Mental Health
Abstract
OBJECTIVE: Only in the last 30 years has psychiatry begun to develop empirical approaches to conceptualizing and assessing positive mental health. Six models of mental health are reviewed here. METHOD: The author points out pitfalls in research on mental health, e.g., equating average with healthy, failing to distinguish trait from state, overlooking cultural norms, and conversely, blindly accepting the culture’s values. He describes the six models and provides history and research needs for each. RESULTS: The first model, being “above normal,” is epitomized by DSM-IV’s axis V, the Global Assessment of Functioning Scale. High scores represent “superior functioning in a wide range of activities, life’s problems never seem to get out of hand, is sought out by others because of his or her many positive qualities.” The goal of the second model, positive psychology, is intervention to maximize positive qualities, such as self-efficacy. Maturity and Erikson’s four developmental tasks (identity, intimacy, generativity, integrity) are the basis of the third model. The author adds two other tasks: career consolidation and “keeper of the meaning.” The fourth model is emotional or social intelligence, the ability to read other people’s emotions. Surprisingly, subjective well-being, the fifth model, is as much a characteristic of temperament as of a benign environment. The last model, resilience, is epitomized by DSM-IV’s Defense Function Scale, which categorizes coping mechanisms in terms of adaptational value. CONCLUSIONS: As with the blind men and the elephant, each model describes only some aspects of mental health. Further research may reveal the contribution of each.
We cannot even really know what causes neurotic suffering until we have an idea of what causes real health. This we have only begun to investigate.
Erik Erikson (1, p. 93)
Too often, psychiatry has been preoccupied only with mental illness. To paraphrase Mark Twain’s quip about the weather, psychiatry is always talking about mental health, but nobody ever does anything about it. Mental illness, after all, is a condition that can be reliably defined, and its limits are relatively clear. In contrast, mental health seems to lie more in the domain of value judgment than of science. For example, mental illness can be defined as the presence of selected symptoms, but mental health is something more than the absence of symptoms. With the notable exception of the chapter by Offer and Sabshin in the third and fourth editions of Comprehensive Textbook of Psychiatry(2), recent major psychiatric textbooks reveal virtually no serious discussion of positive mental health. An electronic search of Psychological Abstracts since 1987 turned up 57,800 articles on anxiety and 70,856 on depression, but only 5,701 mentioned life satisfaction and only 851 mentioned joy (3).
But mental health is too important to be ignored. In 1978 the report to the President by the President’s Commission on Mental Health (4) forcefully reiterated the importance of clearly defining what is meant by mental health, and over the last 30 years research has slowly moved the study of mental health from pious platitude toward science. Finally, 10 years ago, when evidence (5) emerged to support the validity of axis V (the Global Assessment of Functioning [GAF] Scale) in DSM-IV (p. 32), psychiatry actually possessed a metric for the measurement of mental health.
Previously, there had been an implicit assumption that mental health could be best defined as the antonym of mental illness, but accepting that assumption is to underestimate human potential. Starting early in the last century, internists, as they recognized that health was more than an absence of symptoms, began studying high-altitude physiology and developed measures of positive physical health for athletes, pilots, and finally astronauts. Thus, the antonym of physical illness is physical fitness. In the late 1930s, Arlie Bock, an internist trained in high-altitude physiology and interested in positive physical health, began at Harvard the Study of Adult Development, an interdisciplinary study of both positive mental and physical health (6, 7). The results of that study, lasting for 60 years (8), inform many facets of this paper.
It must be admitted that above average mental health is more difficult to define than physical fitness. Nevertheless, it is important for psychiatry to emulate sports medicine and to provide precise definitions and measures of positive mental health. Psychologists, like physiologists, have learned to quantify not only normal but better than average intelligence. Thus, we regard the antonym of mental retardation not as an IQ of 100 but as an IQ over 130. Psychiatry must follow suit. For rather than merely deciding who is too sick for a job, psychiatrists are called on to make decisions about who is mentally healthy enough for certain positions—such as air traffic controllers and submariners.
Before positive mental health can be defined, several cautionary steps are necessary. The first step in discussing mental health is to note that average is not the same as healthy, for average always includes mixing in with the healthy the prevalent amount of psychopathology. For example, in the general population the mean weight or eyesight is actually unhealthy, and if all sources of biopsychosocial pathology were excluded from the population, the average IQ would be significantly above 100. Put differently, being at the center of a normal bell curve of distribution may or may not be healthy. In the case of red blood cell count, body temperature, or mood, the middle of the bell curve is healthy. In the case of eyesight, exercise tolerance, or empathy, only the upper end of the bell curve is healthy; in the case of serum cholesterol, bilirubin, and narcissism, only the low end of the curve is healthy.
A second cautionary step in discussing mental health is to appreciate the caveat that what is healthy sometimes depends on geography, culture, and the historical moment. Punctuality is a virtue in some countries and a failing in others. General George Patton’s competitive temperament was a psychological liability in time of peace but a virtue in two world wars.
A third cautionary step is to make clear whether one is discussing trait or state. Who is physically healthier: an Olympic miler disabled by a simple but temporary (state) ankle fracture or a type 1 diabetic (trait) with a temporarily normal blood sugar level?
In defining mental health, the fourth and most important cautionary step is to appreciate the two-fold danger of “contamination by values.” On the one hand, cultural anthropology teaches us how parochial a given culture’s definition of mental health can be. And, even if mental health is “good,” what is it good for? The self or the society? For fitting in or for creativity? For happiness or survival? And who should be the judge? As Erikson warned, “The healthy personality is a topic approaching which the expert becomes a fearful angel” (1, p. 92).
On the other hand, common sense must prevail. Biology trumps anthropology. Every culture differs in its diet, but the World Health Organization would be in error to ignore the universal importance to diet of vitamins and of the four basic food groups. Although almost no form of behavior is considered abnormal in all cultures, that does not mean that the tolerated behavior is mentally healthy. Just because colonial America did not recognize alcoholism as an illness does not mean that alcoholism contributed less to 18th-century morbidity.
This article will contrast six different empirical approaches to mental health. It is significant that the empirical underpinnings for each of the six models have emerged only recently. First, mental health can be conceptualized as above normal, a mental state that is objectively desirable—as in the capacity to work and to love. Second, mental health can be conceptualized as positive psychology, an early example of which was Maslow’s “self-actualizing” individual (9). Third, from the viewpoint of healthy adult development, mental health can be conceptualized as maturity. Fourth, mental health can be conceptualized as emotional or social intelligence. Fifth, mental health can be conceptualized as subjective well-being—a mental state that is subjectively experienced as happy, contented, and desired. Finally, mental health can be conceptualized as resilience, as in successful adaptation and homeostasis. A moment’s reflection reveals that each of these models describes only part of the “elephant” of mental health. One research agenda must be empirically to decide, by means of multivariate modeling, which facets of each model are additive.
Model A: Mental Health as Above Normal
In 1835 Adolphe Quetelet published what appears to be the first important book on normality (10). Rather than focus on pathology, he tried “to approach more closely to what is good and beautiful” (p. x), and his goal was the statistical analysis of healthy humans. He challenged generations of future investigators with his introductory sentence, “Man is born, grows up, and dies, according to certain laws which have never been properly investigated” (p. 5).
Until World War II, however, Quetelet’s challenge to mental health professionals went largely unheeded. When in 1941 the U.S. draft board asked health professionals to define 1-A mental health, they were assigning a novel task. Indeed, it was not until after World War II that tentative works on normal adaptive behavior began to be published—White’s Lives in Progress(11), Srole and associates’ Mental Health in the Metropolis(12), Erikson’s “Growth and Crises of the ‘Healthy Personality’” (1), the Stirling County studies by the Leightons and colleagues (13, 14), and Grinker and Spiegel’s Men Under Stress(15). Such studies concentrated on the adaptation of nonpatient or normal populations but from different vantage points.
Nevertheless, many distinguished postwar psychiatrists continued to agree with Freud, who had dismissed mental health as “an ideal fiction.” In the late 1950s Lewis wrote, “Mental health is an invincibly obscure concept” (16, p. 227), and Redlich asserted, “We do not possess any general definition of normality and mental health from either a statistical or a clinical viewpoint” (17).
Shortly thereafter, Jahoda’s report to the Joint Commission on Mental Illness and Health led to a psychiatric sea change regarding the existence of mental health (18). As illustrated in Figure 1, Jahoda suggested that a mentally healthy individual should 1) be in touch with his or her own identity and feelings, 2) be oriented toward the future and remain fruitfully invested in life, 3) have a psyche that provides resistance to stress, 4) possess autonomy, perceive reality without distortion, and yet possess empathy, and 5) be able to work, to love, to play, and to be efficient in problem solving. Although the purpose of Jahoda’s report was to rid the term “mental health” of “vague, elusive and ambiguous connotation,” Jahoda could not marshal empirical evidence to prove that her plausible definition was more than platitude.
In the 1960s, beginning with Grinker and associates’ studies of “homoclites” (22) (physical education majors selected for normality) and Offer and Sabshin’s text on normality (19), investigators began to study mental health empirically. Although data from the Terman Study at Stanford (23), the Institute of Human Development at Berkeley (24, 25), and the Study of Adult Development at Harvard (7, 8) were later to be highly informative, the first longitudinal study of positive mental health to be harvested was arguably the elimination process by which out of 130 healthy jet pilots, already winnowed for over a decade for psychological resilience, the seven original astronauts were selected (26). This study underscored both the importance and the commonsensical nature of mental health. The final seven astronauts not only enjoyed exemplary work records but were also competent at loving. All had come from intact, happy, small-town families. In their 30s, they all were married with children. Although venturesome test pilots, they had suffered unusually few accidents during their years as pilots or even earlier. They could tolerate both close interdependent association and extreme isolation. They trusted others and were uncomplaining under discomfort. Emotions, both negative and positive, were strongly experienced. Not introspective, the astronauts seldom dwelled on their inner emotions; but they could describe them when asked. They were aware of the feelings of others, and they avoided interpersonal difficulties. Their group score on the neuroticism scale of the Maudsley Personality Inventory has been described as the lowest of any group reported in the literature (27).
A more influential early study of mental health was the Menninger Psychotherapy Project (28). To assess the psychological functioning of study subjects, Menninger psychologist Lester Luborsky devised an empirical measure of mental health (Health-Sickness Rating Scale), a scale of 0–100 (29, 30). In 1976, because Luborsky’s scale had been designed to evaluate candidates for psychotherapy rather than for general epidemiological studies, two of the architects of DSM-III modified the Health-Sickness Rating Scale and rechristened it the Global Assessment Scale (GAS) (31). The reliability values for between-rater agreement on each instrument and agreement between the two instruments were 0.85 to 0.95 (5). In a cross-cultural comparison Armelius and co-workers (32) noted that “the usefulness of the Health-Sickness Rating Scale as an international thermometer of mental health is strongly supported.” A modified version of the GAS was introduced in DSM-III-R as the GAF Scale, or axis V.
As with excellence in the decathlon, no single measure defines mental health, but all measures are highly intercorrelated. On the Health-Sickness Rating Scale a score of 95–100 reflects “an ideal state of complete functioning integration, of resiliency in the face of stress, of happiness and social effectiveness.” On the DSM-IV GAF Scale, a score of 91–100 equals “superior functioning in a wide range of activities, life’s problems never seem to get out of hand, is sought out by others because of his or her many positive qualities; no symptoms.” The words differ, but the melody is the same. Figure 1 illustrates how multifaceted and unique models of positive mental health can be and yet how strong their “family” resemblance.
Some items on a future research agenda seem clear. First, it behooves psychiatry to pursue cross-cultural validation and refinement of the GAF Scale. Second, since primary prevention is clearly superior to treating disease once it has occurred, we need to study individuals with positive mental health the way that agronomists study wheat that is resistant to drought and blight. Third, the concept of mental health raises the issue of therapeutic interventions to achieve it. Which facets of mental health are fixed and which are susceptible to change? By analogy, in most individuals the most intensive educational intervention will raise IQ only about 7 points, but sustained therapeutic intervention can change individuals utterly illiterate in Italian into fluent Italian conversationalists. With clozapine or with cognitive behavior therapy we can raise a GAF Scale score from 40 to 70, but how would we raise a score from 70 to 90? This is an important research question that psychiatry has not yet begun to address.
Model B: Mental Health as Positive Psychology
The second model, as old as Aristotle, conceives of mental health as a utopian ideal and has provided the impetus for the recent positive psychology movement (33). In the 19th century mental health was viewed as related to morality. Psychiatrists wrote of both “moral insanity” and “good character.” But in the 20th century, as psychiatry became more concerned with pathology, only educational psychology remained interested in character and “virtue.”
In psychology, interventions to improve already adequate intelligence and social skills are common, while in medicine and psychiatry to meddle with adequate thyroid function, a healthy hematocrit, or a normal mood is only to invite trouble. It can be argued that in the healthy rested individual virtually all psychopharmacological interventions will, over time, make the brain function worse; it can also be argued that many nonpharmacological interventions (e.g., literacy training, stress management, and tennis lessons) will make the brain function better. Thus, those with the medical goal of using medication to remove pathology sometimes forget educational interventions to enhance above average functioning.
Over the last 40 years, Maslow’s concept of self-actualization and his emphasis on humanistic psychology (9, 34) have drawn attention to full use and exploitation of talents, capacities, potentialities. But until very recently, such humanistic psychology did not provide empirical research and ignored both predictive validity and follow-up. As early as 1925, psychiatrist Adolf Meyer was already warning psychologists of the difference between “moralizing” about mental health and studying it by “conscientious and impartial study” and “constructive experimentation” (35, p. 118).
Recently, Seligman (36, 37) has served notice that positive psychology will follow Meyer’s rules of conscientious and impartial study and constructive experimentation. Seligman’s concept of learned optimism incorporates the empirical advances in cognitive psychology that have taken place over the past three decades. Creating a positive attributional style not only serves as a cognitive behavior treatment for depression (36, 37) but can lead to positive mental states.
Advocates of positive psychology wish to learn how to build the qualities that help individuals and communities not just to endure and survive but also to flourish. Formally introduced in the January 2000 issue of American Psychologist, positive psychology entails rendering “humanistic” psychology amenable to scientific study and intervention.
At the individual level, it is about positive individual traits; the capacity for love and vocation, courage, interpersonal skill, aesthetic sensibility, perseverance, forgiveness, originality, future mindedness, spirituality, high talent, and wisdom.… And in this quest for what is best, positive psychology does not rely on wishful thinking, faith, self-deception, fads, or hand waving; it tries to adapt what is best in the scientific method to the unique problems that human behavior presents to those who wish to understand it in all its complexity. (33, p. 5)
Recently, advocates of positive psychology have divided positive mental health into four components: talents, enablers, strengths, and outcomes (20). Talents are inborn, are genetic, and are not much affected by intervention (e.g., high IQ, being an easy baby). Enablers reflect social interventions and environmental good luck (e.g., strong family, good school system); these can be experimentally modified to enhance strengths. Strengths (Figure 1) are character traits such as curiosity and openness that reflect facets of mental health that are amenable to change. Outcomes reflect dependent variables (e.g., improved score on the GAF Scale, positive social relationships, subjective well-being) that can be used to provide evidence that clinicians’ efforts to alter strengths are not just wishful thinking.
As components of mental health, the specific ideal strengths (or virtues) are subject to debate. Wisdom, kindness, and the capacity to love and be loved are strengths over which few would argue. But should courage be included as a strength, and why were intelligence, perfect musical pitch, and punctuality excluded? The answer is that the 24 strengths listed in Figure 1 may be subjected to a variety of tests. First, they have been recurrent positive values across cultures and across centuries. Second, they may be valued in their own right and not just as a means to ends.
There are pitfalls with positive psychology. First, the perspective of mental health as Utopia is one of the bogeymen of national health policy makers. They are afraid, without directly expressing it, that this perspective, commonly adhered to by some mental health specialists, will put a backbreaking burden on health insurance. Is helping people to become happier with themselves a process that any health insurance program should be expected to cover? Over time society will have to decide who should pay for positive mental health: the individual, the educational system, third-party payers, religious organizations, or a combination of all four.
A second caution about positive psychology relates to the danger of the culturally insensitive prescription of parochial virtues. The dangers of value judgments are enormous. We need to distinguish virtues, even Aristotelian virtues, from health. Keeping wounds clean is healthy but not a virtue. Body hygiene in public places is a virtue but not necessarily healthy.
A third controversial facet of positive psychology is its emphasis on optimism. Since the late 19th century, many social scientists, especially those in Europe, have mistrusted optimistic cognition, especially religious optimism, as a maladaptive “American” illusion interfering with accurate perception of reality. Nietzsche, Freud, Marx, and Darwin all perceived optimism as evidence of an ingenuous cultural adolescence, not of mature mental health. It is healthier to face the hard facts of life. Besides, there is a significant body of work suggesting that the depressed perceive the world more accurately (38).
Nevertheless, over the past 30 years cognitive therapists have demonstrated that altered cognition can not only change behavior, it can also alter brain function (39). If pessimism is the dominant cognition of the depressed, optimism appears the dominant cognition of the mentally healthy. If learned helplessness leads to depression, learned optimism and self-efficacy lead to mental health (37).
In part, the importance of optimism to positive mental health depends on an explanatory style that asserts, “The good things that happen to me will last forever. They are pervasive, and they are my own doing. The bad things that happen to me occur by chance, are limited, and are unlikely to happen again.” The explanatory style of many chronically depressed individuals is just the opposite (40, 41). In addition, optimism includes hope, a facet of mental health as old as the Greek myth of Pandora. Yet hope is a topic to which psychiatry up to now has given little formal consideration. In addition, the illusion of optimism permits one to contemplate and plan for, rather than to deny, the future. Longitudinal studies have repeatedly shown future-mindedness to be a critical ingredient of mental health (7, 24). Finally, positive psychology is the only model of mental health that suggests, even tentatively, how a GAF Scale score of 75 might be raised to 90. The research agenda for positive psychology includes continuing to build bridges to medicine and to build on work (42) that undergirds such humanistic ideas with Meyer’s “constructive experimentation.”
Model C: Mental Health as Maturity
Unlike organs of the body that are designed to stay the same, the brain is designed to be plastic. A 10-year-old’s lungs and kidneys are more likely to reflect health than those of a 50-year-old, but that is not true of the central nervous system (CNS). To some extent, then, adult mental health reflects a continuing process of maturational unfolding.
It may be argued that the “brain” gets worse with age, so why should the “mind” get better? But research reveals that in the absence of disease the brain works surprisingly well until age 80 (43) and that neurologically optimal brain development requires almost a lifetime (44, 45). Prospective studies reveal that individuals are less depressed and show greater emotional modulation at 70 than they did at 30 (8, 25).
Erikson, influenced by his work at the Institute of Human Development, provided the first model of adult social development (1, 46). Although he devoted only four out of 55 pages to his three stages of adult development, he saw each of his eight developmental stages as a “criterion of mental health” (1, p. 142). Later, Jane Loevinger provided a model of adult ego development (47), Lawrence Kohlberg proposed a model of adult moral development (48), and James Fowler described a model of spiritual development (49). Implicit in all these models is the assumption that greater maturity reflects greater mental health. Perhaps the best definition of mental health that we have is William Menninger’s definition of maturity (21) (Figure 1). In this model maturity is not only the antonym of narcissism but is quite congruent with other models of mental health.
To confirm the hypothesis that maturity and positive mental health are almost synonymous, the study of the behavior and feeling states of persons over a lifetime becomes necessary. Although most such longitudinal studies have come to fruition relatively recently (7, 23, 25, 50, 51), all illustrate the association of increasing mental health with maturity. (After age 50, of course, the association between mental health and maturity is contingent on a healthy CNS. The ravages of brain trauma, major depression, arteriosclerosis, Alzheimer’s disease, alcoholism, and schizophrenia can all reverse the process.)
The association of mental health with maturity is probably mediated not only by progressive brain myelinization (44, 45) but also by the evolution of emotional and social intelligence over time. Erikson conceptualized such development as a “widening social radius.” In his view, life after age 50 is no longer a staircase leading downward, as in the Pennsylvania Dutch cartoons of life span development. Rather, Eriksonian development can be conceptualized as expanding ripples in a pond. Over time the adult social radius expands through the mastery of four tasks: identity versus identity diffusion, intimacy versus isolation, generativity versus stagnation, and integrity versus despair. On the basis of empirical data from Harvard’s Study of Adult Development, I have added two more tasks—career consolidation and “keeper of the meaning”—to Erikson’s four (52) (Figure 2) and demonstrated their sequential nature. Mastery of such tasks appears relatively independent of education, gender, social class, and arguably, culture (53).
In such a model the social radius of each adult developmental task fits inside the next. First, the adolescent must evolve an identity that allows him or her to become separate from the parents, for mental health and adult development cannot evolve through a false self. The task of identity requires mastering the last task of childhood: sustained separation from social, residential, economic, and ideological dependence on one’s family of origin. Such separation derives as much from the identification and internalization of important adolescent friends and mentors as it does from simple biologic maturation (54). For example, our accents become relatively fixed by age 16 and reflect those of our adolescent peer group rather than the accents of our parents.
Then adults develop intimacy, which permits them to become reciprocally, and not narcissistically, involved with a partner. To many young adults, to live with one other person in an interdependent, reciprocal, committed, and contented fashion for years and years may seem neither desirable nor possible. Once achieved, however, the capacity for intimacy may seem as effortless and desirable as riding a bicycle. Sometimes the relationship is with a person of the same gender; sometimes it is completely asexual; and sometimes, as in religious orders, the interdependence is with a community. In different cultures and epochs, mastery of intimacy has taken very different guises but “mating for life” and “marriage-type love” are tasks built into the developmental repertoires of many warm-blooded species, including our own.
Career consolidation is a task that is usually mastered together with or that follows the mastery of intimacy. Mastery of this task permits adults to find a career as valuable as they once found play. On a desert island one can have a hobby but not a career, for careers involve being of value to other people. There are four crucial developmental criteria that transform a job or hobby into a career: contentment, compensation, competence, and commitment. Not only people with schizophrenia but also individuals with severe personality disorder often manifest a lifelong inability to achieve either intimacy or sustained, gratifying employment. Such individuals rarely enjoy a GAF Scale score over 65.
Mastery of the fourth task, generativity, involves the demonstration of a clear capacity to unselfishly care for and guide the next generation. Existing research reveals that sometime between ages 35 and 55 our need for achievement declines and our need for community and affiliation increases (55). Depending on the opportunities that the society makes available, generativity can mean serving as a consultant, guide, mentor, or coach to young adults in the larger society. Generativity reflects the capacity to give the self—finally completed through mastery of the first three tasks of adult development—away. Its mastery is strongly correlated with subsequent mental health in old age (8). For in old age there are inevitable losses, and these may overwhelm us if we have not continued to grow beyond our immediate family.
The penultimate life task is to become a keeper of the meaning. Like grandparenthood, this task involves passing on the traditions of the past to the future. Generativity and its virtue, care, require taking care of one person rather than another. Keeper of the meaning and its virtues of wisdom and justice are less selective; for justice, unlike care, means not taking sides. The focus of a keeper of the meaning is with conservation and preservation of the collective products of mankind—the culture in which one lives and its institutions—rather than with just the development of its children. Clearly, caretakers and grandparents are not mentally healthier than caregivers and parents. The distinction is only that grandparents are usually better at the tasks of keeper of the meaning than are 30-year-olds.
Finally, in old age it is common to feel that some life exists after death and that one is part of something greater than one’s community. Thus, the last life task is integrity, the task of achieving some sense of peace and unity with respect to one’s own life. One’s social radius may expand to embrace the whole world. Erikson described integrity as an experience that conveys some world order and spiritual sense. “It is the acceptance of one’s one and only life cycle and of the people who have become significant to it as something that had to be and that, by necessity, permitted of no substitutions” (1, p. 143).
Of course, healthy adult development does not follow rigid rules, nor are butterflies healthier than caterpillars. Some individuals, often because of great stress, tackle developmental tasks out of order or all at once. Beethoven enjoyed a brilliant committed career but never enjoyed intimacy.
The research agenda for the maturational model is the same as for positive psychology—to provide such humanistic concepts of adult development with more operational, empirically grounded, prospectively derived, and cross-culturally validated definitions of maturational tasks and then to demonstrate their predictive validity.
Model D: Mental Health as Social-Emotional Intelligence
In the Nicomachean Ethics, Aristotle defined social-emotional intelligence as follows: “Anyone can become angry—that is easy. But to be angry with the right person, to the right degree, at the right time, for the right purpose, and in the right way—that is not easy.” Nevertheless, as recently as 40 years ago a textbook on intelligence dismissed the concept of social intelligence as “useless.” Indeed, only since the 1970s has modulation of “object relations” seemed more important to psychoanalysis than modulation of “instinct.”
The benefits of being able to read feelings from nonverbal cues have been demonstrated in almost a score of countries (56). These benefits include being better emotionally adjusted, more popular, and more responsive to others. Empathic children, without being more intelligent, do better in school and are more popular than their peers. Head Start found that early school success was achieved not by intelligence but by being able to wait and knowing what kind of behavior is expected, how to rein in the impulse to misbehave, and how to get on with other children (57).
Social-emotional intelligence can be defined by the following criteria (56):
| 1. | Accurate conscious perception and monitoring of one’s own emotions. | ||||
| 2. | Modification of one’s emotions so that their expression is appropriate. This involves the capacity to self-soothe anxiety and to shake off hopelessness and gloom. | ||||
| 3. | Accurate recognition of and response to emotions in others. | ||||
| 4. | Skill in negotiating close relationships with others. | ||||
| 5. | Capacity for focusing emotions (motivation) on a desired goal. This involves delayed gratification and adaptively displacing and channeling impulse. | ||||
Over the last 15 years, two important empirical steps have been taken in our understanding of the importance of social-emotional intelligence to positive mental health. The first step is that both functional magnetic resonance imaging (fMRI) and ingenious neurophysiological experimentation (58, 59) have led to advances in our understanding of the integration of the prefrontal cortex with the limbic system, especially with the amygdala and its connections. This in turn has brought us closer to understanding emotions as neurophysiological phenomena rather than as platonic abstractions.
The second step has been our slow but steady progress in conceptualizing and even measuring “emotional intelligence” (60). High emotional intelligence reflects above average mental health in the same way that a high IQ reflects above average intellectual aptitude. Gardner described emotional intelligence as the capacity to “discern and respond appropriately to the moods, temperaments, motivations and desires of other people” (61, p. 8).
Where the study of positive mental health ends and primary prevention begins is unclear, but like the model of positive psychology, the model of social-emotional intelligence is potentially interventionist. Just as we can have above average musical skill or physical coordination and yet can train these strengths to be even greater; so we are learning to enhance emotional intelligence. There are already exercises in teaching emotion recognition and differentiation to patients with eating disorders and teaching anger modulation and how to find creative solutions to social predicaments for individuals with behavior disorders. Once we have a firmer grasp of its measurement, the relative importance of emotional intelligence to other components of mental health can be assessed. I wager that it will emerge as the most important single dimension of mental health.
Model E: Mental Health as Subjective Well-Being
Is it better to meet some expert’s definition of mental health, or is it better to feel subjectively fulfilled? The answer is “both.” For positive mental health does not involve just being a joy to others; one must also experience subjective well-being. Indeed, long before humankind considered definitions of mental health, they pondered criteria for subjective happiness. “No man is happy who does not think himself so.”
Nevertheless, the mental health issues involved in subjective well-being are complicated and clouded by historical relativism, value judgment, and illusion. As already noted, Europeans have been skeptical of American concern with happiness. On the one hand, happiness that comes from joy or unselfish love (agape), that comes from self-control and self-efficacy, or that comes from play or deep but effortless involvement (62) reflects health. On the other hand, happiness can be based on illusion or on dissociative states, and the search for happiness can appear selfish, narcissistic, superficial, and banal. Examples of maladaptive “happiness” include the excitement of risk taking, being “high” on drugs, and short-lived satisfaction from binge eating, tantrums, promiscuity, and revenge. It is because of such ambiguity of meaning that throughout this section the term “subjective well-being” is substituted for “happiness.”
Only in the last decade have investigators such as Barbara Fredrickson (63), Martin Seligman (36), and David Snowdon (64) pointed out that a primary function of positive emotional states and optimism is facilitation of self-care. Subjective well-being makes available personal resources that can be directed toward innovation and creativity in thought and action. Thus, subjective well-being, like optimism, becomes an antidote to learned helplessness. Again, after control for income, education, weight, smoking, drinking, and disease, happy people are perhaps only half as likely to die at an early age or become disabled as unhappy people (65).
Until recently the scientific parameters of subjective well-being were as vague as those for objective mental health. A 1967 definition suggested that a happy person is “young, healthy, well-educated, well paid, extroverted, optimistic, worry free, religious and married with high self esteem, a good job, morals, and modest aspirations” (italics added) (66). In the last 30 years, however, empirical research has shown such a vacuous generalization only partly correct. The italicized adjectives are all untrue or true only with qualifications (37).
The Nuns Study provides perhaps the most convincing link between subjective happiness and health (64, 67). When they were in their 20s, 180 nuns were asked to write a 2–3-page autobiography. Of those who expressed the most positive emotion, only 24% had died by age 80. In contrast, by the same age 54% of those who expressed the least positive emotion had died.
Only in the last three decades have investigators, especially Edward Diener (3, 68), made a serious effort to research the definitional and causal parameters of subjective well-being and thereby address important questions. One such question is, Is subjective well-being more a function of environmental good fortune, or is it more a function of an inborn, genetically based temperament? Put differently, Does subjective well-being reflect trait or state? If subjective well-being reflects a safe environment and the absence of stress, it should fluctuate over time, and individuals happy in one domain in their lives might not be happy in another.
The answer is that subjective well-being has more effect on the environment than the environment exerts on it. For example, investigators have been startled that a significant number of AIDS victims perceive that their illness has enhanced the quality of their subjective lives. Similarly, after a few weeks of temporary elation, the subjective well-being of lottery winners returns to baseline.
In other words, subjective well-being is due more to “top-down” processes—temperamental factors governing subjective well-being—than to “bottom-up factors”—for example, the fulfillment of universal human needs. Indeed, subjective well-being is highly heritable and relatively independent of demographic variables. The subjective well-being of monozygous twins raised apart is more similar than that of heterozygous twins raised together (69). Among the partially heritable factors making significant contributions to a high level of subjective well-being are a low level of trait neuroticism, high level of trait extraversion, absence of alcoholism, and absence of major depression (3). For example, when heritable variables are controlled, subjective well-being—unlike tested intelligence—is not affected by environmental factors such as income, parental social class, age, and education.
Consistently, relationships are more important to subjective well-being than is money. In a representative study of 800 college alumni, respondents who preferred high income, occupational success, and prestige over having very close friends and a close marriage were twice as likely to describe themselves as “fairly” or “very” unhappy (70). Over the last two decades the doubling of net disposable income in the western world did not affect subjective well-being (3). Mean life satisfaction in socioeconomically challenged Brazil and China is higher than in socioeconomically blessed Japan and Germany.
In some instances environment can be important to subjective well-being. Young widows remain subjectively depressed for years. Even though their poverty has been endured for centuries, respondents in very poor nations, such as India and Nigeria, report lower subjective well-being than those in more prosperous nations. Pain from the loss of a child never stops.
Maintaining self-efficacy, agency, and autonomy make additional environmental contributions to subjective well-being. Subjective well-being is usually higher in democracies than in dictatorships. Assuming responsibility for favorable or unfavorable outcomes (internalization) is another major factor leading to subjective well-being. Placing the blame elsewhere (externalization) significantly reduces subjective well-being. In other words, paranoia and projection make people feel worse rather than better. Religiosity is consistently and positively correlated with well-being, but there may be a chicken-egg relationship between social support and religious observance. For example, among church-goers it is difficult to disentangle where spiritual faith ends and community support begins. The research agenda for subjective well-being includes establishing with greater definition the relative contributions of heredity and of environment and culture. In addition, we need to establish the magnitude of the contribution of subjective well-being to the other models. We need to disentangle interpersonal happiness (model D) from intrapersonal happiness (model E).
Model F: Mental Health as Resilience
In 1865, Claude Bernard, the founder of experimental medicine, declared, “We shall never have a science of medicine as long as we separate the explanation of the pathological from the explanation of normal, vital phenomena” (71). Later, Meyer (72) perhaps overstated the case when he asserted that there are no mental diseases, there are only characteristic patterns of reaction to stress. But Meyer drew attention to the fact that mentally healthy responses to stress, analogous to pus and cough, are often misinterpreted as pathological.
There are three broad classes of coping mechanisms that humans use to overcome stressful situations. First, there are the ways in which an individual elicits help from appropriate others: namely, consciously seeking social support. Second, there are conscious cognitive strategies that we intentionally use to master stress (73). Third, there are involuntary mental coping mechanisms (often called “defense mechanisms” or “denial”) (74). This third, involuntary class of coping mechanisms reduces conflict and cognitive dissonance during sudden changes in internal and external reality. If such sudden changes are not “distorted” and “denied,” they can result in disabling anxiety and/or depression. Such homeostatic mental defenses shield us from sudden changes in the four lodestars of conflict. These four lodestars are affect/impulse, reality, relationships, and social learning. Involuntary coping mechanisms can abolish impulse (e.g., by reaction formation), relationships (e.g., by schizoid fantasy), reality (e.g., by psychotic denial), or social learning (e.g., by acting out). They can alter our conscious recognition of the subject (e.g., by projection) or the object (e.g., by turning against the self) of a conflict, our awareness of the conflictual idea (e.g., by repression), or the conflictual affect associated with the idea (e.g., by isolation of affect).
By 1970, defense mechanisms, like many psychoanalytic metaphors, had been largely discarded by most empirical social scientists. Consistency of definition and rater reliability were lacking. But over the last 30 years, the idea of healthy involuntary coping has entered the literature of empirical cognitive psychology under such rubrics as “hardiness” (75), “self-deception” and “emotional coping” (73), and “illusion” (76). In the last decade experimental strategies for assessing defense mechanisms have also improved (77–80). Several reviews have also clarified our understanding of healthy and unhealthy defenses (81, 82). By offering both a tentative hierarchy and a glossary of consensually validated definitions, an optional axis of involuntary coping mechanisms was added to DSM-IV. The Defensive Function Scale (DSM-IV, p. 752) has set the stage for further progress in our understanding of positive mental health. In addition, in terms of predictive validity (i.e., predicting future mental health), the Defensive Function Scale is as powerful a tool as we have (83–85). Nevertheless, no one has yet developed a method for assessing defenses that meets conventional standards for psychometric reliability. The Q-sort technique is perhaps the most promising (80).
All classes of defenses in the Defensive Function Scale are effective in “denying” or defusing conflict and in “repressing” or minimizing stress, but they differ greatly in the psychiatric diagnoses assigned to their users and in their consequences for long-term biopsychosocial adaptation. In level 1, the most pathological category, are found denial and distortion of external reality. These mechanisms are common in young children, in our dreams, and in psychosis. To breach them requires altering the brain by neuroleptics or waking the dreamer.
More common to everyday life are the relatively maladaptive defenses found in levels 2–5. Defenses in these categories are common in adolescents, in immature adults, and in individuals with personality disorders. They often make others more uncomfortable than the user. Such defenses are consistently and negatively correlated with global assessment of mental health, and they profoundly distort the affective component of interpersonal relationships. The third class of defenses, those in level 6, are often associated with what DSM-IV calls axis I anxiety disorders and with the psychopathology of everyday life. These include mechanisms such as repression, intellectualization, and reaction formation. They are common to everyone from 5 years old until death. They are neither healthy nor unhealthy.
The mechanisms at level 7 still distort and alter feelings, conscience, relationships, and reality, but they achieve these alterations gracefully and flexibly. These mechanisms allow the individual consciously to experience the affective component of interpersonal relationships but in a tempered fashion. Thus, the beholder may regard level 7 adaptive defenses as virtues, just as the same beholder might regard the prejudice of projection and the tantrums of acting out as sins. Doing as one would be done by (altruism), keeping a stiff upper lip (suppression), keeping future pain in awareness (anticipation), being able not to take one’s self too seriously (humor), and turning lemons into lemonade (sublimation) are the very stuff from which positive mental health is made. In addition, the thoughtful reader may wish to add involuntary but adaptive offences: for example, creativity, charisma, leadership, courage, and vision. Unfortunately, like tightrope walking, without months of practice mature mechanisms cannot easily be deployed voluntarily and only then by those with innate balance.
Identification of defenses is difficult and has impeded research. Rarely can we identify our own defenses, and we often fail to recognize them in others or even project our own. Like other facets of mental health, the reliable identification of healthy but unconscious defenses requires longitudinal study. Whether we ultimately view another’s coping response as healthy or psychopathic depends on the results of their involuntary efforts.
Besides establishment of rater reliability and obtaining further evidence that the Defensive Function Scale deserves to be retained, twin and fMRI studies are needed to test whether these metaphorical mechanisms are, as hypothesized, biologically based homeostatic processes. The research agenda must include examination of how best to facilitate in the clinic the transformation of less adaptive defenses into more adaptive defenses. One suggestion has been, first, to increase social supports and interpersonal safety and, second, to facilitate the intactness of the CNS (e.g., through rest, nutrition, and sobriety) (53).
Future Directions
In conclusion, it seems important to review some of the safeguards for a study of positive mental health. Mental health must always be broadly defined in terms that are culturally sensitive and inclusive. The criteria for mental health must be empirically and longitudinally validated. Third, validation means special attention to cross-cultural studies (86). Fourth, in trying to improve mental health we must respect individual autonomy. Finally, any student of health must remember that there are differences between real mental health and value-ridden morality, and between real success at living and mere questing after the bitch goddess success.
Nevertheless, we need to be able to measure and record mental health. The mental status and formulation should both reflect not only the absence of symptoms but also an assessment of social competence and coping style. Although room exists for improvement, axis V, the GAF Scale, provides the same reliability as and greater predictive validity than the presence or absence of most axis I and II designations. No psychiatric chart should be without it. The capacities to work and to love over time are extremely important indices of mental health. They are far more important than the cross-sectional presence or absence of anxiety, depression, or illegal drug use. But such capacities must be assessed longitudinally. “How many years since age 21 have you spent employed?” is a more useful question than “What is your present job?” Again, “Tell me about your longest intimate relationship” is much more useful than “Are you married?”
As with the blind men and the elephant, this article has suggested six conceptually distinct ways to assess a single construct—mental health. It would be a terrible mistake to believe any one of these six models superior to all the others. Rather, all are important and all are highly correlated with each other (83). In conducting future research on positive mental health, multivariate comparison will be needed to reveal the relative contribution of each model. Equally important, in the area of national health policy, if and when interventions to improve positive mental health are identified, who should pay: the consumer, the educational system, the medical care system, or some as-yet-to-be-identified payer?
Received Aug. 21, 2002; revision received Dec. 27, 2002; accepted Jan. 10, 2003. From the Department of Psychiatry, Brigham and Women’s Hospital. Address reprint requests to Dr. Vaillant, Department of Psychiatry, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115; [email protected] (e-mail). Supported by NIMH grant MH-42248.
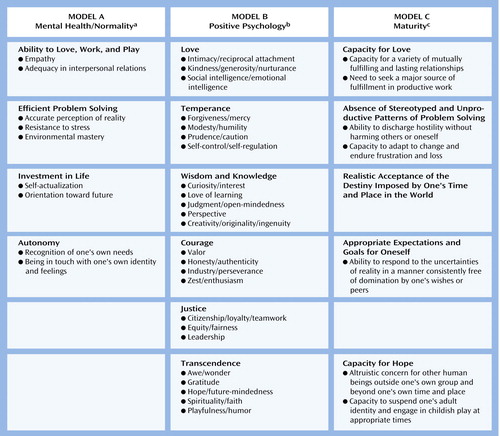
Figure 1. Three Definitions of Mental Health in the Last Half Century
aBased on description by Jahoda (18) as summarized by Offer and Sabshin (19).
bBased on description by Peterson and Seligman (20).
cBased on description by Menninger (21).
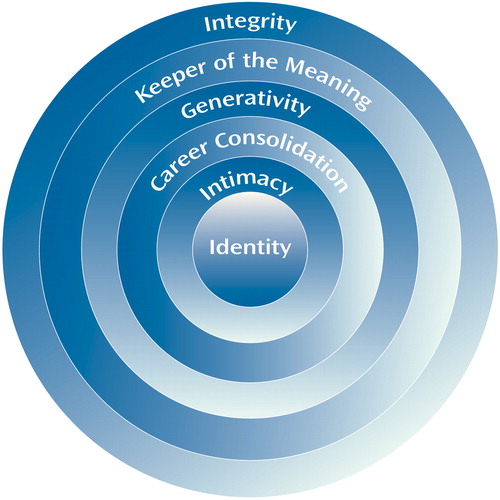
Figure 2. Model of Adult Development Combining Erikson’s Four Tasks With Two Others (Career Consolidation and Keeper of the Meaning)
1. Erikson EH: Growth and crises of the “healthy personality,” in Symposium on the Healthy Personality: Supplement II of the Fourth Conference on Infancy and Childhood. Edited by Senn MJE. New York, Josiah Macy, Jr, Foundation, 1950, pp 1–95Google Scholar
2. Offer D, Sabshin M: Normality, in The Comprehensive Textbook of Psychiatry, 3rd ed, vol 3. Edited by Kaplan HI, Freedman AM, Sadock BJ. Baltimore, Williams & Wilkins, 1980, pp 608–613Google Scholar
3. Diener E, Suh EM, Lucas RE, Smith HL: Subjective well-being: three decades of progress. Psychol Bull 1999; 125:276–302Crossref, Google Scholar
4. Report to the President From the President’s Commission on Mental Health, vol I: Number 040–000–00390–8. Washington, DC, US Government Printing Office, 1978Google Scholar
5. Goldman HH, Skodol AE, Lave TR: Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry 1992; 149:1148–1156Link, Google Scholar
6. Heath C: What People Are. Cambridge, Mass, Harvard University Press, 1945Google Scholar
7. Vaillant GE: Adaptation to Life. Boston, Little, Brown, 1977Google Scholar
8. Vaillant GE: Aging Well. New York, Little, Brown, 2002Google Scholar
9. Maslow AH: The Farthest Reaches of Human Nature. New York, Viking, 1971Google Scholar
10. Quetelet A: A Treatise on Man, and the Development of His Faculties (1835). Edinburgh, William and Robert Chambers, 1842Google Scholar
11. White RW: Lives in Progress. New York, Dryden, 1952Google Scholar
12. Srole L, Langer TS, Michael ST, Opler MK, Rennie TAC: Mental Health in the Metropolis. New York, McGraw-Hill, 1962Google Scholar
13. Leighton AH: My Name Is Legion: The Stirling County Study, vol 1. New York, Basic Books, 1959Google Scholar
14. Leighton DC, Harding JS, Macklin D, MacMillan AM, Leighton AH: The Character of Danger: The Stirling County Study, vol 3. New York, Basic Books, 1963Google Scholar
15. Grinker RR, Spiegel J: Men Under Stress. Philadelphia, Blakiston, 1945Google Scholar
16. Lewis A: Between guesswork and certainty in psychiatry. Lancet 1958; 1:227Crossref, Medline, Google Scholar
17. Redlich FC: The concept of health psychiatry, in Explorations of Social Psychiatry. Edited by Leighton AH, Clausen JA, Wilson R. New York, Basic Books, 1957Google Scholar
18. Jahoda M: Current Concepts of Positive Mental Health. New York, Basic Books, 1958Google Scholar
19. Offer D, Sabshin M: Normality: Theoretical and Clinical Concepts of Mental Health. New York, Basic Books, 1966Google Scholar
20. Peterson C, Seligman MEP: The Values in Action Classification of Strengths. Washington, DC, American Psychological Association (in press)Google Scholar
21. Menninger WC: A Psychiatrist for a Troubled World: Selected Papers of William C Menninger, MD. New York, Viking Press, 1967, pp 788–804Google Scholar
22. Grinker RR Sr, Grinker RR Jr, Timberlake J: A study of mentally healthy young males (homoclites). Arch Gen Psychiatry 1962; 6:405–453Crossref, Medline, Google Scholar
23. Oden MH: The fulfillment of promise: 40-year follow-up of the Terman gifted group. Genet Psychol Monogr 1968; 77:3–93Medline, Google Scholar
24. Clausen J: American Lives. New York, Free Press, 1993Google Scholar
25. Jones CJ, Meredith W: Developmental paths of psychological health from early adolescence to later adulthood. Psychol Aging 2000; 15:351–360Crossref, Medline, Google Scholar
26. Korchin SJ, Ruff GF: Personality characteristics of the Mercury astronauts, in The Threat of Impending Disaster. Edited by Massachusetts Institute of Technology. Boston, MIT Press, 1964, pp 197–207Google Scholar
27. Perry CJG: Psychiatric selection of candidates for space missions. JAMA 1965; 194:841–844Crossref, Medline, Google Scholar
28. Kernberg OF, Coyne L, Horwitz L, Appelbaum A, Burstein ED: Psychotherapy and psychoanalysis. the application of facet theory and the multidimensional scalogram analysis to the quantitative data of the psychotherapy research project. Bull Menninger Clin 1972; 36:87–275Medline, Google Scholar
29. Luborsky L: Clinicians’ judgments of mental health: a proposed scale. Arch Gen Psychiatry 1962; 7:407–417Crossref, Medline, Google Scholar
30. Luborsky L, Bachrach H: Factors influencing clinicians’ judgment of mental health: eighteen experiences with the Health-Sickness Rating Scale. Arch Gen Psychiatry 1974; 31:292–299Crossref, Medline, Google Scholar
31. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
32. Armelius BA, Gerin P, Luborsky L, Alexander L: Clinician’s judgment of mental health: an international validation of HSRS. Psychother Res 1991; 1:31–38Crossref, Google Scholar
33. Seligman MEP, Csikszentmihalyi M: Positive psychology. Am Psychol 2000; 55:5–14Crossref, Medline, Google Scholar
34. Maslow AH: Motivation and Personality, 2nd ed. New York, Harper & Row, 1970Google Scholar
35. Meyer A: Suggestions of a Modern Science Concerning Education. New York, Macmillan, 1925, p 118Google Scholar
36. Seligman MEP: Learned Optimism. New York, Simon & Schuster, 1991Google Scholar
37. Seligman MEP: Authentic Happiness. New York, Free Press, 2002Google Scholar
38. Taylor SE, Brown JD: Illusion and well-being: some social psychological contributions to a theory of mental health. Psychol Bull 1988; 103:193–210Crossref, Medline, Google Scholar
39. Baxter LR, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta Alazrak A, Selin CE, Ferris HK, Punford P, Phelps ME: Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49:681–689Crossref, Medline, Google Scholar
40. Beck AT: Depression: Clinical, Experimental and Theoretical Aspects. New York, Hoeber, 1967Google Scholar
41. Peterson C, Seligman MEP: Causal explanations as a risk factor for depression: theory and evidence. Psychol Rev 1984; 91:347–374Crossref, Medline, Google Scholar
42. Snyder CR, Lopez SJ: Handbook of Positive Psychology. New York, Oxford University Press, 2002Google Scholar
43. Schaie KW: The Seattle Longitudinal Study: a 21-year exploration of psychometric intelligence in adulthood, in Longitudinal Studies of Adult Psychological Development. Edited by Schaie KW. New York, Guilford, 1983, pp 64–135 Google Scholar
44. Yakovlev PI, Lecours AR: The myelogenetic cycles of regional maturation of the brain, in Regional Development of the Brain in Early Life. Edited by Minkowski A. Oxford, UK, Blackwell Scientific, 1967, pp 3–69Google Scholar
45. Benes FM, Turtle M, Khan Y, Farol P: Myelinization of a key relay in the hippocampal formation occurs in the human brain during childhood, adolescence, and adulthood. Arch Gen Psychiatry 1994; 51:477–484Crossref, Medline, Google Scholar
46. Erikson E: Childhood and Society. New York, WW Norton, 1950Google Scholar
47. Loevinger J: Ego Development. San Francisco, Jossey-Bass, 1976Google Scholar
48. Kohlberg L: Essays on Moral Development, vol 2: The Nature and Validity of Moral Stages. San Francisco, Harper & Row, 1984Google Scholar
49. Fowler J: Stages of Faith. New York, Harper & Row, 1981Google Scholar
50. White RW: Lives in Progress, 3rd ed. New York, Holt Rinehart & Winston, 1975Google Scholar
51. Heath DH: Maturity and Competence: A Transcultural View. New York, Gardner Press, 1977Google Scholar
52. Vaillant GE, Milofsky ES: Natural history of male psychological health, IX: empirical evidence for Erikson’s model of the life cycle. Am J Psychiatry 1980; 137:1348–1359Link, Google Scholar
53. Vaillant GE: The Wisdom of the Ego. Cambridge, Mass, Harvard University Press, 1995Google Scholar
54. Hauser ST: Adolescents and Their Families. New York, Free Press, 1991Google Scholar
55. Franz CE: Does thought content change as individuals age? a longitudinal study of midlife adults, in Can Personality Change? Edited by Heatherington TF, Weinberger JL. Washington, DC, American Psychological Association, 1994, pp 227–250Google Scholar
56. Goleman D: Emotional Intelligence. New York, Bantam Books, 1995Google Scholar
57. Oden S, Schweinhart L, Weikart D: Into Adulthood: A Study of the Effects of Head Start. Ypsilanti, Mich, High Scope Press, 2000Google Scholar
58. Davidson RJ: Affective style, psychopathology and resilience: brain mechanisms and plasticity. Am Psychol 2000; 55:1196–1214Crossref, Medline, Google Scholar
59. Ledoux J: The Emotional Brain. New York, Simon & Schuster, 1996Google Scholar
60. Salovey P, Mayer JD, Caruso D, Lopes PN: Measuring emotional intelligence as a set of abilities with the MSCEIT, in Positive Psychological Assessment : A Handbook of Models and Measures. Edited by Lopez SJ, Snyder CR. Washington, DC, American Psychological Association, 2003Google Scholar
61. Gardner H: Multiple Intelligences: The Theory in Practice. New York, Basic Books, 1993Google Scholar
62. Csikszentmihalyi M: Flow: The Psychology of Optimal Experience. New York, Harper & Row, 1990Google Scholar
63. Frederickson BL: What good are positive emotions? Rev Gen Psychol 1998; 2:300–319Crossref, Medline, Google Scholar
64. Snowdon DA: Aging With Grace. New York, Bantam, 2001Google Scholar
65. Ostir G, Markides K, Black S, Goodwin J: Emotional well-being predicts subsequent functional independence and survival. J Am Geriatr Soc 2000; 48:473–478Crossref, Medline, Google Scholar
66. Wilson W: Correlates of avowed happiness. Psychol Bull 1967; 67:294–306Crossref, Medline, Google Scholar
67. Danner DD, Snowdon DA, Friesen WV: Positive emotions in early life and longevity: findings from the Nun Study. J Pers Soc Psychol 2001; 80:804–813Crossref, Medline, Google Scholar
68. Diener E: Subjective well-being. Am Psychol 2000; 55:34–43Crossref, Medline, Google Scholar
69. Tellegen A, Lykken DT, Bouchard TJ, Wilcox KJ, Segal NL, Rich S: Personality similarity in twins reared apart and together. J Pers Soc Psychol 1988; 54:1031–1039Crossref, Medline, Google Scholar
70. Perkins HW: Religious commitment, Yuppie values and well-being in post-collegiate life. Rev Relig Res 1991; 32:244–251Crossref, Google Scholar
71. Bernard C: An Introduction to the Study of Experimental Medicine (1865). New York, Dover, 1957, p 146Google Scholar
72. Meyer A: The Commonsense Psychiatry of Dr Adolf Meyer. Edited by Lief A. New York, McGraw-Hill, 1948Google Scholar
73. Lazarus RS, Folkman S: Stress, Appraisal and Coping. New York, Springer, 1984Google Scholar
74. Freud A: The Ego and Mechanisms of Defense. London, Hogarth Press, 1937Google Scholar
75. Kobasa SC, Maddi SR, Kahn S: Hardiness and health: a prospective study. J Pers Soc Psychol 1982; 42:168–177Crossref, Medline, Google Scholar
76. Taylor S: Positive Illusions: Creative Self-Deception and the Healthy Mind. New York, Basic Books, 1989Google Scholar
77. Horowitz MJ, Markman HC, Stinson C: A Classification Theory of Defense in Repression and Dissociation. Edited by Singer JL. Chicago, University of Chicago Press, 1990Google Scholar
78. Cramer P: The Development of Defense Mechanisms. New York, Springer Verlag, 1991Google Scholar
79. Perry JC, Ianni F: Observer rated measures of defense mechanisms. J Pers 1998; 66:993–1024Crossref, Google Scholar
80. Vaillant GE: Ego Mechanisms of Defense: A Guide for Clinicians and Researchers. Washington, DC, American Psychiatric Press, 1992Google Scholar
81. Conte HR, Plutchik R: Ego Defenses: Theory and Measurement. New York, John Wiley & Sons, 1995Google Scholar
82. Skodol AE, Perry JC: Should an axis for defense mechanisms be included in DSM-IV? Compr Psychiatry 1993; 34:108–119Crossref, Medline, Google Scholar
83. Vaillant GE, Schnurr P: What is a case? a 45-year study of psychiatric impairment within a college sample selected for mental health. Arch Gen Psychiatry 1988; 45:313–327Crossref, Medline, Google Scholar
84. Vaillant GE: Adaptive mental mechanisms: their role in a positive psychology. Am Psychol 2000; 55:89–98Crossref, Medline, Google Scholar
85. Vaillant GE, Mukamal K: Successful aging. Am J Psychiatry 2001; 158:839–847Link, Google Scholar
86. Tseng WS: Handbook of Cultural Psychiatry. San Diego, Academic Press, 2001Google Scholar



