Depressive and Anxiety Disorders in Women With HIV Infection
Abstract
OBJECTIVE: This study examined whether there were differences in the rate of depressive and anxiety disorders between HIV-infected women (N=93) and a comparison group of uninfected women (N=62). Secondary objectives were to examine correlates of depression in HIV-infected women—including HIV disease stage and protease inhibitor use—and the associations between symptoms of depression or anxiety and other potential predictor variables. METHOD: Subjects underwent extensive semiannual clinical, psychiatric, neuropsychological, and immunological evaluations. Depressive and anxiety disorder diagnoses were assessed by using the Structured Clinical Interview for DSM-IV. Symptoms of depression and anxiety were evaluated with the Hamilton Depression Rating Scale (the 17-item version and a modified 11-item version) and the Hamilton Anxiety Rating Scale, respectively. RESULTS: The rate of current major depressive disorder was four times higher in HIV-seropositive women (19.4%) than in HIV-seronegative women (4.8%). Mean depressive symptom scores on the 17-item Hamilton depression scale also were significantly higher, overall, in the HIV-infected women (mean=8.7, SD=8.0) relative to comparison subjects (mean=3.3, SD=5.8). There was no significant between-group difference in the rate of anxiety disorders. However, HIV-seropositive women had significantly higher anxiety symptom scores (mean=8.8, SD=8.9) than did HIV-seronegative women (mean=3.6, SD=5.5). Both groups had similar substance abuse/dependence histories, but adjusting for this factor had little impact on the relationship of HIV status to current major depressive disorder. CONCLUSIONS: HIV-seropositive women without current substance abuse exhibited a significantly higher rate of major depressive disorder and more symptoms of depression and anxiety than did a group of HIV-seronegative women with similar demographic characteristics. These controlled, clinical findings extend recent epidemiologic findings and underscore the importance of adequate assessment and treatment of depression and anxiety in HIV-infected women.
Increasing evidence suggests that psychosocial factors such as stress and depression may have a harmful impact on the course of many diseases, such as cardiovascular disease and cancer (1–8), and may heighten susceptibility to infectious diseases (9). Recent studies also have examined the effects of depression on HIV disease progression, demonstrating an association between depression and early, as well as late, disease progression in men (10–12) and between depression and mortality in women (13). Alterations in key parameters of cellular immunity have been documented in depressed individuals who are otherwise healthy (14–18). Some studies assessing the effects of stress and depression on immune function in HIV-infected individuals have yielded a positive relationship (19–22), whereas others have found no association (23–25). Thus, the mechanisms by which stress and depression may influence disease progression and mortality in HIV infection remain to be determined.
Psychiatric morbidity has been associated with HIV disease since the beginning of the AIDS epidemic (26). To date, most of the clinical literature has focused on psychiatric issues of HIV-seropositive men (27–33). Previous work has found that HIV-infected gay men have a high prevalence of major depression compared with men of similar age in the U.S. population but no higher than that of HIV-seronegative gay men of similar age (32), a finding that has been confirmed by others (33–35).
There have been little data regarding the prevalence of psychiatric disorders in HIV-infected women, despite the fact that HIV remains a leading cause of death for U.S. women between the ages of 25 and 44 years. HIV also is the leading cause of death among African American women in this age group (26). Estimates of the prevalence of major depressive disorder in HIV-seropositive women vary widely in the literature, with reported prevalence rates that range from 1.9% to 35% in clinical samples (36–38) and from 30% to 60% in community samples (13, 39, 40). In the five-site World Health Organization Neuropsychiatric AIDS study (41), which included men and women, prevalence rates of major depressive disorder ranged from 3.0% to 10.9% in asymptomatic HIV-seropositive subjects and from 4.0% to 18.4% in symptomatic HIV-seropositive subjects. Although women demonstrated higher depression scores on the Montgomery-Åsberg Depression Rating Scale at two of the five sites participating in this multicenter study, data on gender differences for major depressive disorder were not reported.
In the largest U.S. clinical study of non-substance-abusing HIV-seropositive women (N=54), Goggin et al. (36) reported that only 1.9% of the women had major depressive disorder and that 3.7% had dysthymic disorder. In a case series of 38 HIV-seropositive women (42), 14% met DSM-IV criteria for major depressive disorder, 3% had dysthymic disorder, and 48% had substance abuse disorders. In a case series of 17 HIV-seropositive women (37), 29% met DSM-IV criteria for current major depressive disorder, and 18% met criteria for current dysthymic disorder. Studies of HIV-seropositive women that included active intravenous substance abusers have demonstrated an association between current substance abuse, depressive symptoms (38), and major depressive disorder (24), but not HIV status.
Major depression has not been recognized as a complication of protease inhibitor use; however, elevated depressive symptoms have been reported. In a phase III study in patients with HIV infection (43), treatment with amprenavir (a protease inhibitor) in combination with lamivudine and zidovudine was compared with lamivudine and zidovudine treatment alone. In the amprenavir group, 15% of subjects reported depressive or mood symptoms, whereas 4% reported depressive or mood symptoms in the group not treated with amprenavir (43).
The wide range of estimates of major depressive disorder among the available clinical studies of HIV-seropositive women, coupled with recent epidemiological data that depressive symptoms are associated with mortality in HIV-seropositive women, underscore the need for controlled studies to ascertain the rate of depression in HIV-seropositive women and to examine its correlates. The present study addresses these issues.
Specifically, the primary objective was to determine whether there were differences in the rate of depressive and anxiety disorders in a cohort of HIV-infected women relative to a comparison group of uninfected women. Secondary objectives were to examine correlates of depression—including HIV disease stage and protease inhibitor use—and the associations between symptoms of depression or anxiety and other potential predictor variables. Analyses are based on baseline findings collected at entry into a longitudinal cohort study. Female residents of a rural area in Northern Florida who were seropositive for HIV and who were not current substance abusers were compared with a group of HIV-seronegative women who met similar enrollment criteria; both groups were recruited between 1997 and 2000. We examined presentations of depression and anxiety by using comprehensive interview-based diagnostic instruments. Finally, to better characterize mood disturbances in HIV-seropositive women, we assessed the relationship of major depressive disorder, as well as higher depressive symptom scores, to past history of major depressive disorder, stage of HIV illness, and HIV medication use. To our knowledge, this is the largest and the first controlled systematic report in the era of highly active antiretroviral therapy regimens to reflect the distribution of psychiatric disorders in HIV-infected women who are not current substance abusers.
Method
Data were collected as part of an ongoing longitudinal cohort study that is investigating neuropsychiatric, psychosocial, neuroendocrine, and immune aspects of HIV infection in women.
Subjects
HIV-seropositive subjects were recruited from outpatient medical clinics, county health departments, and organizations focusing on HIV illness and care in North Central Florida. A combination of methods was used to identify potential subjects, including community outreach presentations, clinician referrals, word of mouth, and newspaper advertisements. HIV-seronegative subjects were recruited by word of mouth, advertisements, and by inviting enrolled subjects to recruit a friend or neighbor who was interested in the study. Potential subjects were prescreened by telephone to eliminate those who were ineligible. Subjects were enrolled if they were female, aged 18–70 years, and able to communicate in English. HIV serostatus was determined by enzyme-linked immunoabsorbent assay and confirmed by Western blot. Subjects were excluded if the following conditions were found: 1) significant chronic, systemic illness; 2) significant neurologic disorders, including traumatic brain injury; 3) a history of schizophrenia or severe psychotic disorder; 4) subject was pregnant or nursing; or 5) current substance/alcohol abuse or dependence (per DSM-IV). The protocol was reviewed and approved by the institutional review boards of the University of Florida, where clinical assessments were performed, and the University of Pennsylvania. All subjects provided written informed consent and were reimbursed $100.00 for their time and travel expenses.
Procedures
Each subject received a thorough outpatient assessment that included physical and neuropsychological examinations and structured life stress and psychiatric interviews. Subjects also completed a comprehensive set of questionnaires that assessed mood, psychosocial factors, and health habits. Current and lifetime DSM-IV axis I diagnoses were assessed by an experienced research psychiatric clinician with a modified Structured Clinical Interview for DSM-IV (44, 45). All psychiatric measurements were reviewed at diagnostic conferences, and reported findings represent consensus diagnoses. Symptoms of depression and anxiety were evaluated by using the 17-item Hamilton Depression Rating Scale (46) and the Hamilton Anxiety Rating Scale (47). An 11-item Hamilton depression scale also was used to eliminate physical symptoms that might overlap with symptoms of HIV disease, as previously reported (20). Classification of HIV disease status was performed according to the 1993 Centers for Disease Control and Prevention (CDC) criteria for staging of HIV infection (48).
Statistical Analysis
The main outcome measures were 1) presence or absence of current major depressive disorder, 2) other depressive and anxiety disorder diagnoses, 3) depressive symptom scores, and 4) anxiety symptom scores. Secondary analyses included the association of these outcomes with HIV stage, antiretroviral medication, history of major depressive disorder, history of substance abuse, and demographic and socioeconomic status variables (age, race, marital status, education, and gross monthly income). Only HIV-seropositive subjects were included in analyses that examined HIV disease stage and antiretroviral medication use. For each outcome-covariate pair, a univariate model initially was fitted. For discrete outcomes, univariate tests and estimation of odds ratios were performed by using exact odds ratios, confidence intervals, and p values for two-tailed tests of significance, all of which were computed with StatXact version 3.1 (Cytel Software Corporation, Cambridge, Mass.). Because all p values for univariate discrete variables were from Fisher’s exact tests, chi-square statistics are not presented. Subsequently, bivariate models (two covariate models) were fitted with one of the outcome variables as the dependent variable and either HIV status or antiretroviral medication as a covariate along with one of the other covariates listed. In order to ensure accurate estimates and standard errors, we maintained at least a 10 case to one covariate ratio; models with more than two covariates were not fitted because the number of depression cases ranged between 20 and 30 depending on the analysis (49). To assess the dichotomous variable of current major depressive disorder as an outcome measure, logistic models were fitted by using PROC LOGIST in SAS version 8.01 (SAS Institute, Cary, N.C.) for multivariable models, yielding chi-square tests, odds ratios, and confidence intervals. For the continuous variables of Hamilton depression and anxiety scale scores, linear regression, including ANOVA, was used for univariate and multiple variable tests, yielding presentations of t statistics or F statistics, p values, and slopes or mean differences represented by beta and corresponding 95% confidence intervals (CIs). For seronegative versus seropositive comparisons, p values based on normality and constant variance assumptions were confirmed with nonparametric Kruskal-Wallis analyses.
Results
Subjects
Following telephone prescreening, 95% of eligible subjects agreed to participate and completed their baseline visit. The demographic characteristics of the 93 HIV-seropositive and 62 HIV-seronegative women were similar in most respects. Age, race, marital status, number of children and monthly income were similar between the two groups. Both groups of women were relatively young (HIV-seropositive: mean age=37.0 years, SD=9.0; HIV-seronegative: mean age=33.4 years, SD=11.1). Racial distribution was similar, with Caucasian women comprising 39.8% (N=37) of the HIV-seropositive group and 40.3% (N=25) of the HIV-seronegative group. The distribution of ethnic minorities was similar in both groups. Among HIV-seropositive women, 55.9% (N=52) were African American, and 4.3% (N=4) were Hispanic; among HIV-seronegative women, 53.2% (N=33) were African American, 4.8% (N=3) were Hispanic, and one subject (1.6%) was of “other” ethnicity. There were no significant differences in gross monthly income between the two groups of women. The HIV-seropositive women had completed an average of 11.8 years of education (SD=2.1), and the HIV-seronegative women had completed a mean of 12.5 years of education (SD=2.1).
Disease Status in HIV-Seropositive Women
Almost half of the HIV-seropositive women (45.2%, N=42) had stage A HIV infection. Thirty-three women (35.5%) had stage B infection, and a small proportion (N=17, 18.3%) had stage C infection. Thirty-one (33.3%) women were on a regimen of antiretroviral therapy that included taking protease inhibitors, 40 women (43.0%) had medication regimens that did not include protease inhibitors, and 22 women (23.7%) were not taking any medication for HIV infection.
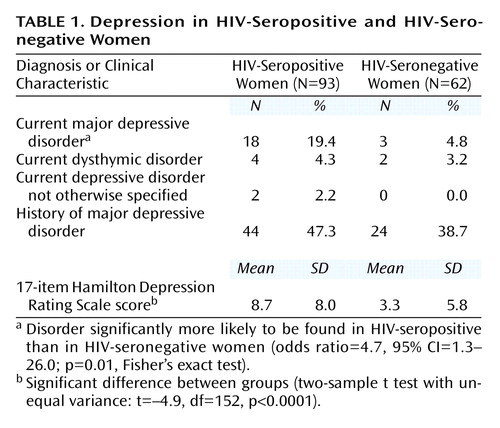
As shown in Table 1, the proportion of women with a diagnosis of current major depressive disorder was four times greater in the HIV-seropositive group than in the HIV-seronegative comparison group, a significantly higher proportion. In contrast, the proportion of women with a history of major depressive disorder was similarly high in the HIV-seropositive group (47.3%) and the HIV-seronegative group (38.7%) (odds ratio=1.4, 95% CI=0.7–2.9; p=0.40, Fisher’s exact test).
Scores on the 17-item and 11-item Hamilton depression scales showed the greater risk and severity of depression among HIV-seropositive women as well. HIV-seropositive women with major depressive disorder had a mean 17-item Hamilton depression scale score of 16.9 (SD=7.3, median=16.0) and a mean 11-item score of 11.3 (SD=5.9, median=11.5), whereas the respective scores for HIV-infected women with no major depressive disorder were 6.5 (SD=5.2, median=6.0) and 4.0 (SD=3.5, median=4.0). Within the HIV-seronegative group, women with major depressive disorder had a mean 17-item Hamilton depression scale score of 17.8 (SD=9.2, median=15.5) and a mean 11-item score of 12.3 (SD=6. 9, median=12.5), whereas the respective scores for HIV-seronegative women with no major depressive disorder were 3.3 (SD=4.5, median=1.5) and 2.2 (SD=3.3, median=1.0).
Factors Associated With Depressive Presentations
Controlling for each baseline covariate separately did not change the association between HIV status and current major depressive disorder. Older age demonstrated a marginal association with current major depressive disorder (odds ratio=1.04, 95% CI=0.997–1.10; p=0.06, Fisher’s exact test). Bivariate models were used to examine the relationship of current major depressive disorder with other variables, holding HIV status constant as the second covariate in the model. Age, race, level of education, income, marital status, and history of major depressive disorder were not significantly associated with current major depressive disorder in any of these analyses.
The proportion of women with dysthymic disorder and depressive disorder not otherwise specified was similar in both HIV-seropositive and seronegative women. As seen in Table 1, mean 17-item Hamilton depression scale scores were higher in the HIV-seropositive group than in the HIV-seronegative group, indicating that the HIV-seropositive women reported significantly more depressive symptoms (beta=5.4, 95% CI=3.1–7.8, where beta is the difference between group means). The 11-item Hamilton depression scale results were similar: HIV-seropositive women had a mean score of 5.8 (SD=5.7) whereas HIV-seronegative women had a mean score of 2.3 (SD=4.3) (t=4.0, df=153, p<0.0001; beta=3.5, 95% CI=1.8–5.1). The Hamilton depression scale results indicate a strong association between HIV status and depressive symptoms in both the univariate analysis above and after adjustment for a history of major depressive disorder (t=4.5, df=152, p<0.0001; beta=5.1, 95% CI=2.8–7.4).
In a series of univariate analyses, higher depressive symptom scores, as per the 17-item Hamilton depression scale, were significantly associated with older age (t=2.3, df=153, p=0.02; beta=0.1, 95% CI=0.02–0.3), Caucasian race (t=2.1, df=153, p=0.04; beta=2.6, 95% CI=0.1–5.0), and less education (t=2.1, df=152, p=0.04; beta=–0.6, 95% CI=–1.2 to –0.02). Marital status and income were not significantly associated with depressive symptoms. After adjustment for age, race, and years of education, HIV status remained significantly associated with depressive symptoms as measured by the 17-item Hamilton depression scale (t=4.1, df=149, p<0.0001; beta=4.8, 95% CI=2.5–7.2).
Anxiety
As seen in Table 2, there was no significant difference between the HIV-seropositive and HIV-seronegative women in the proportion having any of the anxiety disorders. Social phobia was found in 5.4% (N=5) of HIV-seropositive women and in 1.6% (N=1) of HIV-seronegative women, but this difference did not reach statistical significance. When any anxiety disorder was considered, 10.8% (N=10) of the HIV-seropositive women and 6.5% (N=4) of the HIV-seronegative women had at least one anxiety disorder diagnosis, a difference that was not statistically significant (odds ratio=1.7, 95% CI=0.5–7.8; p=0.54, Fisher’s exact test). Nevertheless, HIV-seropositive women had higher scores on the 14-item Hamilton anxiety scale than did the HIV-seronegative women (beta=5.2, 95% CI=2.7–7.7). Thus, relative to HIV-seronegative women, HIV-seropositive women had higher levels of anxiety symptoms but similar rates of anxiety disorders.
Substance Abuse and Dependence
A large proportion of women in both groups reported a history of substance abuse or dependence. The proportion of women with a history of substance abuse or dependence was higher in the HIV-seropositive group (50.5%, N=47) than in the HIV-seronegative women (30.6%, N=19), a difference that was statistically significant (odds ratio=2.3, 95% CI=1.2–4.6; p=0.02, Fisher’s exact test). Adjusting for history of substance abuse or dependence did not substantively alter the relationship of positive HIV serostatus and current major depressive disorder from the aforementioned unadjusted odds ratio of 4.7 (odds ratio=4.0, 95% CI=1.1–14.5; χ2=4.4, df=1, p=0.04).
Antiretroviral Medication and Depression
To understand further the association of antiretroviral medication use and depression, we investigated the relationships between use of specific classes of antiretroviral medication and current major depressive disorder. Among the HIV-seropositive women who were receiving protease inhibitor therapy (N=31), nine women (29.0%) had a diagnosis of major depressive disorder. Among the 62 women who were receiving antiretroviral treatment that did not include a protease inhibitor or who were not taking any antiretroviral therapy medication, the proportion of women with major depressive disorder (14.5%, N=9) was lower, but this difference was not statistically significant (odds ratio=2.4, 95% CI=0.7–7.8; p=0.10, Fisher’s exact test). Mean 17-item Hamilton depression scale scores were higher in the 31 women receiving protease inhibitor therapy (mean=10.6, SD=9.1) than in the 62 women who were taking other antiretroviral medications or no medications (mean=7.8, SD=7.3), but this difference also was not statistically significant (t=1.6, df=91, p=0.10; beta=2.8, 95% CI=–0.6 to 6.2). In a univariate analysis of those taking antiretroviral therapy, protease inhibitor use was associated with current major depressive disorder (odds ratio=8.6, 95% CI=1.0–394.1; p=0.05, Fisher’s exact test); however, this association did not remain significant after adjustment for stage of HIV illness (odds ratio=5.7, 95% CI=0.6–290.1; χ2=1.6, df=1, p=0.20). The proportion of HIV-seropositive women taking antiretroviral therapy with major depressive disorder did not significantly differ by CDC stage (stage A: 18% [N=6 of 33], stage B: 33% [N=11 of 33], stage C: 25% [N=1 of 4]). Furthermore, for the entire group of HIV-seropositive women, the proportion of women with major depressive disorder did not significantly differ by CDC stage (stage A: 15% [N=7 of 48], stage B: 28% [N=11 of 39], stage C: 20% [N=1 of 5]). The mean 17-item Hamilton depression scale scores for those women in stages A, B, and C were 7.5, 10.0, and 9.8, respectively (F=1.16, df=2, 89, p=0.30); the corresponding 11-item Hamilton depression scale scores were 5.1, 6.5, and 6.6 (F=0.7, df=2, 89, p=0.50).
Protease Inhibitors and Anxiety
Use of protease inhibitors was not associated with anxiety disorders or symptoms. In a univariate analysis, Hamilton anxiety scale scores were associated with protease inhibitor use (t=2.07, df=152, p=0.02; beta=5.47, 95% CI=0.03–10.42) but not after adjustment for HIV disease stage (t=0.41, df=151, p=0.34; beta=1.6, 95% CI=–1.8 to 5.0).
Discussion
We found a high rate of current major depressive disorder (19.4%) among the HIV-seropositive women at entry into our cohort study. Interpreting these findings in the context of reported work in this field is complicated by the small number of published studies of mood disorders in women and the diverse demographic characteristics, assessment methods, and small sample sizes across the reported clinical studies. The low prevalence rates for depressive disorder diagnoses (1.9%) reported by Goggin et al. (36) are similar to Brown et al.’s finding of a 5% rate of major depressive disorder in a sample of 43 non-substance-using women in the military (50). Investigators studying substance-abusing populations have reported rates ranging from 20% to 35% (38, 42). However, these studies were limited by the lack of a comparison group of HIV-seronegative women. Goggin et al. (36) attributed their low depressive disorder rates to the absence of current substance use/dependence. However, our subjects also had no current substance use/dependence, yet they had a much higher rate of major depressive disorder relative to population norms for women in this age range. The proportion of HIV-seronegative women in our cohort who had current major depressive disorder was 4.8%, which is similar to the 1-year prevalence rate in women seen in the Epidemiologic Catchment Area study (4.0%) (51) and slightly less than the 30-day prevalence rate seen in the National Comorbidity Survey (6.4%) (52).
The high rate of past major depressive disorder found in our cohort (47.3% in HIV-seropositive and 38.7% in HIV-seronegative subjects) is consistent with the 22.1%–61.0% lifetime prevalence of mood disorders seen in other studies of HIV-seropositive and at-risk HIV populations (32, 41, 53–56) and much higher than the lifetime prevalence of major depressive disorder reported for women in the Epidemiologic Catchment Area study (7.0%) (51) and the National Comorbidity Survey (21.3%) (52). Thus, consistent with other studies of HIV-seropositive women and women at risk for HIV, our cohort had a much higher lifetime prevalence of major depressive disorder.
Ickovics and colleagues (13) recently reported adverse health effects associated with depressive symptoms in longitudinal analyses from the HIV Epidemiology Research Study, a large epidemiologic cohort study of HIV-infected women. Using a screening tool for assessment of depressive symptoms (the CES-D Scale), the HIV Epidemiology Research Study investigators found that after clinical, substance abuse, and sociodemographic characteristics were controlled, HIV-infected women with chronic or intermittent depressive symptoms over a 7-year period were at greater risk of HIV disease progression (decline in CD4 cell count and death) than were women with limited or no depressive symptoms. Unlike our study, the HIV Epidemiology Research Study had no control group. Forty-six percent of women in the HIV Epidemiology Research Study cohort reported substance abuse during the study, a factor that may have contributed to the high proportion of women classified as having chronic (42%) or intermittent (35%) depressive symptoms. Furthermore, the actual prevalence of major depressive disorder could not be assessed, given that self-report measures of depressive symptoms are standard in community-based, epidemiologic investigations. Thus, controlled clinical studies, like the present study, are needed to determine a more reliable estimate of the frequency of major depressive disorder among HIV-infected women.
We found a higher rate of anxiety symptoms in HIV-seropositive women. Despite this observation, the proportion of women with anxiety disorders was not significantly different between the HIV-seropositive and HIV-seronegative groups. There are few studies regarding the prevalence of anxiety disorders in HIV-seropositive populations, particularly in women. Goggin et al. (36) found a rate of 1.9% for generalized anxiety disorder in HIV-seropositive women. Among HIV-seropositive men in the United States, there was no difference in the prevalence rate of current anxiety disorders between HIV-seropositive men and a comparison group of uninfected men (4% had social phobia, 3% had specific phobias, 2% had obsessive-compulsive disorder, 2% generalized anxiety disorder, and 12% any anxiety disorder) (57). In a case series from a clinic population in France, 7.7% of patients had diagnoses of anxiety disorders according to DSM-IV criteria (58). Thus, although anxiety symptoms were seen more often in the HIV-seropositive women, anxiety disorder diagnoses were not. The 10.8% of HIV-seropositive women with any anxiety disorder observed in our study group is consistent with that observed in other cohorts of HIV-seropositiveindividuals.
We explored the possibility that the higher rate of major depressive disorder in our cohort of HIV-seropositive women was related to the use of protease inhibitors. Although we found that 29% of HIV-seropositive women taking protease inhibitors had major depressive disorder compared with 14.5% in women taking no antiretroviral therapy or a medication regimen that did not include protease inhibitors, we did not find a statistically significant association of protease inhibitor use and major depressive disorder. One possible explanation for this may be that the small number of cases of major depressive disorder in the cohort of HIV-seropositive women did not provide adequate power to detect significant differences. However, two recent studies focusing on men found positive effects on mood in individuals treated with protease inhibitors and no increase in depression (59, 60). The present study may suggest the need for further investigation of the possible association of protease inhibitor use and depression in women.
Several potential methodological limitations of the study are recognized. It is possible that features of the recruitment process introduced a bias (toward more or less psychopathology) into one or both samples. For example, identifying comparison subjects through friendships with participants may bias toward better mental health, since individuals with someone to refer may have a larger or more active network of social support from which to recruit.
Psychiatric diagnoses were confirmed at consensus conferences by using an inclusive diagnostic approach, and interviewers as well as consensus reviewers were not blinded regarding subject serostatus. In our experience, we have not found a satisfactory way to maintain such a blind and achieve validation of the consensus diagnosis. Thus, the potential for a bias in psychiatric diagnoses is small but possible.
Another potential methodological difficulty in studies of depression in populations with known medical illness is to distinguish symptoms of depression from symptoms of medical illness (61). In this and previous studies of HIV populations, to address this possible confounding, we have analyzed symptom scores from both the 17-item Hamilton scale and a modified 11-item Hamilton scale that deletes six items of physical symptoms potentially related to HIV disease (20). In the present study, HIV-seropositive women still had higher scores on the 11-item Hamilton depression scale than did the HIV-seronegative women, suggesting that depression was not confounded by HIV disease symptoms.
Finally, it should be recognized that the participants were women who were residing in rural Florida, a nonepicenter location, and represented two predominant racial groups, African American and Caucasian. Thus, this study cannot necessarily be generalized to Hispanic, Asian, or urban populations, nor to active substance abusers.
Several strengths of the present study should be noted. Study participants underwent comprehensive interview-based assessments for mood and anxiety; structured, standardized psychiatric instruments and consensus diagnoses were used. Because one of the general aims of the longitudinal cohort study was the determination of depression’s effects on immune function, we excluded subjects with current alcohol or substance abuse/dependence and included a comparison group of HIV-seronegative women. Thus, the rate of depression found in this cohort was not confounded by active substance abuse.
Women represent an increasing percentage of the HIV epidemic in the United States, and there is a paucity of information on psychiatric diagnoses in this population. The baseline findings from this ongoing longitudinal cohort study suggest that HIV-seropositive women are at significantly greater risk of major depressive disorder compared with a demographically similar group of HIV-seronegative women. To our knowledge, this is the largest clinical study and the first controlled investigation of depression and anxiety in HIV-infected women who are not active substance abusers. Our finding of higher rates of current major depressive disorder in HIV-seropositive women who are not current substance abusers requires confirmation from other studies of HIV-infected women receiving current regimens of antiretroviral therapy. It is noteworthy that the rate of major depressive disorder in the present study of HIV-seropositive women is consistent with reported rates of major depressive disorder in women with cancer (62) as well as in women with cardiovascular disease (6). Furthermore, the finding that nearly 20% of HIV-seropositive women have diagnosable major depressive disorder is consistent with recent epidemiologic data documenting that 42% of HIV-seropositive women experience chronic depressive symptoms (13). Our findings suggest that HIV-infected women should be screened and assessed for depression. Further research is required to determine if effective antidepressant treatment is associated with improved survival in HIV disease progression, in addition to relief of depression and improved quality of life.
 |
 |
Presented in part at the 37th annual meeting of the American College of Neuropsychopharmacology, Los Croabas, Puerto Rico, Dec. 14–18, 1998, and the 39th annual meeting of the American College of Neuropsychopharmacology, San Juan, Puerto Rico, Dec. 10–14, 2000. Received May 22, 2001; revision received Oct. 12, 2001; accepted Nov. 27, 2001. From the Center for Clinical Epidemiology and Biostatistics and the Departments of Psychiatry, Pediatrics, Medicine, and Neuroscience, University of Pennsylvania School of Medicine; and the McKnight Brain Institute, University of Florida College of Medicine, Gainesville. Address reprint requests to Dr. Evans, Department of Psychiatry, University of Pennsylvania School of Medicine, 305 Blockley Hall, Philadelphia, PA 19104-6021; [email protected] (e-mail). Supported by NIMH grants MH-55454 (Dr. Evans) and MH-01350 (Dr. Morrison).
1. Spiegel D, Kraemer HC, Bloom JR, Gottheil E: Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 1989; 2:888-891Crossref, Medline, Google Scholar
2. Ramirez AJ, Craig TJK, Watson JP, Fentiman IS, North WRS, Rubens RD: Stress and relapse of breast cancer. Br Med J 1989; 298:291-293Crossref, Medline, Google Scholar
3. Frasure-Smith N, Lesperance F, Talajic M: Depression following myocardial infarction: impact on 6-month survival. Circulation 1993; 270:1819-1825Google Scholar
4. Frasure-Smith N, Lesperance F, Talajic M: Depression and 18-month prognosis after myocardial infarction. Circulation 1995; 91:999-1005Crossref, Medline, Google Scholar
5. Fawzy FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D, Fahey JL, Morton DL: Malignant melanoma: effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch Gen Psychiatry 1993; 50:681-689Crossref, Medline, Google Scholar
6. Musselman DL, Evans DL, Nemeroff CB: The relationship of depression to cardiovascular disease: epidemiology, biology and treatment. Arch Gen Psychiatry 1998; 55:580-592Crossref, Medline, Google Scholar
7. Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ: Association between depression and mortality in older adults. Arch Intern Med 2000; 160:1761-1768Crossref, Medline, Google Scholar
8. Faller H, Bulzebruck H, Drings P, Lang H: Coping, distress, and survival among patients with lung cancer. Arch Gen Psychiatry 1999; 55:756-762Crossref, Google Scholar
9. Glaser R, Rabin B, Chesney M, Cohen S, Natelson B: Stress-induced immunomodulation: implications for infectious diseases? JAMA 1999; 281:2268-2270Crossref, Medline, Google Scholar
10. Page-Schaeffer K, Delonenze GN, Satariano WA, Winkelstein W: Comorbidity and survival in HIV-infected men in the San Francisco Men’s Health Survey. Ann Epidemiol 1996; 6:420-430Crossref, Medline, Google Scholar
11. Mayne TJ, Vittinghoff E, Chesney MA, Barrett DC, Coates TJ: Depressive affect and survival among gay and bisexual men infected with HIV. Arch Intern Med 1996; 156:2233-2238Crossref, Medline, Google Scholar
12. Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, Cai J, Folds JD, Evans DL: Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosom Med 1999; 61:397-406Crossref, Medline, Google Scholar
13. Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, Moore J (HIV Epidemiology Research Study Group): Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women. JAMA 2001; 285:1466-1474Crossref, Medline, Google Scholar
14. Evans DL, Leserman J, Pederson CA, Golden RN, Lewis MH, Folds JA, Ozer H: Immune correlates of stress and depression. Psychopharmacol Bull 1989; 25:319-324Medline, Google Scholar
15. Evans DL, Folds JD, Comer S, Golden RN, Pederson CA, Corrigan M, Gilmore JH, Silva SG, Quade D, Ozer H: Circulating natural killer cell phenotypes in males and females with major depression: relation to cytotoxic activity and severity of depression. Arch Gen Psychiatry 1992; 49:388-395Crossref, Medline, Google Scholar
16. Stein M, Miller AH, Trestman RL: Depression, the immune system and health and illness. Arch Gen Psychiatry 1991; 48:171-177Crossref, Medline, Google Scholar
17. Herbert TB, Cohen S: Depression and immunity: a meta-analytical review. Psychol Bull 1993; 113:472-486Crossref, Medline, Google Scholar
18. Reichlin S: Mechanisms of disease: neuroendocrine-immune interactions. N Engl J Med 1993; 329:1246-1253Crossref, Medline, Google Scholar
19. Evans DL, Leserman J, Perkins DO, Stern RA, Murphy C, Tamul K, Liao D, van der Horst CM, Hall CD, Folds JD, Golden RN, Petitto JM: Stress-associated reductions of cytotoxic T lymphocytes and natural killer cells in asymptomatic HIV infection. Am J Psychiatry 1995; 152:543-550Link, Google Scholar
20. Leserman J, Petitto JM, Perkins DO, Folds JD, Golden RN, Evans DL: Severe stress, depressive symptoms, and changes in lymphocyte subsets in human immunodeficiency virus-infected men: a 2-year follow-up study. Arch Gen Psychiatry 1997; 54:279-285Crossref, Medline, Google Scholar
21. Burack JH, Barrett DC, Stall RD, Chesney MA, Ekstrand ML, Coates TJ: Depressive symptoms and CD4 lymphocyte decline among HIV-infected men. JAMA 1993; 270:2568-2573Crossref, Medline, Google Scholar
22. Kemeny ME, Weiner H, Taylor SE, Schneider S, Visscher B, Fahey JL: Repeated bereavement, depressed mood, and immune parameters in HIV-seropositive and seronegative gay men. Health Psychol 1994; 13:14-24Crossref, Medline, Google Scholar
23. Perry S, Fishman B, Jacobsberg L, Frances A: Relationships over 1 year between lymphocyte subsets and psychosocial variables among adults with infection by human immunodeficiency virus. Arch Gen Psychiatry 1992; 49:396-401Crossref, Medline, Google Scholar
24. Lipsitz JD, Williams JB, Rabkin JG, Remien RH, Bradbury M, el Sadr W, Goetz R, Sorrell S, Gorman JM: Psychopathology in male and female intravenous drug users with and without HIV infection. Am J Psychiatry 1994; 151:1662-1668Link, Google Scholar
25. Rabkin JG, Williams JB, Remien RH, Goetz R, Kertzner R, Gorman JM: Depression, distress, lymphocyte subsets and human immunodeficiency virus symptoms on two occasions in HIV-positive homosexual men. Arch Gen Psychiatry 1991; 48:111-119Crossref, Medline, Google Scholar
26. Evans DL, Mason K, Bauer R, Leserman J, Pettito J: Neuropsychiatric manifestations of HIV-1 infection and AIDS, in Neuropsychopharmacology: The Fifth Generation of Progress. Edited by Charney D, Coyle J, Davis K, Nemeroff C. New York, Raven Press (2002)Google Scholar
27. Rabkin JG, Wagner GJ, Rabkin R: Fluoxetine treatment for depression in patients with HIV and AIDS: a randomized, placebo-controlled trial. Am J Psychiatry 1999; 156:101-107Link, Google Scholar
28. Dickey WC, Dew MA, Becker JT, Kingsley L: Combined effects of HIV-infection status and psychosocial vulnerability on mental health in homosexual men. Soc Psychiatry Psychiatr Epidemiol 1999; 34:4-11Crossref, Medline, Google Scholar
29. Zisook S, Peterkin J, Goggin KJ, Sledge P, Atkinson JH, Grant I (HIV Neurobehavioral Research Center Group): Treatment of major depression in HIV-seropositive men. J Clin Psychiatry 1998; 59:217-224Crossref, Medline, Google Scholar
30. Griffin KW, Rabkin JG, Remien RH, Williams JB: Disease severity, physical limitations and depression in HIV-infected men. J Psychosom Res 1998; 44:219-227Crossref, Medline, Google Scholar
31. Lyketsos CG, Hoover DR, Guccione M, Dew MA, Wesch JE, Bing EG, Treisman GJ: Changes in depressive symptoms as AIDS develops. Am J Psychiatry 1996; 153:1430-1437Link, Google Scholar
32. Perkins DO, Stern RA, Golden RN, Murphy C, Naftolowitz D, Evans DL: Mood disorders in HIV infection: prevalence and risk factors in a nonepicenter of the AIDS epidemic. Am J Psychiatry 1994; 151:233-236Link, Google Scholar
33. Rabkin JG, Goetz RR, Remien RH, Williams JBW, Todak G, Gorman JM: Stability of mood despite HIV illness progression in a group of homosexual men. Am J Psychiatry 1997; 154:231-238Link, Google Scholar
34. Atkinson J, Grant I, Kennedy CJ, Richman DD, Spector SA, McCutcheon JA: Prevalence of psychiatric disorders among men infected with human immunodeficiency virus: a controlled study. Arch Gen Psychiatry 1988; 45:859-864Crossref, Medline, Google Scholar
35. Williams JBW, Rabkin JG, Remien RH, Gorman JM, Ehrhardt AA: Multidisciplinary baseline assessment of homosexual men with and without human immunodeficiency virus infection: standardized clinical assessment of current and lifetime psychopathology. Arch Gen Psychiatry 1991; 48:124-130Crossref, Medline, Google Scholar
36. Goggin K, Engelson ES, Rabkin JG, Kotler DP: The relationship of mood, endocrine, and sexual disorders in human immunodeficiency virus positive (HIV+) women: an exploratory study. Psychosom Med 1998; 60:11-16Crossref, Medline, Google Scholar
37. McDaniel JS, Fowlie E, Summerville MB, Farber EW, Cohen-Cole SA: An assessment of rates of psychiatric morbidity and functioning in HIV disease. Gen Hosp Psychiatry 1995; 17:346-352Crossref, Medline, Google Scholar
38. Boland RJ, Moore J, Schuman P: The longitudinal course of depression in HIV-infected women (abstract). Psychosomatics 1999; 40:160Google Scholar
39. Moore J, Schuman P, Schoenbaum E, Boland B, Solomon L, Smith D: Severe adverse life events and depressive symptoms among women with, or at risk for, HIV infection in four cities in the United States of America. AIDS 1999; 13:2459-2468Crossref, Medline, Google Scholar
40. Smith DK, Moore JS, Warren D, Solomon L, Schuman P, Stein M, Greenberg B: The design, participants, and selected early findings of the HIV Epidemiology Research Study, in Women and AIDS: Coping and Care. Edited by O’Leary A, Jemott LS. New York, Plenum, 1996, pp 185-206Google Scholar
41. Maj M: Depressive syndromes and symptoms in subjects with human immunodeficiency virus (HIV) infection. Br J Psychiatry Suppl 1996; 30:117-122Medline, Google Scholar
42. Taylor ER, Amodei N, Mangos R: The presence of psychiatric disorders in HIV-infected women. J Couns Dev 1996; 74:345-351Crossref, Google Scholar
43. Adverse Events and Laboratory Abnormalities Associated With the Use of Agenerase in Adult and Pediatric Patients. Research Triangle Park, NC, Glaxo Wellcome, 2000Google Scholar
44. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
45. Perkins DO, Dickinson JA, Evans DL: SCID-RDC: DSM-III-R and RDC Integrated Interview, in 1990 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1990, p 75Google Scholar
46. Hamilton M: Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 1967; 6:278-296Crossref, Medline, Google Scholar
47. Hamilton M: The assessment of anxiety states by rating. Br J Med Psychol 1959; 32:50-55Crossref, Medline, Google Scholar
48. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morb Mortal Wkly Rep 1992; 41(RR-17):1-19Google Scholar
49. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR: A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49:1373-1379Crossref, Medline, Google Scholar
50. Brown GR, Kendall S, Ledsky R: Sexual dysfunction in HIV-seropositive women without AIDS. J Psychol Hum Sexuality 1995; 7:73-97Crossref, Google Scholar
51. Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C: Affective disorders, in Psychiatric Disorders in America: The Epidemiological Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 53-80Google Scholar
52. Blazer DG, Kessler RC, McGonagle KA, Swartz MS: The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry 1994; 151:979-986Link, Google Scholar
53. Rosenberger PH, Bornstein RA, Nasrallah HA: Psychopathology in human immunodeficiency virus infection: lifetime and current assessment. Compr Psychiatry 1993; 34:150-158Crossref, Medline, Google Scholar
54. Rabkin JG, Ferrando SJ, Jacobsberg LB, Fishman B: Prevalence of axis I disorders in an AIDS cohort: a cross-sectional, controlled study. Compr Psychiatry 1997; 38:146-154Crossref, Medline, Google Scholar
55. Dew MA, Becker JT, Sanchez J, Caldararo R, Lopez OL, Wess J, Dorst SK, Banks G: Prevalence and predictors of depressive, anxiety and substance use disorders in HIV-infected and uninfected men: a longitudinal evaluation. Psychol Med 1997; 27:395-409Crossref, Medline, Google Scholar
56. Kelly B, Raphael B, Judd F, Perdices M, Kernutt G, Burrows GD, Burnett PO, Dunne M: Psychiatric disorder in HIV infection. Aust NZ J Psychiatry 1998; 32:441-453Crossref, Medline, Google Scholar
57. Sewell MC, Goggin KJ, Rabkin JG, Ferrando SJ, McElhiney MC, Evans S: Anxiety syndromes and symptoms among men with AIDS. Psychosomatics 2000; 41:294-300Crossref, Medline, Google Scholar
58. Kantin S, Kolb MA, Hudzik G: Psychiatric disorders in patients with HIV infection (abstract). International Conference on AIDS 1998:483Google Scholar
59. Low-Beer S, Chan K, Yip B, Wood E, Montaner JSG, O’Shaughnessy MV, Hogg RS: Depressive symptoms decline among persons on HIV protease inhibitors. J Acquir Immune Defic Syndr 2000; 23:295-301Crossref, Medline, Google Scholar
60. Rabkin JG, Ferrando SJ, Lin SH, Sewell M, McElhiney M: Psychological effects of HAART: a 2-year study. Psychosom Med 2000; 62:413-422Crossref, Medline, Google Scholar
61. Perkins DO, Leserman J, Stern RA, Baum SF, Liao D, Golden RN, Evans DL: Somatic symptoms and HIV infection: relationship to depressive symptoms and indicators of HIV disease. Am J Psychiatry 1995; 152:1776-1781Link, Google Scholar
62. Evans DL, McCartney CF, Nemeroff CB, Raft D, Quade D, Golden RN, Haggerty JJ Jr, Holmes V, Simon JS, Droba M: Depression in women treated for gynecological cancer: clinical and neuroendocrine assessment. Am J Psychiatry 1986; 143:447-452Link, Google Scholar



