Controlled Clinical Trial of Interpersonal Psychotherapy Versus Parenting Education Program for Depressed Pregnant Women
Abstract
OBJECTIVE: Antenatal depression is a significant risk factor for postpartum depression, with a 10%–12% prevalence in all pregnancies. Rates of depression are higher for pregnant women with chronic stressors, financial and housing problems, and inadequate social support. Despite the prevalence and associated family and infant morbidity, there are no controlled clinical treatment trials regarding this topic, to the authors’ knowledge. APA has identified treatment of depression during pregnancy as a priority for clinical guidelines. METHOD: A 16-week bilingual controlled clinical trial compared a group receiving interpersonal psychotherapy for antepartum depression to a parenting education control program. Fifty outpatient antepartum women who met DSM-IV criteria for major depressive disorder were randomly assigned to interpersonal psychotherapy or a didactic parenting education program. Thirty-eight women remained in the study and were included in the data analysis. Depressed mood was measured with the Edinburgh Postnatal Depression Scale, the Beck Depression Inventory, and the Hamilton Depression Rating Scale. The Clinical Global Impression (CGI) and the Hamilton depression scale measured recovery. RESULTS: The interpersonal psychotherapy treatment group showed significant improvement compared to the parenting education control program on all three measures of mood at termination. Recovery criteria were met in 60% of the women treated with interpersonal psychotherapy, according to a CGI score of ≤2. In addition, there was a significant correlation between maternal mood and mother-infant interaction. CONCLUSIONS: Interpersonal psychotherapy is an effective method of antidepressant treatment during pregnancy and should be a first-line treatment in the hierarchy of treatment for antepartum depression.
The fact that 10%–12% of pregnant women experience depression dispels the myth of unconditional well-being during gestation (1–3). In a recent prospective longitudinal cohort study of 14,000 antepartum women (4), 13.5% scored above the threshold for probable depression on the Edinburgh Postnatal Depression Scale at 32 weeks of pregnancy, compared to 9.1% at 8 weeks postpartum.
Women with a history of depression are particularly vulnerable to pregnancy-associated recurrence (5). The gonadal hormones once thought to be protective during pregnancy may provoke uncertain mood effects (6). Furthermore, that one-half of pregnant depressed women will have postpartum depression (7) emphasizes pregnancy as the paramount time for identification, treatment, and prevention.
Risk factors for depression during pregnancy include personal or family history of mood disorder, stressors such as marital dysfunction (8), and demographic variables such as young age, minimal education, larger number of children (1), and a history of child abuse (9).
The majority of women in our study group were immigrants from the Dominican Republic with few support systems and low socioeconomic status. Several factors increased the odds of depression in our group. There are conflicting data on the prevalence of depression among Hispanic immigrants (10, 11). The ethnicity of our group must be seen against the backdrop of other circumstances such as poverty, isolation, chaos, pregnancy, immigrant status, and absence of the baby’s father and other support systems. Studies of pregnant and postpartum women (12) have addressed these variables.
When Hobfoll and colleagues (13) evaluated 192 financially impoverished inner-city single women at two intervals during pregnancy, they found rates of depression of 27.5% and 24.5%. Seguin et al. (14) found that 47% of pregnant women of low socioeconomic status and 20% of women with higher socioeconomic status scored >10 on the Beck Depression Inventory. Chronic stressors, financial and housing problems, negative life events, and inadequate social support were all linked to high depressive symptom profiles during pregnancy.
Timely and appropriate treatment is vital in order to avoid depression-associated appetite and weight loss. Pregnant depressed women are more vulnerable to nicotine, drug, and alcohol abuse and failure to obtain adequate prenatal care (15)—all factors that compromise fetal development. Maternal stress and depression during pregnancy are associated with lower birth weight and gestational age (16), delivery by cesarean section, and admittance of infants to a neonatal care unit (17). Neurobehavioral effects on infants of depressed mothers have been reflected in frontal lobe activity on EEGs (18). Furthermore, maternal-fetal attachment may be explored during gestation in order to facilitate resolution of conflicts or ambivalence before delivery (19).
Alternative Therapies
Although selective serotonin reuptake inhibitors and some other antidepressant medications have demonstrated relative safety during gestation (20), absolute safety cannot be ensured. The infant’s developing brain continues to be vulnerable to adverse events. Data remains limited by small group numbers and unknown long-term effects. Moreover, some women may not want to ingest medication and prefer nonpharmacological treatments. A recent pilot study by Oren et al. (21) suggested that light therapy is beneficial for the treatment of antepartum depression. To date, this interpersonal psychotherapy study is the only randomized controlled clinical trial we know of that suggests an efficacious treatment for antepartum depression.
Several clinical trials have demonstrated the efficacy of interpersonal psychotherapy in the treatment of major depression (22), postpartum depression (23), and depressed adolescents (24). Furthermore, more scientific evidence for the benefits of psychotherapy for depressed subjects treated with interpersonal psychotherapy, compared to control subjects, is associated with brain and physiological change (25).
A risk-benefit analysis is the most appropriate method for intervention. The elegant presentation of Wisner et al. (26) regarding decision analysis for the treatment of childbearing women provides guidelines for choosing appropriate interventions. Interpersonal psychotherapy is an effective treatment that precludes any possible danger to the fetus.
Interpersonal Psychotherapy
Our initial antepartum pilot study (27) suggested that interpersonal psychotherapy is a successful treatment as well as a mechanism of prevention of depression in this population of women. The application of interpersonal psychotherapy to the specific problems and needs of women with antepartum depression is outlined in a manual (28) (and may be obtained from the authors).
Because of the unique and developmental problems associated with gestation, an additional problem area addresses issues unique to pregnancy that cannot be covered by using the original interpersonal psychotherapy problem set (29): grief, interpersonal role disputes, role transitions, and interpersonal deficits. This fifth broad area, complicated pregnancy, addresses problems specific to gestation such as undesired pregnancy, medical problems associated with pregnancy itself, obstetrical complications, multiple births, and congenital anomalies.
The participants met for 45-minute weekly sessions with therapists. Interpersonal psychotherapy was administered over 16 weeks, according to the manual by Klerman et al. (29). The therapy was modified to antepartum depression according to the interpersonal psychotherapy manual (28).
Parenting Education Program
The parenting education program is a systematic didactic control condition of therapist-led weekly educational sessions. The patients were assigned a therapist and seen weekly for 45-minute sessions to discuss their symptoms and functioning. Similar to the interpersonal psychotherapy treatment, the parenting education control condition lasted for 16 weeks.
During parenting education program sessions, the therapist emphasizes the developmental stages of pregnancy, delivery, parenting, and early childhood. The therapist may also facilitate attaining concrete services (housing, etc.) but does not provide specific emotional support in any way similar to interpersonal psychotherapy.
The parenting education program permits weekly evaluation of the patient’s mood and control for contact with a professional as well as the nonspecific effects of repeated evaluations. In addition, the weekly contact with a therapist provides an ethical and reliable way of evaluating the patient’s mood. Therapists were available by beeper at all times for emergencies.
We considered using a waiting-list control; however, a waiting-list control does not control for the aforementioned variables and provides no mechanism for frequent face-to-face evaluation of worsening symptoms (23, 24).
We report the results of a randomized controlled clinical treatment trial on the efficacy of 16 weeks of interpersonal psychotherapy compared to a parenting education control program.
Aims
The aims of this study were 1) to determine the efficacy of interpersonal psychotherapy versus a parenting education program for unipolar depressed nonpsychotic pregnant women and 2) to test the feasibility of a placebo-controlled bilingual clinical treatment trial in an ethnically and economically diverse population of pregnant depressed women.
To our knowledge, this interpersonal psychotherapy treatment trial had the following three unique characteristics: it was 1) the first controlled clinical trial of individual psychotherapy for antepartum depression, 2) the first interpersonal psychotherapy study with a matched systematic nontherapeutic control group to assess the therapeutic benefits of interpersonal psychotherapy, and 3) the first reported bilingual interpersonal psychotherapy treatment in a population of socioeconomically deprived women.
Method
Training in Interpersonal Psychotherapy
Two experienced therapists (with an M.D. and a C.S.W.) received 1 year of interpersonal psychotherapy supervision. Their training included modification of their training skills to include interpersonal psychotherapy in order to provide a uniform method of procedure and psychotherapy treatment. All trainees read the interpersonal psychotherapy book and the interpersonal psychotherapy manual in preparation for the training. One Spanish-speaking therapist provided treatment for our large Latina population. The interpersonal psychotherapy training program was modeled after that used in the National Institute of Mental Health (NIMH) collaborative study of treatment of depression (22). A 5-day didactic program described the clinical strategies of interpersonal psychotherapy in addition to the physical, psychological, and developmental phases of pregnancy.
After the didactic sessions, the clinicians entered a clinical program that included supervision of three patients, each over a 16-week period. The patients were assigned incrementally. The therapists treated one patient at a time; a second patient was assigned when the therapist was judged to be competent in the techniques of interpersonal psychotherapy. The supervisor, who was the principal investigator (M.G.S.), made the assignments. All sessions were videotaped and subsequently reviewed by the supervisor (30). Weekly supervision included a 1-hour videotaped review in order to ensure reliable treatment methods. After completion of all cases of interpersonal psychotherapy, certified interpersonal psychotherapists reviewed three tapes of each patient in order to determine qualification for certification.
The therapists in training met monthly to discuss patients and address problems, treatment strategies, procedural methods, and difficulties with the protocol—all to insure uniformity of method. Both therapists were judged competent. The patients treated during the therapist training were excluded from the study group.
Training in Parenting Education
The supervisor met with the therapists and provided written instruction, books on pregnancy, the postpartum, and early childhood as well as videotapes and visual aids that addressed the developmental stages of pregnancy, childbirth, and early parenting. There were few limitations on the content of instruction as long as the focus remained didactic.
The therapists tailored the parenting education program sessions to the gestational age of the study participants. Regular conferences were held to discuss and review tapes and to alert the therapists to potential treatment bias.
The important point addressed in the parenting education program was to avoid any psychological intervention that may be similar to interpersonal psychotherapy. Videotapes of both interpersonal psychotherapy and parenting education program sessions were reviewed for supervision, evaluation of the quality of sessions, treatment adherence, and integrity.
Patients
More than 200 prospective research participants were recruited to the Maternal Mental Health Program from our outpatient clinics at the New York State Psychiatric Institute of Columbia University College of Physicians and Surgeons as well as other institutions in the New York metropolitan area. They were referred by professionals, community outreach programs, and former patients. A majority of Latina patients came from the social workers and midwives at our prenatal clinic in the Department of Obstetrics and Gynecology. Other subjects were self-referred, having heard about the Maternal Mental Health Program from newspapers, magazines, and radio announcements.
Fifty pregnant depressed women entered the study. Twenty-five were randomly assigned to the experimental treatment interpersonal psychotherapy group and 25 to the parenting education control program by using a table of random numbers. Thirty-eight women who completed at least one interpersonal psychotherapy or parenting education program session were included in the data analysis.
English- and Spanish-speaking, physically healthy pregnant women between 6 and 36 weeks’ gestation and 18 and 45 years of age were included in the study. Of the Latina women, 80% were Spanish speaking. Consent forms were bilingual. All women understood the study and gave written informed consent to participate. Diagnostic inclusion criteria were based on DSM-IV criteria for major depressive disorder and a Hamilton Depression Rating Scale score ≥12. Only pregnant women with major depression entered the study.
Patients were excluded if they had abused drugs or alcohol in the past 6 months, were acute risks for suicide, or had comorbid axis I disorders or medical conditions likely to interfere with participation in the study. Patients currently taking antidepressant medication were also excluded from the study.
Assessments of Change
After a baseline psychiatric evaluation, the Structured Clinical Interview for DSM-IV Axis I Disorders (31) was administered to determine the presence of major depressive disorder and to rule out comorbid axis I diagnosis.
All assessments were translated and back-translated to Spanish in the Dominican dialect. The Hamilton depression scale (32) was the principal clinician-rated outcome measure. Because the discomforts of pregnancy may mimic somatic symptoms of depression (33), the patients were asked to evaluate whether symptoms such as appetite and weight change were likely due to pregnancy or depression.
The Beck Depression Inventory (34) is a self-rated measure of depressive symptoms in both the general and puerperal (35) populations. The cognitive-affective cluster of symptoms is the most sensitive to “true” depression during pregnancy (36). Because the removal of the somatic cluster does not reduce the value of the Beck Depression Inventory, the somatic cluster was eliminated (37, 38).
The self-rated Edinburgh Postnatal Depression Scale (39) emphasizes behavioral changes with no emphasis on somatic changes. Although primarily designed for postpartum mood states, it has been used as a sensitive measure in pregnancy (40) and translated into Spanish (41). The Edinburgh Postnatal Depression Scale is the only self-report mood scale validated for use during pregnancy and the postpartum period (sensitivity=86%, specificity=78%). The Clinical Global Impression (CGI) (42) provides measures of severity and improvement of depressive symptoms.
Weekly assessments of mood change were administered before interpersonal psychotherapy or parenting education program sessions in order to avoid treatment effects. A modified version of the Maudsley Mother Infant Interaction Scale (43) was used to measure mother-infant interaction in the postpartum period.
Data Analysis
Intent-to-treat analysis was performed with the last score carried forward. A group size of 38 subjects was used in the analysis (17 control and 21 treatment subjects). The chi-square test was used to determine significant differences in patient demographic and other characteristics. Pretreatment and posttreatment differences in means for both groups on outcome measures of depression were assessed by using paired t tests. Overall efficacy of treatment was assessed as follows.
The efficacy of the two treatments was determined by comparing scores on measures of depressive symptoms (the Hamilton depression scale, the Beck Depression Inventory, the Edinburgh Postnatal Depression Scale) by using intent-to-treat analysis and the last phase as outcome, with the last score carried forward. A repeated analysis of variance model was used to compare outcome scores of the two groups at termination. Recovery status of the two groups was compared by using contingency-table chi-square tests and defined as a score of ≤6 on the Hamilton depression scale or a CGI of 1 (very much improved) or 2 (much improved). Pearson’s correlation coefficients were used to compare scores on the Maudsley Mother Infant Interaction Scale and the Hamilton depression scale. All statistical tests were two-tailed and used an alpha level of 0.05.
Results
Demographic Characteristics
There were no significant differences between the groups regarding race, marital status, gravity, education, employment status, income, or history of depression (Table 1). The mean age of the interpersonal psychotherapy group was 28.3 years (SD=5.7), and the mean age of the parenting education program control group was 29.3 years (SD=7.11). Women entered the study at 21.5 weeks (SD=8.3) (interpersonal psychotherapy group) and 21.0 weeks (SD=6.8) (parenting education control group) of gestation.
The diversity in our patient group is reflected by the large Latina group; 61.9% (13 of 21) of the interpersonal psychotherapy group and 70.6% (12 of 17) of the parenting education control group were representative of the Latina population of our catchment area in the New York State Psychiatric Institute. Other groups represented in the interpersonal psychotherapy and parenting education groups were white (28.6% [six of 21] and 29.4% [five of 17, respectively]) and African American (9.5% [two of 21] and zero). Our study group was composed of many immigrants from the Dominican Republic. About one-half of the women were single, separated, or divorced, and one-half were married or living with a significant other. More than one-half of our group (52.5%) had an income of less than $25,000, and 36.8% had an income of less than $15,000.
A history of child abuse was reported by 47.0% of the women, sexual abuse by 28.0%, physical abuse by 25.0%, and both of the latter for 5.6%, while 73.0% reported a past history of major depression.
Assessments of Mood
Interpersonal psychotherapy demonstrated significant advantage over parenting education for all mood scores (Table 2), while both groups showed marked improvement over the course of treatment. The mood of the interpersonal psychotherapy treatment group improved significantly more than the parenting education program control group on scores on the Edinburgh Postnatal Depression Scale (t=2.99, df=36, p=0.005). The treatment group showed a steeper downward curve, with lower scores by week 7 that continued to fluctuate through week 12 (Figure 1), while the parenting education program group’s score maintained a rather flat plateau. However, mood improvement (Table 2) was marked in both groups: 33.3% of the interpersonal psychotherapy group (t=5.70, df=19, p=0.001) and 11.8% of the parenting education program group (t=2.07, df=17, p=0.054).
Figure 2 and Figure 3 illustrate that the interpersonal psychotherapy treatment effect was significantly better than control effect on scores on the Hamilton depression scale (t=2.42, df=36, p<0.03) and the Beck Depression Inventory (t=2.72, df=31, p<0.02), respectively. The shape and direction of the curves were similar to that of the Edinburgh Postnatal Depression Scale, with a steep drop at week 7 and mild fluctuation until week 12. The treatment group had a >50% improvement in mood symptoms on the Hamilton depression scale (52.4%) (t=8.85, df=20, p=0.001) and the Beck Depression Inventory (52.4%) (t=5.35, df=15, p=0.001), compared to the control subjects (29.4% and 23.5%; t=3.68, df=16, p=0.002, and t=2.51, df=16, p<0.03, respectively).
Recovery Status
The difference in the recovery rate on the CGI was significant between the groups (χ2=6.42, df=1, p<0.02). The interpersonal psychotherapy group had a recovery rate of 60.0%, compared to the 15.4% rate of the parenting education control program (Figure 4). Those who “recovered,” with a Hamilton depression scale score of ≤6, were 19.0% of the interpersonal psychotherapy group and 0.0% of the parenting education control group (χ2=0.70, df=1, p=0.40).
Maudsley Mother Infant Interaction Scale
There was a significant correlation (r=0.7, p<0.05) between the modified score (sum of five interactive items) on the Mother Infant Interaction Scale (43) and the Hamilton depression scale in 11 patients at the first postpartum visit. The five interactive items of the Mother Infant Interaction Scale are 1) quality of emotional relationship with baby, 2) quality of interaction (i.e., responsiveness and sensitivity to baby by mother), 3) perceived risk to infant from mother, impulse or rejection, 4) psychopathology incorporating baby, and 5) incident affecting baby.
Discussion
Interpersonal psychotherapy resulted in a significant mood improvement relative to the parenting education program control condition based on all mood measures: the Hamilton depression scale, the Beck Depression Inventory, the Edinburgh Postnatal Depression Scale, and CGI symptom recovery. Most notable was the significant difference in the recovery rate between the treatment and control groups on the CGI. In general, the graphic representations for all treatment measures were the same, with a steeper downward curve at week 7 and continued fluctuation through week 12 for the treatment group compared to the plateau of the control group. The similar curve of the graphs suggests similar temporal mood patterns.
All data outcomes were significant except for the Hamilton depression scale recovery scores. This is likely attributed to the weight of Hamilton depression scale somatic symptoms, which are similar to the discomforts of pregnancy. In an effort to correct this similarity, the evaluator asked the participants if they attributed a somatic symptom such as sleeplessness to pregnancy (i.e., from fetal movement) or depression (33). The item was scored if they believed it was a consequence of their depression. In retrospect, we found that differences were not easily determined and likely kept the Hamilton depression scale scores artificially elevated. Our recovery criteria for the Hamilton depression scale was based on a score of ≤6, the recovery score used in the NIMH depression treatment trial, which is not indicative of the pregnant population. Therefore, recovery outcome scores on the Hamilton depression scale may not be a reliable reflection of mood in pregnant women.
Similarly, the Beck Depression Inventory also has a somatic symptom cluster (34). However, the affective items did not compete with the discomforts of pregnancy or the immediate postpartum state. Factor analyses have demonstrated that the Beck Depression Inventory cognitive-affective cluster is as sensitive to depression during pregnancy as the Edinburgh Postnatal Depression Scale, which measures postpartum and antepartum changes (36–38). The removal of the somatic symptom cluster did not reduce the psychometric stability of the Beck Depression Inventory.
The significance of the CGI recovery data is the absence of somatic symptoms. In addition, the clinician-derived measure has demonstrated minimum clinician bias, compared to outcome based on patient ratings (42).
A positive control effect on mood suggests that the control condition was therapeutic for some participants. Our Spanish-speaking therapist was uniquely sensitive to the cultural issues and language of this isolated group of young women, variables that likely contributed to a positive transference and therapeutic benefit. In addition, the control effects for our mood scales (the Edinburgh Postnatal Depression Scale: 11.8%, the Beck Depression Inventory=23.5%, and the Hamilton depression scale=29.4%) were similar to placebo responses in antidepressant medication studies (mean=29.7%, SD=8.3, range=12.5–51.8) (44).
A central point of the study was the selection of a nontherapeutic systematized treatment control condition that enabled careful and sensitive detection of the benefits of interpersonal psychotherapy. Although interpersonal psychotherapy faired significantly better in some studies by use of a waiting-list control (24), the specific benefit of psychotherapy remains undetermined because the condition did not permit examination or detection of the distinct efficacy of the interpersonal psychotherapy treatment itself. In contrast, the parenting education program controls for contact with a professional and duration of sessions as well as nonspecific effects of repeated evaluations, reassurance, and education (variables not controlled in the waiting-list control condition). Control for these measures and nonspecific therapeutic benefits enhanced our ability to assess the singular contribution of a focused interpersonal psychotherapy treatment and support our findings that the mood improvement in our group was attributable to the unique treatment effects of interpersonal psychotherapy.
The high attrition rate (32.0% for control subjects and 16.0% for treatment subjects) is attributed to several factors. Three women left after delivery, and one left after a stillbirth. Second, child care and work demands were obstacles to care for sole-support mothers. The unpredictable nature of pregnancy and young motherhood demanded that the staff be sensitive to the unique needs of young and prospective mothers. Such complications as bed rest and delivery complications required flexible measures such as the use of telephone sessions and mechanisms for child care.
The study was composed of a predominantly fragile group of recent immigrants from the Dominican Republic. Homes were often transient and chaotic, with unpredictable and unstable support systems. For some, circumstances were even more tragic. Partners were involved in drug sales and street crime, and many were incarcerated. Two women left the study when they were reunited with incarcerated partners. Many women were lost to treatment and follow-up because of disconnected telephone numbers.
In all the cases of women who were lost to follow-up, letters were sent with appropriate referrals. Our attrition rate suggests the need for more diligence in follow-up with mothers in less-permanent populations. An additional impediment to treatment may have been the duration of the treatment itself. Sixteen weeks required significant commitment and was a likely contributor to the attrition rate and our limited ability to collect postpartum information. Most interpersonal psychotherapy studies have successfully used treatment durations of 12 weeks (23, 24). Furthermore, mean depression scores improved by the seventh week of interpersonal psychotherapy and fluctuated slightly through week 12, indicating that a 12-week trial is probably sufficient.
One unexpected finding was the high incidence of reported child abuse (47.0%). Women with a history of childhood trauma are more likely to experience depression and suicidal ideation during pregnancy (9). Throughout normal pregnancy, the emotional attachment between mother and infant grows. The mother develops an elaborate internalized image of the fetus, a process conceptualized by Rubin (45) as “binding in”; the fetus becomes part of the self. Consequently, the event of childbirth may exacerbate preexisting conflicts. Because parental and other early relationships may act as an imprint for future relationships, particularly with the infant, this data signals the need for early identification of mothers at risk. A trusting relationship with a therapist may function as a protective factor, providing a high-risk mother with new ways of viewing herself and others.
Although this study was primarily about treatment success, limited information was available for postpartum follow-up. Seven of eight women treated with interpersonal psychotherapy had no postpartum depression, while one treated patient did. Of three available subjects in the control group, two had postpartum depression, and one did not. We can make few inferences from this limited data. However, this information emphasizes the importance of postpartum follow-up and the potential for prevention.
There was a significant correlation of the mother’s improved mood with her ability to interact with the infant. Because this was illustrated at one time point in a small number of women (N=11), the results are not generalizable. However, our findings support those of other researchers (46) and emphasize prevention. Depressed postpartum mothers are less sensitive to infant cues (15) and are therefore less likely to soothe their infants, who tend to be withdrawn and inconsolable (15, 47). Problems in behavior, cognition, and creativity often persist into early childhood and adulthood (48).
Poverty such as that described in our study group is also an important antecedent to postpartum depression (13). Halpern (49) suggested that the presence of one or two difficult conditions, such as infant illness, poverty, and difficult personality, intensifies hostile feelings in the mother and emphasizes the vital need for psychiatric services.
A striking finding was a history of depression in 73.0% of our group (5), data easily obtainable in antepartum clinics and obstetrician/midwife offices. Yet we frequently miss the opportunity for potential intervention and prevention in this accessible study group.
Another unique contribution of this study was the demonstrated feasibility of including a unique cross-section of an understudied population of socioeconomically deprived, poorly educated immigrant women. Although immigrant women comprised most of our group, African American, Caucasian, and Latina women of all socioeconomic backgrounds from the neighboring boroughs of Manhattan and the state of New Jersey were represented.
This study must be considered preliminary and the results considered in view of limitations such as the small group size and the large attrition rate. The benefit of treating mood disorders during pregnancy is far-reaching and extends to the nuclear family, the marital relationship, and parenting potential.
Replication of this study with a larger, more diverse study group will provide generalizability and further information about the effects of ethnicity and socioeconomic status on the causes and treatment outcome of antepartum depression. Mechanisms for diligent follow-up will be in place.
Financial compensation for transportation and child care must be provided to mothers in impoverished or unstable populations in order to facilitate opportunities for treatment and provide greater study feasibility in this underserved population.
Since specific guidelines for effective, safe treatment of antepartum depression do not exist, interpersonal psychotherapy should be a first-line treatment in the hierarchy of treatment guidelines for depressed pregnant women.
 |
 |
Presented in part at the 154th annual meeting of the American Psychiatric Association, New Orleans, May 5–10, 2001; and at the biennial scientific meeting of the Marcé Society for Treatment and Prevention of Postpartum Disorders, Manchester, U.K., Sept., 9–11, 2000. Received Dec. 3, 2001; revision received May 10, 2002; accepted Aug. 27, 2002. From the New York State Psychiatric Institute, College of Physicians and Surgeons, Columbia University. Address reprint requests to Dr. Spinelli, Department of Maternal Mental Health, Columbia University, 1051 Riverside Dr., Unit 123, New York, NY 10032; [email protected] (e-mail). Supported by an NIMH Research Scientist Development Award for Clinicians (grant number MH-01276). The authors thank Myrna Weissman, Ph.D., Katherine Wisner, M.D., Pamela Collins, M.D., Quisqueya Meyreles, C.S.W., and Songmei Wu for their assistance with this article.
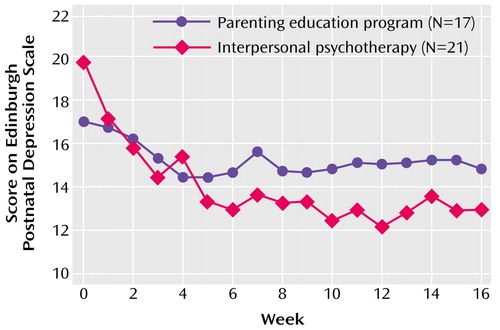
Figure 1. Scores on the Edinburgh Postnatal Depression Scale for Pregnant Women With Major Depression Who Were Randomly Assigned to 16 Weeks of Interpersonal Psychotherapy or a Parenting Education Control Program
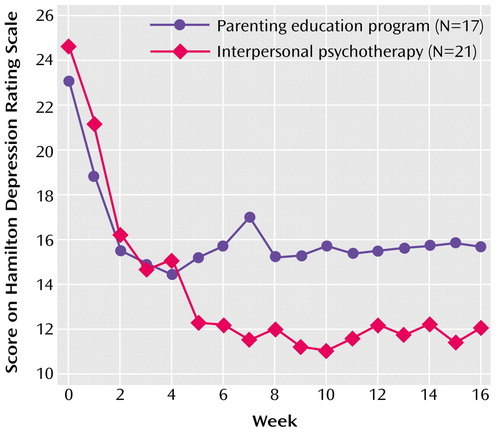
Figure 2. Scores on the Hamilton Depression Scale for Pregnant Women With Major Depression Who Were Randomly Assigned to 16 Weeks of Interpersonal Psychotherapy or a Parenting Education Control Program
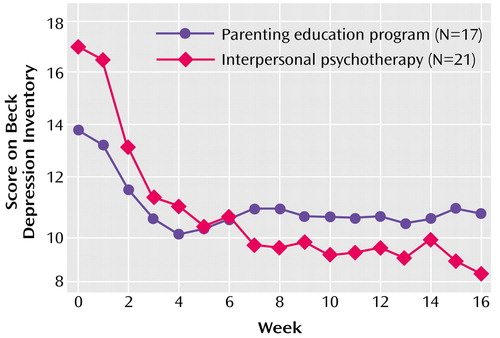
Figure 3. Scores on the Beck Depression Inventory for Pregnant Women With Major Depression Who Were Randomly Assigned to 16 Weeks of Interpersonal Psychotherapy or a Parenting Education Control Program
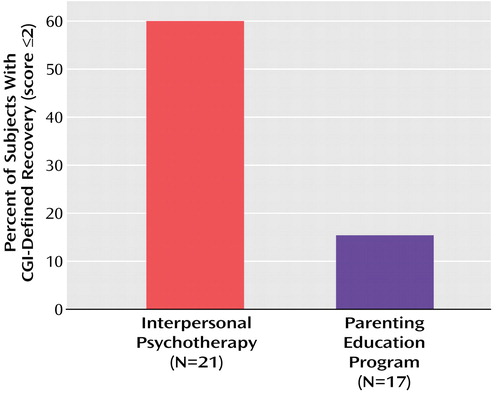
Figure 4. Rates of Recoverya for Pregnant Women With Major Depressive Disorder Who Were Randomly Assigned to 16 Weeks of Interpersonal Psychotherapy or a Parenting Education Control Programb
aRecovery was defined as a score of ≤2 on the Clinical Global Impression (CGI).
bSignificant difference between groups (χ2=6.42, df=1, p<0.02).
1. Gotlib IH, Whiffen VE, Mount JH, Milne K, Cordy NI: Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol 1989; 57:269-274Crossref, Medline, Google Scholar
2. Kumar R, Robson KM: A prospective study of emotional disorders in childbearing women. Br J Psychiatry 1984; 144:35-47Crossref, Medline, Google Scholar
3. O’Hara M, Zekoski EM, Philipps LH, Wright EJ: Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 1990; 99:3-15Crossref, Medline, Google Scholar
4. Evans J, Heron J, Francomb H, Oke S, Golding J: Cohort study of depressed mood during pregnancy and after childbirth. Br Med J 2001; 323:257-260Crossref, Medline, Google Scholar
5. Frank E, Kupfer DJ, Jacob M, Blumenthal SJ, Jarrett DB: Pregnancy-related affective episodes among women with recurrent depression. Am J Psychiatry 1987; 144:288-293Link, Google Scholar
6. Wisner KL, Stowe ZN: Psychobiology of postpartum mood disorders. Brain, Behavior and Reproductive Function 1997; 15:77-90Google Scholar
7. Graff LA, Dyck DG, Schallow JR: Predicting postpartum depressive symptoms and structural modeling analysis. Percept Mot Skills 1991; 73:1137-1138Crossref, Medline, Google Scholar
8. Dimitrovsky L, Perez-Hishberg M, Itskowitz R: Depression during and following pregnancy: quality of family relationships. J Psychol 1986; 12:213-218Google Scholar
9. Farber EW, Herbert SE, Reviere SL: Childhood abuse and suicidality in obstetrics patients in a hospital-based urban prenatal clinic. Gen Hosp Psychiatry 1996; 18:56-60Crossref, Medline, Google Scholar
10. Vega WA, Kolody B, Auuilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduga J: Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry 1998; 55:781-782Crossref, Medline, Google Scholar
11. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
12. Yonkers KA, Ramin SM, Rush AJ, Navarrete CA, Carmody T, March D, Heartwell SF, Leveno KJ: Onset and persistence of postpartum depression in an inner-city maternal health clinic system. Am J Psychiatry 2001; 158:1856-1863Link, Google Scholar
13. Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron R: Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol 1995; 63:445-453Crossref, Medline, Google Scholar
14. Seguin L, Potvin L, St Denis M, Jacinthe L: Chronic stressors, social support, and depression during pregnancy. Obstetric Gynecol 1995; 85:583-589Crossref, Medline, Google Scholar
15. Zuckerman B, Bauchner H, Parker S, Cabral H: Maternal depressive symptoms during pregnancy and newborn irritability. J Dev Behav Pediatr 1990; 114:190-194Google Scholar
16. Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Garite TJ: The association between prenatal stress and infant birth weight and gestational age at birth: a prospective investigation. Am J Obstet Gynecol 1993; 169:858-865Crossref, Medline, Google Scholar
17. Chung T, Lau TK, Alexander SK, Chiu H, Lee D: Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med 2001; 63:830-834Crossref, Medline, Google Scholar
18. Dawson G, Klinger LG, Panagiotides H, Hill D, Spieder S: Frontal lobe activity and affective behavior of infants of mothers with depressive symptoms. Child Dev 1992; 63:725-737Crossref, Medline, Google Scholar
19. Robinson GE, Stewart DE: Postpartum disorders, in Psychological Aspects of Women’s Health. Edited by Stewart DE, Stotland NL. Washington, DC, American Psychiatric Press, 1993, pp 115-138Google Scholar
20. Wisner KL, Gelenberg AJ, Leonard H, Zarin D, Frank E: Pharmacologic treatment of depression during pregnancy. JAMA 1999; 282:1264-1269Crossref, Medline, Google Scholar
21. Oren DA, Wisner KL, Spinelli M, Epperson CN, Peindl KS, Terman JS, Terman M: An open trial of morning light therapy for treatment of antepartum depression. Am J Psychiatry 2002; 159:666-669Link, Google Scholar
22. Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, Glass DR, Pilkonis PA, Leber WR, Docherty JP, Fiester SJ, Parloff MB: National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 1989; 46:971-982Crossref, Medline, Google Scholar
23. O’Hara MW, Stuart S, Gorman LL, Wenzel A: Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000; 57:1039-1045Crossref, Medline, Google Scholar
24. Mufson L, Weissman MM, Moreau D, Garfinkel R: Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999; 56:573-579Crossref, Medline, Google Scholar
25. Brody AL, Saxena S, Stoessel P, Gillies LA, Fairbanks LA, Alborzian S, Phelps ME, Huang S, Wu H, Ho ML, Ho MK, Au SC, Maidment K, Baxter LR: Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy. Arch Gen Psychiatry 2001; 58:641-648Crossref, Medline, Google Scholar
26. Wisner KL, Zarin D, Holmboe E, Appelbaum P, Gelenberg AJ, Leonard HL, Frank E: Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry 2000; 157:1933-1940Link, Google Scholar
27. Spinelli MG: Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry 1997; 154:1028-1030Link, Google Scholar
28. Spinelli MA: Interpersonal psychotherapy for antepartum depressed women, in Management of Psychiatric Disorders in Pregnancy. Edited by Yonkers K, Little B. London, Arnold, 2001, pp 105-121Google Scholar
29. Klerman GL, Weissman MM, Rounsaville BH, Chevron ES: Interpersonal Psychotherapy in Depression. New York, Basic Books, 1984Google Scholar
30. Chevron ES, Rounsaville BJ: Evaluating the clinical skills of psychotherapists: a comparison of techniques. Arch Gen Psychiatry 1983; 40:1129-1132Crossref, Medline, Google Scholar
31. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
32. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56-62Crossref, Medline, Google Scholar
33. Klein MH, Essex MJ: Pregnant or depressed? the effect of overlap between symptoms of depression and somatic complaints of pregnancy on rates of major depression in the second trimester. Depression 1994; 2:1994-1995Crossref, Google Scholar
34. Beck AT: Beck Depression Inventory, in Test Critiques, vol II. Edited by Deyser DJ, Sweetland RC. Kansas City, Mo., Test Corporation of America, 1985, pp 83-87Google Scholar
35. O’Hara MD, Schlechte JA, Lewis DA, Wright EJ: Prospective study of postpartum blues: biologic and psychosocial factors. Arch Gen Psychiatry 1991; 48:801-806Crossref, Medline, Google Scholar
36. Huffman LC, Lamour M, Bryan YE, Pederson FA: Depressive symptomatology during pregnancy and the postpartum period: is the Beck Depression Inventory applicable? J Reprod Infant Psychol 1990; 8:87-97Crossref, Google Scholar
37. Salamero M, Marcos T, Gutierez F, Rebull E: Factorial study of the BDI in pregnant women. Psychol Med 1994, 24:1031-1035Google Scholar
38. Campbell IM, Burgess PM, Finch SJ: A factorial analysis of BDI scores. J Clin Psychol 1984; 40:992-996Crossref, Medline, Google Scholar
39. Harris B, Huckle P, Thomas R, Johns S, Fung H: The use of rating scales to identify postnatal depression. Br J Psychiatry 1989; 154:813-817Crossref, Medline, Google Scholar
40. Murray D, Cox JL: Screening for depression during pregnancy with the Edinburgh Depression Scale. J Reprod Infant Psychol 1990; 8:99-107Crossref, Google Scholar
41. Cox J, Holden J: Perinatal Psychiatry: Use and Misuse of the Edinburgh Postnatal Depression Scale. London, Gaskell (Royal College of Psychiatrists), 1994Google Scholar
42. Petkova E, Quitkin FM, McGrath PJ, Stewart JW, Klein DF: A method to quantify rater bias in antidepressant trials. Neuropsychopharmacology 2000; 22:559-565Crossref, Medline, Google Scholar
43. Kumar R, Hipwell AE: Development of a clinical rating scale to assess mother infant interaction in a psychiatric mother and baby unit. Br J Psychiatry 1996; 169:18-26Crossref, Medline, Google Scholar
44. Walsh BT, Seidman SN, Sysko R, Gould M: Placebo response in studies of major depression: variable, substantial and growing. JAMA 2002; 287:1840-1847Crossref, Medline, Google Scholar
45. Rubin R: Maternal Identity and the Maternal Experience. New York, Springer, 1984Google Scholar
46. Murray L: The impact of postnatal depression on infant development. J Child Psychol Psychiatry 1992; 35:343-361Google Scholar
47. Biringen Z, Robison J: Emotional availability in mother-child interaction: a reconceptualization for research. Am J Orthopsychiatry 1991; 61:258-271Crossref, Medline, Google Scholar
48. Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, Sholomskas D: Children of depressed parents: increased psychopathology and early onset of major depression. Arch Gen Psychiatry 1987; 44:847-853Crossref, Medline, Google Scholar
49. Halpern R: Poverty and infant development, in Handbook of Infant Mental Health. Edited by Zeanah C. New York, Guilford, 1993, pp 73-87Google Scholar



