In This Issue
Depression, Alzheimer Style
The frequency of major depression generally declines with age among older Americans, but major depression followed the onset of Alzheimer’s disease in approximately 25% of the least demented patients at four research centers and nearly 50% of those with severe dementia. Zubenko et al. (p. 857) propose major depressive syndrome of Alzheimer’s disease as a separate depressive subtype. In addition to the high prevalence, its clinical features distinguish it from depression among elderly patients without Alzheimer’s disease: those with Alzheimer’s disease were significantly more likely to have diminished concentration or indecisiveness and were less likely to have disturbed sleep or feelings of guilt or worthlessness. The frequency of psychosis increased with greater dementia severity. The prevalence of Alzheimer’s disease is increasing with the growing elderly U.S. population, thus creating a large subgroup of patients with major depression in Alzheimer’s disease.
Marker of Hippocampal Abnormalities in Bipolar Disorder
Magnetic resonance imaging (MRI) has shown that the hippocampus of patients with major depression is smaller than normal. Findings for bipolar disorder have been equivocal, and it is possible that hippocampal pathology in this illness is too subtle to be detected with MRI-based volume measurements. N-Acetylaspartate is the second most abundant amino acid in the central nervous system, and low levels have been associated with neuronal and axonal injury. It is reliably measured by proton magnetic resonance spectroscopy, which Deicken et al. (p. 873) used to measure N-acetylaspartate in the hippocampus of patients with familial bipolar disorder. Levels in both hemispheres were significantly lower in the patients than in healthy comparison subjects. Lower levels of N-acetylaspartate in the right hippocampus were associated with longer illness duration. This correlation suggests that illness progression results in further neuropathology and may involve the right hemisphere more than the left.
Dynamics of Dopamine Receptors in Methamphetamine Users
Methamphetamine is a widely used stimulant drug that enhances release of the neurotransmitter dopamine in the human brain. The behavioral action of dopamine is mediated in part through stimulation of the enzyme adenylyl cyclase by way of the dopamine D1 receptor. It has been suspected that some of the behavioral changes associated with chronic use of methamphetamine might be due to abnormal D1 receptor function. Tong et al. (p. 896) report that postmortem D1 stimulation of adenylyl cyclase was 25%–30% lower in all three striatal subregions (nucleus accumbens, caudate, and putamen) of brains from long-term methamphetamine users than in comparison subjects without substance abuse or neuropathology. These data suggest that brain dopamine D1 receptor function might be low in human methamphetamine users, a change that could explain some of the consequences (e.g., drug craving, tolerance) of repeated drug exposure.
Childhood Sexual Abuse, Without PTSD, Leaves Hippocampus Intact
Several aspects of memory—flashbacks, intrusive recollections, impaired learning—are prominent in posttraumatic stress disorder (PTSD). The hippocampus is critical to memory and is affected by stress. Low hippocampal volume or indicators of neuronal damage are common in patients with PTSD, but are these effects of PTSD or of the original trauma? Bremner et al. (p. 924) assessed both hippocampal volume and functioning in women with a childhood history of severe sexual abuse; 10 had developed PTSD, and 12 had not. The women with PTSD had a 16% lower mean hippocampal volume and showed significantly less brain activity during a verbal memory task. Deficits in hippocampal structure and functioning thus appear to be specific to PTSD and not an outcome of childhood sexual abuse per se.
Self-Help for Bulimia Nervosa
Cognitive behavior self-help programs for bulimia nervosa have shown promise, but it is not clear whether the cognitive behavior approach is essential and which patients are most likely to benefit. Carter et al. (p. 973) assessed baseline characteristics of female patients with bulimia nervosa and assigned them to three treatment types: a self-help manual with a cognitive behavior focus, a self-help manual emphasizing assertiveness, and a waiting list. After 8 weeks, both groups given self-help manuals showed significant reductions in binge eating and purging, whereas patients on the waiting list did not. Episodes of binge eating or purging decreased by at least half for 54% of the women given the cognitive behavior self-help manual, 56% of those given the assertiveness self-help manual, and 32% of those on the waiting list. Greater improvement occurred for women with less baseline knowledge of eating disorders, more difficulty with intimacy, greater compulsivity, and greater perfectionism. Illness severity did not predict outcome.
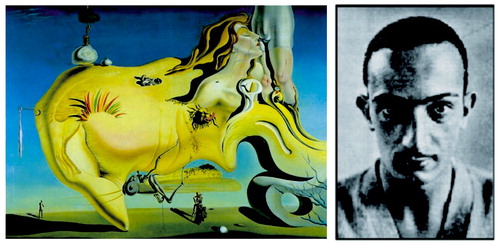
Images in Psychiatry
Dalí (1904–1989): Psychoanalysis and Pictorial Surrealism (p. 855)

Correlation Between Right Hippocampal N-Acetylaspartate Concentration and Years of Illness in Euthymic Male Outpatients With Bipolar I Disorder