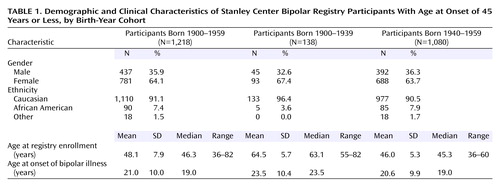
The analyses presented in this report are based on data for the 2,839 registry participants living within a 150-mile radius of the Pittsburgh metropolitan region (13) because the diagnostic validity study was conducted for this group only (14). The sample was further limited to 2,308 participants for whom data on the first illness episode were obtained (Figure 1). Among those self-identified as having a diagnosis of bipolar disorder in this sample, only five subjects reported hypomania without mania (bipolar II disorder). Thus, the sample was almost exclusively made up of subjects with a diagnosis of bipolar I disorder. Finally, the sample was further reduced to 1,280 subjects born in the years 1900–1959. The questions in this study focused on a younger age at onset, and as the median and mean age of the younger cohort was just over 45 years, it was decided that only those subjects whose age at onset of the first episode was 45 years or less would be included. Consequently, the entire sample was reduced to 1,218 subjects. This last step also addressed the concern that the younger cohort would have no subjects in their sixth decade or older. Specific information regarding manifestation of the first full episode as major depression, mania, or a mixed state was ascertained. Questions based on symptom checklists from the DSM-IV diagnostic criteria were used to characterize the episodes as hypomanic, manic, mixed, or depressive. In addition to questions about the type of episode and when it was first noted, questions about living arrangements, marital and employment status, and types of treatment received, including hospitalization, were reviewed with each of the subjects. The responses were probed in some detail to elicit a description of the full first episode of bipolar disorder.
For the majority of the analyses, the subjects were reported as belonging to an earlier birth cohort (those born from 1900 through 1939) or a later birth cohort (those born from 1940 through 1959). The rationale for excluding those born in 1960 or later was that the follow-up time would have been inadequate for expression of the illness. A further important point was that earlier and not later age at onset of the first episode was the focus of this study. Later age at onset could not reliably be estimated for the younger age cohort.
In theory, the ages of the subjects in the earlier birth cohort (those born from 1900 through 1939) who joined the registry between 1995 and 1999 could have ranged from a minimum of nearly 55 years to a maximum of 99 years. Thus, it is likely that the majority of those subjects had experienced full expression of the illness.
The age range of the subjects in the later birth cohort (those born from 1940 through 1959) who joined the registry between 1995 and 1999 could have ranged from a minimum of nearly 35 years to a maximum of 60 years. As the median age of the cohort was just over 45 years, the age-at-onset data beyond age 45 years would be less reliable in this cohort, although earlier age-at-onset data would be more reliable. Most of the questions we had raised for these analyses were in fact directed at an earlier and not a later age at onset.
To determine whether age at onset of the first episode had decreased especially in recent years in the cohort born after 1940, data from a separate group of subjects born from 1960 through 1969 were analyzed. The rationale for using data from this group was that the youngest member of the cohort born from 1960 through 1969 who joined the registry in 1995 would have been nearly 25 years old. Because this entire cohort would have passed through the age period for prepubertal onset, data from this group could be used to address questions about prepubertal onset. As these subjects would not have been in follow-up long enough, we did not consider it appropriate to use data from them to answer the other questions relating to age at onset in this report.
Recall Bias
Retrospective reporting of age at onset could have been affected by faulty memory in registry participants. We tried to address this potential bias separately for the earlier and later birth cohorts. In the interviewer-administered clinical questionnaire, questions on current age and date of birth were asked within the first three questions of the interview. Halfway through the interview (after a mean of 25 minutes), two specific questions relating to the first episode were asked. The first was, “How old were you when you had your first episode of what you now know to be either mania or mixed state or depression?” The follow-up question was “What month and year did this episode begin?” To assess the accuracy of the recall, we evaluated the concordance of responses to these two questions asked halfway through the interview with the subject’s report of date of birth provided at the start of the interview. This method did not exclude systematic misreporting of age at onset by each cohort, but it did provide a way to evaluate faulty recall within a single interview. It also provided information about whether recall in the earlier birth-year cohort was markedly different from that in the later birth-year cohort, at least within the time frame of the interview.
As a second check of the consistency of recall, the age at first episode was evaluated by cross-checking the data entered from the SCID with the self-reported age at onset in the subset of subjects whose data were used in the diagnostic validation of the registry (14).
Results
Demographic characteristics and age at onset of the first illness episode for the two birth-year cohorts are presented in Table 1.
Data regarding the age at onset are presented as cumulative percentages in the two birth-year cohorts in Figure 2 and as frequency histograms for different age intervals in the entire sample in Figure 3 and in the two birth-year cohorts in Figure 4. The percentages of subjects in each cohort presenting with major depression, mania, or a mixed state at onset of illness are presented in Figure 5. As there were only five subjects of African American descent in the cohort born from 1900 through 1939, racial differences between the two cohorts for age at onset could not be reliably estimated.
Based on visual inspection of the distribution of the age-at-onset plots, it was determined that the data for age at onset were not normally distributed. Therefore, these data were subjected to square-root transformation before further analyses. As Table 1 shows, there was nearly a 3-year earlier mean age at onset of the first episode of bipolar illness in the 1940–1959 birth cohort, compared with the 1900–1939 cohort (t=2.97, df=1,216, p<0.004). The median age at onset of the first episode differed in the two birth-year cohorts by 4.5 years (Figure 2). The age at onset was correlated with the birth year in the entire cohort (r=0.16, N=1,218, p<0.0001). When this correlation was reviewed for the 1900–1939 birth cohort, it was not statistically significant (r=0.03, N=138, p=0.75), whereas there was a small but statistically significant correlation in the 1940–1959 cohort (r=0.08, N=1,080, p<0.009).
In the entire sample, more than 75% of the subjects had their first episode by age 29 years, with a peak between 15 to 19 years (Figure 3). The 1940–1959 cohort had a greater proportion of subjects (53%) with onset of the first episode before age 19 years (Figure 4), compared with the 1900–1939 cohort (37%) (χ2=11.44, df=1, p<0.001).
There was no statistically significant difference in the mean age at first episode between men and women in the entire sample (men: mean=21.5 years, SD=10.1; women: mean=20.6 years, SD=9.9) (t=1.55, df=1,216, p=0.12) and in each birth-year cohort.
The two cohorts were significantly different in the proportion of subjects who reported that their first episode was major depression, mania, and a mixed state (Figure 5). In the 1900–1939 cohort, the first episode was a depressive episode for 91 subjects (67%), a manic episode for 21 subjects (15%), and mixed for 24 subjects (18%), compared with 593 subjects (55%), 244 subjects (23%), and 231 subjects (22%), respectively, in the 1940–1959 cohort (χ2=6.66, df=2, p=0.04).
In the entire sample, the proportions of men and women presenting with a first episode of major depression, mania, or a mixed state were significantly different. Among women, the first episode was major depression for 457 subjects (59%), mania for 147 subjects (19%), and mixed for 168 subjects (22%), compared with 227 subjects (53%), 118 subjects (27%), and 87 subjects (25%), respectively, among men (χ2=11.12, df=2, p<0.0004).
Gender differences in the type of episode at onset were not evident in the 1900–1939 cohort. Among women, 65 subjects (71%) reported a first depressive episode, 13 subjects (14%) reported a manic episode, and 14 subjects (15%) reported a mixed episode, compared to 26 men (59%), eight men (18%), and 10 men (23%), respectively (χ2=1.86, df=2, p=0.39). In contrast, in the 1940–1959 cohort, 392 women (58%) reported major depression as the first episode, 134 women (20%) reported mania, and 154 women (22%) reported a mixed episode, whereas 201 men (52%) reported major depression, 110 men (28%) reported mania, and 77 men (20%) reported a mixed state (χ2=10.5, df=2, p<0.006).
Within each birth-year cohort, subjects who reported that either parent had a diagnosis of major depression, bipolar disorder, or schizophrenia had an earlier age at onset of the first episode than subjects without such a parental history (Figure 6). In the entire sample, the age at first episode for the 751 subjects with a parental psychiatric history was earlier (mean=19.4 years, SD=9.7, median=18.0 years) than that for the 467 subjects without such a parental history (mean=23.4 years, SD=10.0, median=22.0 years) (t=6.93, df=1,216, p<0.0001). In the 1900–1939 cohort, the mean age at illness onset among subjects with a parental psychiatric history was 21.3 years (SD=10.0), compared with 26.3 years (SD=10.2) for those without a parental psychiatric history (t=2.80, df=136, p<0.006). In the 1940–1959 cohort, the mean age at illness onset for subjects with a parental psychiatric history was 19.2 years (SD=9.6), compared with 23.0 years (SD=9.9) for those without such a history (t=6.23, df=1,078, p<0.0001).
To answer the question of whether age at onset has become even earlier (14 years of age or less, i.e., prepubertal onset) in recent years, comparisons were made not only between the two birth-year cohorts described earlier but with a separate cohort born during the years 1960–1969 (N=570). The proportions of subjects in the three birth-year cohorts who had their first illness episode at age 14 years or earlier were significantly different. In the 1900–1939 cohort, 28 subjects (15.6%) had their first episode by age 14 years, compared with 318 subjects (28.9%) in the 1940–1959 cohort and 196 subjects (36.7%) in the 1960–1969 cohort (χ2=30.29, df=2, p<0.0001). The odds ratio for onset of disorder by age 14 was 2.19 (95% confidence interval [CI]=1.43–3.35) for the 1940–1959 cohort and 3.12 (95% CI=2.02–4.84) for the 1960–1969 cohort, compared with the 1900–1939 cohort.
To evaluate faulty recall of the age at onset of the first illness episode, the calculated age at onset (by using the actual date of birth and the reported age at onset, requested halfway through the interview) was a mean of 6.0 months (SD=5.6) later than it should have been given the reported date of birth in the 1900–1939 cohort. In the 1940–1959 cohort, the age at onset was reported to be a mean of 3.0 months (SD=2.1) earlier than it should have been. Both of these differences were well within a 1-year time frame. Furthermore, the self-reported age at onset of the first episode (mean=22.4 years, SD=9.9) closely matched the age-at-onset data derived from the SCID (mean=22.5 years, SD=8.3). The minor difference was not statistically significant, and the correlation between the two assessments for the subset of subjects in both the registry and the SCID database was high and statistically significant (r=0.81, N=65, p<0.0001).
Discussion
Operational definitions of age at onset for psychiatric illnesses have varied from the first onset of symptoms to the first onset of a full episode of illness with functional impairment that may or may not have required treatment, including psychiatric hospitalization. Each of these definitions is clinically relevant and represents important landmarks in the course of the illness, but, nonetheless, discrepancies in the specifications of the definition of age at onset may easily shift the reported time for onset of illness from several months to nearly 10 years (16). The present data reflect the first full episode of bipolar illness.
Limitations of this report include the voluntary and retrospective nature of the bipolar disorder case registry, compared with a prospective epidemiological registry. However, the subjects’ ability to accurately self-identify their illness (14) and to give details about the first episode of their illness (13) and the limitation of recall bias to a range of a few months suggest that while these data may not be ideal, they still provide a reasonable estimate of age at onset of the first episode of bipolar illness.
What factors may account for these results? One important consideration is diagnosis. Has the diagnosis of bipolar illness become so much broader in recent times that the subjects with an earlier onset of illness would not have been classified as having bipolar disorder in the past? This explanation is possible, but it is not likely to fully account for the current findings. Such an explanation would be more likely if a significant proportion of the subjects’ diagnoses were bipolar spectrum disorders. However, this data set, as with many others used in assessment of age at onset, concentrated on bipolar I disorder. Nonetheless, it is pertinent that the earlier birth-year cohort may have been less likely to receive a bipolar disorder diagnosis in childhood or early adolescence, and this possibility constitutes a limitation of this study.
Many studies of age at onset are based on retrospective recall by subjects. Faulty recall may lead to either underreporting or inaccurate reporting of age at onset. Is it possible that faulty recall by both birth-year cohorts led to disparate reporting of age at onset of bipolar illness in this study? A systematic reporting of later age at onset by the earlier birth-year cohort (a phenomenon sometimes referred to as the “Little Bo-Peep” effect) could in fact be responsible for this reported difference. However, other authors who have evaluated age at onset using different methods have also noted an earlier age at onset in subjects born after 1940 (2, 4). Furthermore, although there were minor differences between the two cohorts in accuracy of recall of age at onset, these differences were well within the time frame of a few months. However, this faulty recall was evaluated within a single interview, which does not preclude the possibility of a systematic misreporting of age at onset that may have influenced the results presented in this paper. It is interesting to note that self-reported age at onset of the first episode in this report was close to that recorded in the subgroup of subjects interviewed with the SCID (14).
Another possibility is that assortative mating may be involved in earlier age at onset of bipolar illness. For instance, because of illness-associated factors, subjects with bipolar affective disorders may marry or cohabit, giving rise to the possibility that their offspring may express the illness sooner. The present data suggest that subjects in both cohorts were more likely to have a nearly 4–5-year earlier age at onset if either parent had major depression, bipolar disorder, or schizophrenia. However, in the absence of systematic data on genetic history, the present study cannot answer this question definitively. Similarly, these data cannot be used to examine the phenomenon of “anticipation” of illness in the offspring of parents with bipolar illness (17).
Is it possible that the earlier and more extensive use of antidepressants or stimulants in younger populations led to an earlier expression of bipolar illness? The present data cannot be used to examine this issue conclusively, although some reports in the literature have appeared to support this contention (9–11). In adults with a diagnosis of bipolar disorder, the use of imipramine as monotherapy in maintenance treatment was associated with a 53% rate of mania, compared to a 28% rate for those receiving the combination of lithium and imipramine (18). Findings from such data sets led to the clinical practice of combining a mood-stabilizing agent such as lithium with an antidepressant, if one were needed in the treatment of depression in bipolar disorder. Nonetheless, the issue of antidepressant- or stimulant-associated hypomania/mania or cycle acceleration remains controversial. The data for children and adolescents in this regard are even less clear.
What then are the implications of these data? First, prospective epidemiological studies of childhood and adolescent populations are needed to accurately estimate the prevalence and incidence of bipolar illness and either affirm or refute the clinical experience suggesting that this condition is not uncommon in childhood and adolescence. Also, it will be important to determine if rates of prepubertal mania differ significantly between the United States and other countries, as suggested by one report (9). Second, these data may have implications for treatment. For instance, the use of stimulant or antidepressant medications in children may need to be considered carefully, especially in those with an initial diagnosis of ADHD, depressive disorder, or obsessive-compulsive disorder who may eventually turn out to have bipolar illness. Careful delineation of family history for evidence of affective disorder or psychoses, symptoms of bipolar disorder, and psychotic depression may be clinically relevant for an accurate diagnosis for these young people. Third, recent survey data from the U.S. National Depressive and Manic Depressive Association have suggested a long delay before adults with bipolar illness receive a correct diagnosis (12), and the situation could possibly be worse for children and adolescents with this disorder (11). Fourth, the abuse of stimulant street drugs such as cocaine by adolescents could mask the onset of mania and further delay an accurate diagnosis of bipolar disorder. Further, as women (and men) are more likely to present with major depression as the first episode of bipolar disorder, it is both possible and likely that they may receive unimodal antidepressant trials initially and that this encounter could occur in a primary care setting. Therefore, it may be helpful for psychiatrists to educate and assist primary care physicians in screening for bipolar illness.
Finally, the data derived from the bipolar disorder registry (13) used in this study and from other studies (19, 20) suggest that an earlier onset of the first episode of bipolar illness is often associated with chronicity as well as serious functional impairment. A natural extension of this issue is whether delayed diagnosis (implying either the lack of treatment or inappropriate treatment) contributes to this functional impairment. For decades, it has been argued in medicine that rapid recognition and treatment of many illnesses result in better functional outcomes for patients. These data on age at onset of bipolar illness support a similar approach to recognition and treatment of these disorders.
 |
Received June 26, 2002; revision received Jan. 8, 2003; accepted Jan. 21, 2003. From Western Psychiatric Institute and Clinic and the University of Pittsburgh School of Medicine, Pittsburgh; and the Special Studies Center at Mayview State Hospital, Bridgeville, Pa. Address reprint requests to Dr. Chengappa, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, 3811 O’Hara St., Pittsburgh, PA 15213-2593; [email protected] (e-mail). Supported in part by the Theodore and Vada Stanley Foundation and the Bosin Memorial Fund of the Pittsburgh Foundation (Dr. Kupfer) and NIMH grants MH-30915 (Dr. Kupfer) and MH-29618 (Dr. Frank).
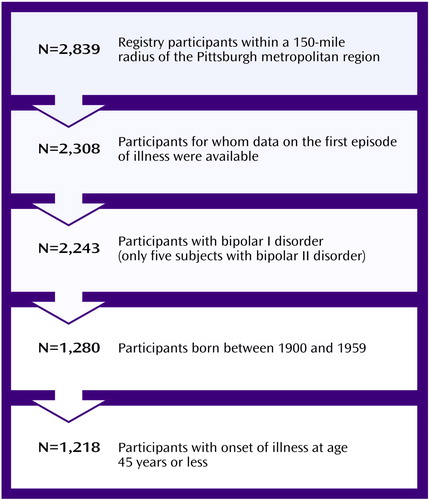
Figure 1. Selection of Stanley Center Bipolar Registry Participants for a Study of Age at Onset of the First Episode of Bipolar Illness
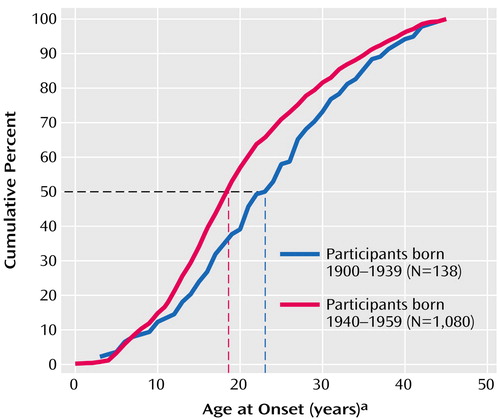
Figure 2. Age at Onset of the First Episode of Bipolar Illness of Stanley Center Bipolar Registry Participants in Two Birth-Year Cohorts
aDashed lines denote median age at onset in the birth cohorts.
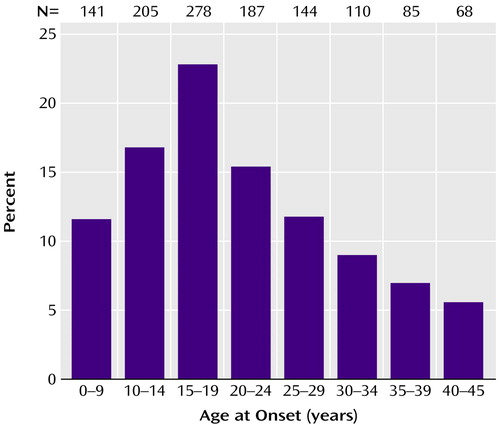
Figure 3. Age Interval at Onset of the First Episode of Bipolar Illness of Stanley Center Bipolar Registry Participants Born 1900–1959 (N=1,218)
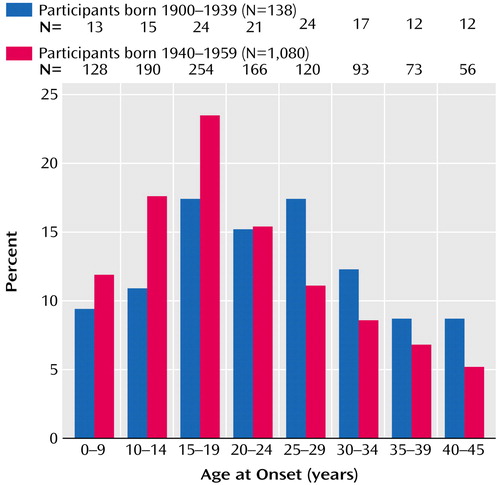
Figure 4. Age Interval at Onset of the First Episode of Bipolar Illness of Stanley Center Bipolar Registry Participants in Two Birth-Year Cohorts
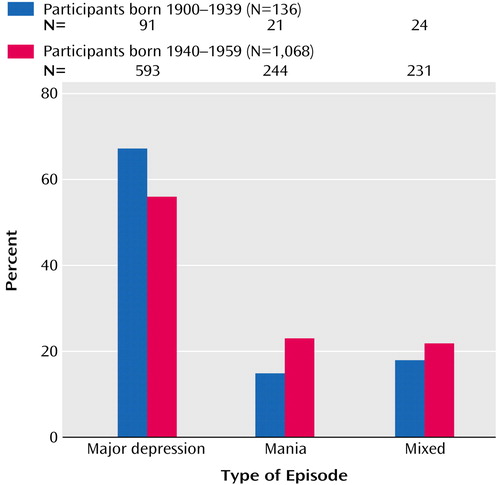
Figure 5. Type of Episode at Onset of Bipolar Illness in Stanley Center Bipolar Registry Participants in Two Birth-Year Cohorts
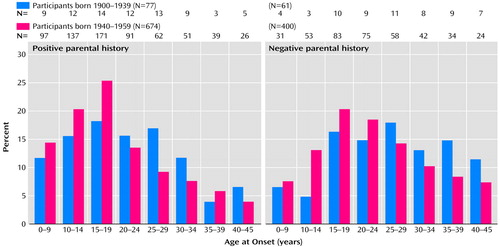
Figure 6. Age Interval at Onset of the First Episode of Bipolar Illness in Stanley Center Bipolar Registry Participants With and Without a Parental History of Psychiatric Disorder in Two Birth-Year Cohortsa
aParticipants were assessed for a parental history of major depression, bipolar disorder, or schizophrenia.
1. Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA: Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 1984; 41:949–958Crossref, Medline, Google Scholar
2. Gershon ES, Hamovit JH, Guroff JJ, Nurnberger JI: Birth-cohort changes in manic and depressive disorders in relatives of bipolar and schizoaffective patients. Arch Gen Psychiatry 1987; 44:314–319Crossref, Medline, Google Scholar
3. Goodwin FK, Jamison KR: Manic-Depressive Illness. New York, Oxford University Press, 1990Google Scholar
4. Christie KA, Burke JD Jr, Regier DA, Rae DS, Boyd JH, Locke BZ: Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. Am J Psychiatry 1988; 145:971–975Link, Google Scholar
5. Weissman MM, Leaf PJ, Tischler GL, Blazer DJ, Karno M, Bruce ML, Florio LP: Affective disorders in five United States communities. Psychol Med 1988; 18:141–153Crossref, Medline, Google Scholar
6. Biederman J: Resolved: mania is mistaken for ADHD in prepubertal children: affirmative. J Am Acad Child Adolesc Psychiatry 1998; 37:1091–1093Crossref, Medline, Google Scholar
7. Biederman J, Faraone S, Mick E, Wozniak J, Chen L, Ouellette C, Marrs A, Moore P, Garcia J, Mennin D, Lelon E: Attention-deficit hyperactivity disorder and juvenile mania: an overlooked comorbidity? J Am Acad Child Adolesc Psychiatry 1996; 35:997–1008Crossref, Medline, Google Scholar
8. Geller B, Williams M, Zimerman B, Frazier J, Beringer L, Warner KL: Prepubertal and early adolescent bipolarity differentiate from ADHD by manic symptoms, grandiose delusions, ultra-rapid or ultradian cycling. J Affect Disord 1998; 51:81–91Crossref, Medline, Google Scholar
9. Reichart CG: What are the risk factors for an early development of bipolar disorder in children? Bipolar Disord 2001; 3(suppl 1):15–16Google Scholar
10. Del Bello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM: Prior stimulant treatment in adolescents with bipolar disorder: association with age of onset. Bipolar Disord 2001; 3:53–57Crossref, Medline, Google Scholar
11. Wozniak J, Biederman J, Richards JA: Diagnostic and therapeutic dilemmas in the management of pediatric-onset bipolar disorder. J Clin Psychiatry 2001; 62(suppl 14):10–15Google Scholar
12. Hirschfeld RM, Lewis L, Vornik LA: Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry 2003; 64:161–174Crossref, Medline, Google Scholar
13. Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA: Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry 2002; 63:120–125Crossref, Medline, Google Scholar
14. Cluss PA, Marcus SC, Kelleher KJ, Thase ME, Aruay LA, Kupfer DJ: Diagnostic certainty of a voluntary bipolar disorder case registry. J Affect Disord 1999; 52:93–99Crossref, Medline, Google Scholar
15. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
16. Egeland JA, Hostetter AM, Pauls DL, Sussex JN: Prodromal symptoms before onset of mania depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000; 39:1245–1252Crossref, Medline, Google Scholar
17. Lange KJ, McInnis MG: Studies of anticipation in bipolar affective disorder. CNS Spectrums 2002; 7:196–202Crossref, Medline, Google Scholar
18. Prien RF, Kupfer DJ, Mansky PA, Small JG, Tuason VB, Voss CB, Johnson WE: Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders: report of the NIMH Collaborative Study Group comparing lithium carbonate, imipramine, and lithium carbonate-imipramine combination. Arch Gen Psychiatry 1984; 41:1096–1104Crossref, Medline, Google Scholar
19. Goldberg JF, Harrow M, Grossman LS: Course and outcome in bipolar affective disorder: a longitudinal follow-up study. Am J Psychiatry 1995; 152:379–384Link, Google Scholar
20. Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM: Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry 2000; 157:220–228Link, Google Scholar



