In This Issue
When Is Clozapine Right for Schizophrenia?
Clozapine is an antipsychotic medication generally reserved for patients whose schizophrenia is unresponsive to other antipsychotics. To help predict which patients will benefit from clozapine, Arango et al. (p. 1421) used a randomized comparison of clozapine and haloperidol to examine how treatment response relates to specific brain regions. The volume of gray matter in the right prefrontal cortex was related to symptom scores in different ways for clozapine and haloperidol: greater volume was associated with better response to clozapine but poorer response to haloperidol. The clozapine and haloperidol groups differed in the change in negative symptoms, akathisia, and anxiety/depression, suggesting that the worse response with haloperidol might be due to worse neurological side effects. Clozapine’s affinity for serotonin (5-HT) receptors may be the link between response and the prefrontal cortex, where 5-HT1A and 5-HT2A receptors are abundant.
Benzodiazepines Versus Guidelines for Panic Disorder
Recent guidelines for treating panic disorder recommend selective serotonin reuptake inhibitors (SSRIs) as the first approach. Over the last decade, however, SSRIs have not come close to supplanting benzodiazepines, according to Bruce et al. (p. 1432). Among 443 patients with panic disorder (with or without agoraphobia), reported use of SSRIs increased only from 13% to 33% between 1989 and 2001, and benzodiazepine use fell only slightly, from 64% to 58%. Most patients taking an SSRI were also taking a benzodiazepine, and only one-third of patients with coexisting major depression reported taking an SSRI. Why was there a nearly 2-to-1 advantage of benzodiazepines over SSRIs in recent years? Benzodiazepines act more quickly, SSRIs’ side effects may lead to noncompliance, and physicians may doubt or resist guidelines. Another important question is, Why were 31%–39% of the patients in this study receiving neither treatment?
How Autism Faces Emotion
People with autism have difficulty recognizing facial emotions, and brain activation is below normal in regions associated with face processing and emotion. Hall et al. (p. 1439) wondered whether turning up the emotional volume of the stimuli would increase recognition of emotions. They added expressive voices to pictures of faces displaying happiness, sadness, surprise, or anger. High-functioning men with autism matched emotions to these faces while regional cerebral blood flow was measured. These men made more errors than healthy men; the multimodal stimuli may have made their task even more difficult. Activation was greater than normal in the thalamus, anterior cingulate gyrus, and right anterior temporal pole. This pattern suggests that people with autism rely on selective analysis of features, emotional prototypes, and categorical knowledge, rather than on the assembly of an integrated emotional experience and holistic processing.
Teenagers’ Problems Around the World
Cultural differences can complicate measurement of mental distress in different countries. For teenagers the problem is compounded by rapid developmental changes. Verhulst et al. (p. 1479) examined scores on the Youth Self-Report for adolescents in Australia, China, Israel, Jamaica, the Netherlands, Turkey, and the United States. The score for total problems varied little. For the subgroup of externalizing problems (e.g., delinquent behavior) the score also showed little variation, but culture had a medium effect on the difference in internalizing problems (e.g., anxiety/depression). In the majority of cultures, scores increased with age. Each country’s scores for individual problems significantly correlated with scores of each other country. Cross-cultural variation was greatest for thought problems (e.g., “I see things that other people think aren’t there”) and smallest for aggressive behavior. Overall, the Youth Self-Report appears to be a simple, inexpensive means of assessing adolescents’ problems in diverse cultures.
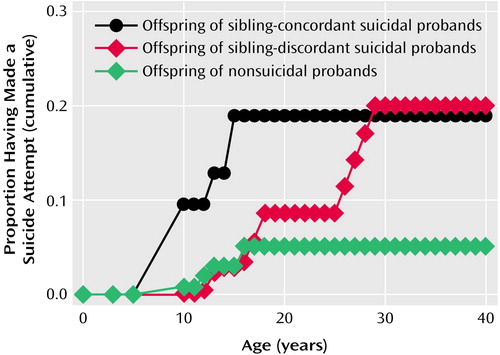
Second-Generation Suicide
Suicide and suicidal behavior are familial, but are they genetic? Brent et al. (p. 1486) examined suicide attempts in offspring with three degrees of family history. All three groups had parents with mood disorders; two had parents who had also attempted suicide. One set of attempter parents also each had a sibling who had attempted suicide. As expected, a stronger “dose” of family history was related to a higher risk of suicide attempts in the offspring. Impulsive aggression appeared to be a mediating factor: it was associated with a higher risk of suicide attempts and lower age at the first attempt, and it was highest in the families with the strongest history. Among both groups of offspring of parents who attempted suicide, the first attempt typically did less physical harm and demonstrated weaker suicidal intent than the parents’ attempts. In those with a strong family history of suicidal behavior, findings of mood disorders and impulsive aggression suggest targets for prevention and early intervention.
Images in Psychiatry
Ernest Jones, 1879–1958(p. 1395)

Ernest Jones, 1879–1958



