White Matter Lesions and Season of Birth of Patients With Bipolar Affective Disorder
Abstract
OBJECTIVE: It is established that patients with bipolar disorder have an excess of births in winter or early spring. The authors investigated a link between season of birth and white matter lesions with magnetic resonance imaging (MRI). METHOD: T2-weighted and proton density MRI scans were examined for 79 patients with bipolar disorder (DSM-IV) for the presence of deep subcortical and periventricular white matter lesions. The birth seasons of patients with white matter lesions were compared with those of the general population. RESULTS: Thirteen subjects exhibited deep subcortical white matter lesions, of whom nine (69.2%) were born in the winter months (January to March). Seven of these patients remained symptomatic, despite adequate treatment for more than 2 years. CONCLUSIONS: Birth season, illness outcome, and deep subcortical white matter lesions appear to be closely linked. Deep subcortical white matter lesions may be a marker of a toxic or infective insult in utero.
The 8% excess of winter births among patients with schizophrenia remains one of the best-established findings of psychiatric epidemiology. Compelling evidence has been presented that patients with bipolar disorder show a 5.8% excess of winter births (1). White matter lesions on magnetic resonance imaging (MRI) scans have been reported in 5%–60% of patients with bipolar disorder. They are 3.3 times more likely to be found in bipolar patients than in comparison subjects (2), and their presence may indicate a poorer clinical outcome (3, 4). In this article we report a link between winter birth (January to March) and the presence of white matter lesions on MRI scans in patients with bipolar disorder.
Method
Seventy-nine patients with bipolar disorder (30 men and 49 women, mean age=35.4 years, SD=8.6) were recruited from general hospital psychiatric clinics in the Tyneside region of the United Kingdom. The names of the patients with bipolar disorder were forwarded to us by their psychiatrists. After a review of case notes, the patients with bipolar disorder (I or II) who met inclusion criteria were subject to clinical interview, which incorporated the Structured Clinical Interview for DSM-IV Axis I Disorders (5), to confirm their diagnosis. Rigorous criteria were formulated to exclude all patients with other psychiatric and physical disorders, including drug and alcohol abuse, cardiovascular or cerebrovascular disorders, and other significant medical conditions and treatments, e.g., taking steroids that influence mood. After a complete description of the study was given to the subjects, written informed consent to participate was obtained. The majority of the study patients (N=64, 81.0%) were euthymic, with a mean Beck Depression Inventory score of 9.0 (SD=1.6), whereas 15 (19.0%) had been symptomatic (Beck Depression Inventory mean score=16.0, SD=1.8) for more than 2 years.
A comparison group of 33 healthy subjects (16 men and 17 women, mean age=33.1 years, SD=12.5) who met the same exclusion criteria as the patients were investigated. MRIs were performed with a GE 0.5-T MR Max Plus Scanner (General Electric, Milwaukee). T2-weighted axial MRI scans (7 mm thick, T2 weighted, TR=2300, TE=25, 100 msec) and proton density scans were examined for the presence of white matter lesions, which were categorized as deep subcortical or periventricular and graded according to the scheme of Fazekas et al. (6). Expected relative monthly birth rates were calculated from monthly live birth rates in England and Wales from 1955 to 1980 (Central Statistical Office). These were compared to experimental study data by using chi-square goodness-of-fit analysis. For subjects with deep subcortical and periventricular white matter lesions, exact calculations based on binomial distributions were used to calculate the probabilities of obtaining the observed distributions among birth seasons of the subjects with these abnormalities (7).
Results
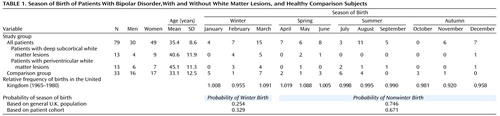
The principal findings of the study are shown in Table 1, which provides the numbers of patients in particular categories who were born during each month of the year. The birth seasons of the bipolar group (N=79) did not differ significantly from the those of the general population (goodness-of-fit χ2=3.56, df=3, p=0.32). The mean ages of the subjects born in each season (January to March: mean=35.7 years, SD=11.6, April to June: mean=35.9, SD=10.9, July to September: mean=35.0, SD=12.4, and October to December: mean=36.7, SD=10.4) did not differ significantly (analysis of variance, F=0.06, df=3, 77, p=0.98).
The probability of a subject being born during the winter months (January to March) from the frequencies of monthly live births (Table 1) for England and Wales from 1965 to 1980 was 0.254, and the probability of a nonwinter birth was 0.746 (1 – the probability of a winter birth). Table 1 shows that of the 13 patients with deep subcortical white matter lesions, nine (69.2%) were born during the winter months. When we compared this with the probability values for winter and nonwinter births from the U.K. population, the probability of 9 or more of the 13 subjects with deep subcortical white matter lesions having a winter birth was p=0.001 (exact calculation, binomial distribution, probability of winter birth=0.256) (i.e., p<0.002 was considered significant). Seven (77.8%) of the nine subjects with deep subcortical white matter lesions had an bipolar illness with a poor treatment outcome and had been continuously unwell for 2 or more years.
Although the birth seasons of the patients with bipolar disorder did not differ significantly from those in the general U.K. population, an inspection of Table 1 reveals that there was a relative excess of winter births, and there was a relative paucity of births during the autumn. On the basis of the birth dates of our bipolar patients, it was possible to calculate an experimental winter birth probability of 0.329 (i.e., 26 of 79) and a probability of nonwinter birth of 0.671 (53 of 79). When we used these figures, the probability of nine or more subjects with deep subcortical white matter lesions having a winter birth was p=0.02 (exact calculation, binomial distribution, probability of a winter birth=0.329), i.e., significant. Thus, we concluded that there was a significant link between birth season and the presence of deep subcortical white matter lesions in the patients with bipolar disorder that was independent of any tendency for winter births in our group of bipolar patients.
The link between periventricular white matter lesions and a winter birth is equivocal. Seven (53.8%) of 13 subjects with periventricular white matter lesions had a winter birth. With the probability of a winter birth at 0.254 in the U.K. population, the probability of 7 or more of 13 subjects with periventricular white matter lesions having a winter birth was significant (p=0.02, exact calculation, binomial distribution, probability of a winter birth=0.254), but this significance disappeared (p=0.11, exact calculation, binomial distribution, probability of a winter birth=0.329) when the likelihood for excess winter births in the cohort was taken into account.
None of our comparison group of 33 subjects had deep subcortical white matter lesions, and only three had periventricular white matter lesions, despite many having a winter birth. The three comparison subjects with periventricular white matter lesions showed relatively minor abnormalities and Fazekas et al. grades of 1, 1, and 2. Their ages were 60, 49, and 53, respectively, with birth seasons of winter, spring, and autumn. The paucity of white matter lesions in the comparison group indicates the success of our study criteria in excluding those with white matter lesions owing to causes other than bipolar disorder.
Comment
Our study of 79 patients was too small to confirm the reported (5.8%) small excess of winter births among patients with bipolar disorder. Nevertheless, our study found that bipolar patients who have deep subcortical white matter lesions on MRIs (and, questionably, periventricular white matter lesions) are born most frequently during the winter months (January to March). Although the etiopathology of deep subcortical white matter lesions in younger patients is not established, in elderly patients these are thought to have a vascular cause (6), whereas periventricular white matter lesions may result from loss of ependymal lining to the ventricles. Age is an important risk factor for deep subcortical white matter lesions; hence, it is important that our group did not show a seasonal age bias. Although the mean age of bipolar subjects with deep subcortical white matter lesions (mean=40.6 years, SD=11.9) exceeded that of the subjects without deep subcortical white matter lesions (mean=34.4 years, SD=10.8), the difference was not significant (Student’s t=1.74, df=16, p=0.10). In contrast, there was a significant difference between the mean ages of the groups with and without periventricular white matter lesions (t=3.42, df=16, p=0.004). Differences in the relationship of birth season and mean age to the presence of periventricular and deep subcortical white matter lesions support the view that these abnormalities have different etiopathologies (6).
The link between deep subcortical white matter lesions and affective disorder is reported increasingly across the age spectrum. In children, cranial ultrasound studies have revealed a link between white matter abnormalities and affective disorders (8). Children with mania show MRI white matter lesions more frequently than adults with bipolar disorder (9). In old age, an association between white matter lesions and late-onset depression has been reported (10, 11). We surmise that deep subcortical white matter lesions in our adult patients may mark insults that contribute to the development of bipolar illnesses in adults with unfavorable outcomes (4). The excess in winter births of subjects with deep subcortical white matter lesions that we found suggests that they may be a consequence of an in utero or early-life environmental, or possibly infective, insult.
Our observations are necessarily preliminary because of the relatively small number of patients scanned. Much larger studies, or a meta-analysis of existing data, are needed to fully explore the effects of birth season and other variables, such as antenatal and perinatal events, on the neurobiology, course, and treatment response of subjects with bipolar disorder.
 |
Received Sept. 6, 2000; revision received March 16, 2001; accepted March 27, 2001. From the Department of Neuroradiology, Newcastle General Hospital, Newcastle Upon Tyne, U.K.; and Department of Psychiatry, Royal Victoria Infirmary, University of Newcastle Upon Tyne. Address reprint requests to Dr. Moore, Department of Psychiatry, Royal Victoria Infirmary, University of Newcastle Upon Tyne, Queen Victoria Rd., Newcastle Upon Tyne NE1 4LP, U.K.; [email protected] (e-mail). Funded by the Theodore and Vada Stanley Foundation.
1. Torrey EF, Rawlings RR, Ennis JM, Merrill DD, Flores DS: Birth seasonality in bipolar disorder, schizophrenia, schizoactive disorder and stillbirths. Schizophr Res 1996; 21:141-149Crossref, Medline, Google Scholar
2. Altshuler LL, Curran JG, Hauser P, Mintz J, Denicoff K, Post R: T2 hyperintensities in bipolar disorder: magnetic resonance imaging comparison and literature meta-analysis. Am J Psychiatry 1995; 152:1139-1144Google Scholar
3. Dupont RM, Jernigan TL, Butters N, Delis D, Hesselink JR, Heindel W, Gillin JC: Subcortical abnormalities detected in bipolar affective disorder using magnetic resonance imaging. Arch Gen Psychiatry 1990; 47:55-59Crossref, Medline, Google Scholar
4. Moore PB, Shepherd DJ, Eccleston D, MacMillan IC, Goswami U, McAllister VL, Ferrier IN: Cerebral white matter lesions in bipolar affective disorder: relationship to outcome. Br J Psychiatry 2001; 178:172-176Crossref, Medline, Google Scholar
5. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1999Google Scholar
6. Fazekas F, Kleinert R, Offenbacher H, Schmidt R, Kleinert G, Payer F, Radner H, Lechner H: Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology 1993; 43:1683-1689Google Scholar
7. Howell DC: Statistical Methods for Psychology, 4th ed. Toronto, Duxbury Press, 1997Google Scholar
8. Whitaker AH, Van Rossem R, Feldman JF, Schonfeld IS, Pinto-Martin JA, Torre C, Shaffer D, Paneth N: Psychiatric outcomes in low-birth-weight children at age 6 years: relation to neonatal cranial ultrasound abnormalities. Arch Gen Psychiatry 1997; 54:847-856Crossref, Medline, Google Scholar
9. Botteron KN, Vannier MW, Geller B, Todd RD, Lee BCP: Preliminary study of magnetic resonance imaging characteristics in 8- to 16-year-olds with mania. J Am Acad Child Adolesc Psychiatry 1995; 34:742-749Crossref, Medline, Google Scholar
10. O’Brien J, Desmond P, Ames D, Schweitzer I, Harrigan S, Tress B: A magnetic resonance imaging study of white matter lesions in depression and Alzheimer’s disease. Br J Psychiatry 1996; 168:477-485Crossref, Medline, Google Scholar
11. Dahabra S, Ashton CH, Bahrainian M, Britton PG, Ferrier IN, McAllister VA, Marsh VR, Moore PB: Structural and functional abnormalities in elderly patients clinically recovered from early- and late-onset depression. Biol Psychiatry 1998; 44:34-46Crossref, Medline, Google Scholar



