Prediction of Psychological Outcomes One Year After a Motor Vehicle Accident
Abstract
OBJECTIVE: The authors’ goal was to identify predictors of 1-year outcomes for consecutive patients in a hospital emergency department following motor vehicle accidents and to describe the prevalence and course of four types of psychiatric outcomes after such accidents. METHOD: Consecutive patients aged 17–69 years who attended a general hospital emergency department following a motor vehicle accident were identified. Medical information for these patients was extracted from case notes, and the patients completed self-report questionnaires at baseline (soon after the accident), 3 months after the accident, and 1 year after the accident. Measures included a self-report scale for posttraumatic stress disorder (PTSD), the Hospital Anxiety and Depression Scale, and questions about phobic travel anxiety. Logistic regression was used to examine predictors of outcome. RESULTS: Different frequencies and courses of PTSD, phobic travel anxiety, general anxiety, and depression were reported by a third of the subjects at both 3-month and 1-year follow-up. Many of the subjects reported improvements between 3 and 12 months, but others described late onset of psychiatric outcomes after the accident. There were differences in baseline and 3-month predictors of each type of 1-year outcome. CONCLUSIONS: The four types of psychiatric outcomes after a motor vehicle accident that were noted overlap, are persistent, and have different early predictors. These findings have implications for the early recognition of psychiatric consequences of motor vehicle accidents that would enable early intervention.
Stressful events have subjective meanings, such as loss, threat, and fear, which are important in the etiology of depression (1), anxiety, specific phobias, posttraumatic stress disorder (PTSD), and other psychiatric disorders. However, research on trauma (i.e., exceptionally frightening and threatening events, with or without physical injury) has largely focused on PTSD. Even so, it has repeatedly been observed in general population studies (2–4) and in studies of disasters (5, 6), combat (7), and other types of trauma (8) that depression, phobic avoidance, substance abuse, and other psychiatric problems are also frequent outcomes.
This article is concerned with the range of psychiatric outcomes after trauma, specifically the trauma experienced by subjects who attended a hospital emergency department as victims of motor vehicle accidents. Previous prospective studies of outcome have shown that a variety of psychiatric complications—PTSD, general anxiety, depression, and specific phobic anxiety about travel—are common (9–13) and that there is considerable overlap among them. However, they also occur separately, and our previous work (11) suggested that there are people who do not meet diagnostic criteria for PTSD who nevertheless report phobias and anxieties about travel that are just as distressing and disabling (11).
We have been able to examine the relationship among the different psychiatric outcomes after trauma in a prospective study over a 1-year period of a large group of consecutive patients aged 17–69 who attended a general hospital emergency department following a motor vehicle, bicycle, or pedestrian road accident. In this article we describe the frequency and course of four categories of psychiatric disorder (PTSD, general anxiety, phobic travel anxiety, and depression) and the extent to which 1-year outcomes are predicted by variables identified as being important in previous research or clinical practice (11, 14) and assessed either shortly after the accident or 3 months later.
Method
Consecutive patients aged 17–69 who attended the Accident and Emergency Department of the John Radcliffe Hospital, Oxford, following a motor vehicle accident (vehicle occupants, motorcyclists, bicyclists, pedestrians) (N=1,441) were approached to take part in the study and given or sent a questionnaire. Those who completed the questionnaires in the hospital were more likely to have been admitted. A further 81 subjects were not asked to take part for different reasons. Individuals with head injury who had been unconscious for more than 15 minutes (N=23) or were too ill to complete a questionnaire (N=11) were excluded; seven people died in the emergency department. Overseas visitors (N=32) and those with learning or psychiatric problems (N=8) were also excluded. There were 12 initial refusals.
Data were collected by means of self-completion questionnaires as specified by the local ethics committee. The baseline questionnaire covered background details, previous travel, health and daily activities, previous tendency to worry, and emotional problems. Follow-up questionnaires, which were sent at 3 months and 1 year after the accident, covered physical recovery; financial, work and legal problems; return to traveling; cognitions; and cognitive strategies. Participants also completed the Posttraumatic Stress Symptoms Scale (15), the Hospital Anxiety and Depression Scale (16), and a six-question health and daily activities questionnaire derived from the 36-Item Short-Form Health Survey (17).
Measures
Outcome variables
The outcome variable of phobic travel anxiety, a measure based on previous research (18), combines increased nervousness about traveling and avoidance of traveling. The cutoff points are consistent with the DSM-IV criteria for phobia. For the outcome variable of general anxiety we used the recommended cutoff of 10 or more on the Hospital Anxiety and Depression Scale (16). For depression we used the recommended cutoff of 10 or more on the Hospital Anxiety and Depression Scale. For PTSD we used the minimum number of symptoms on the Postraumatic Stress Symptom Scale (15) required by DSM-IV criteria.
Predictor variables
Thirteen baseline variables were included in the present study because previous research or theoretical considerations suggested they may be predictors of PTSD (see our earlier report [14]), general anxiety, depression, or phobic travel anxiety. A further seven measures assessed at 3 months were also examined, three social stressors and four cognitive “maintaining factors” (19).
The 13 baseline variables were gender, hospital admission, severity of injury, accident group, previous confidence as a passenger, previous motor vehicle injury, previous frequency of road use, previous emotional problems, tendency to worry, and four reactions to the accident (dissociation, blaming oneself, fear, and negative emotions).
The severity of the injury was classified as no injury, soft tissue injury only, or fracture. The accident group included vehicle driver, passenger, motorcyclist, bicyclist, and pedestrian. The subject’s previous confidence as a passenger was rated on a 5-point scale ranging from very relaxed to very nervous. For previous frequency of road use, seven modes of travel (car driver, passenger, bus, motorcycle, moped, bicycle, on foot) were rated on a 5-point scale on which 1=daily and 5=never. Previous emotional problems were rated on a 6-point scale on which 1=not at all and 5=extremely in response to the question, “During the 4 weeks before the accident how much were you bothered by emotional problems (such as feeling anxious, depressed or irritable)?” This question was from the 36-Item Short-Form Health Survey (17). The tendency to worry was rated on a 7-point scale on which –3=very much disagree and 3=very much agree with the statement, “I tend to worry a lot about things.”
Negative emotions and dissociation after the accident were rated on a 5-pont scale on which 0=not at all and 4=extremely in response to a question about how subjects were feeling “at the moment” in regard to 10 emotional responses (angry, numbed, shaky, excited, relieved, weepy, anxious, guilty, dazed, calm). Negative emotions were the mean of the ratings for anxious, shaky, and weepy minus the rating for calm. Dissociation was the mean of the ratings for dazed and numb. Feeling to blame after the accident was rated on a 3-point scale on which 1=yes, 2=partly, and 3=no in response to the question, “Do you blame yourself at all for the accident?” The reaction of fear was rated on a 4-point scale on which 1=not frightening and 4=very frightening in reply to the question, “How frightening was the accident?”
Social stressors assessed at 3 months included health problems, financial problems, and litigation. Subjects rated their recovery from accident injuries on a 3-point scale on which 0=back to normal, 1=fully recovered, and 2=major problems. They rated their financial problems on a 3-point scale on which 0=no and 2=major in reply to the question, “Has the accident resulted in financial problems for you now?” Litigation was assessed by asking whether the respondent was making a claim for compensation.
Cognitive variables
The frequency of cognitions about memories of the accident was rated on a 5-point scale on which 0=never and 4=always. Rumination was the mean score in response to two questions, “Why did it happen to me?” and “I dwell on memories of the accident.” Thought suppression was the mean score in response to “I try to push them out of my mind” and “I try to distract myself.” Negative interpretations of intrusive recollections was the mean of “I must be going out of my mind” and “I will never get over it.” Anger was the score on “Others have harmed me.” Categorical scales were treated as if they had equal intervals, but most were dichotomized for the analysis.
Statistical Analysis
Logistic regression was used to examine predictors of outcome. The dichotomous dependent variables were the logits of the probability of a poor outcome at 1 year. Logistic regression models were fitted, each independent variable being fitted separately and then adjusted for the remaining factors. Most of the continuous predictor variables were not normally distributed and were dichotomized. This inevitably resulted in some loss of information and reduced the total amount of deviance explained in the models, but the categories were felt to be more useful in a clinical context than log-transformed continuous variables. Cutoff points were chosen to provide meaningful groups of a reasonable size. Significance levels were set at p<0.003 because of the 20 variables included (Bonferroni correction).
Results
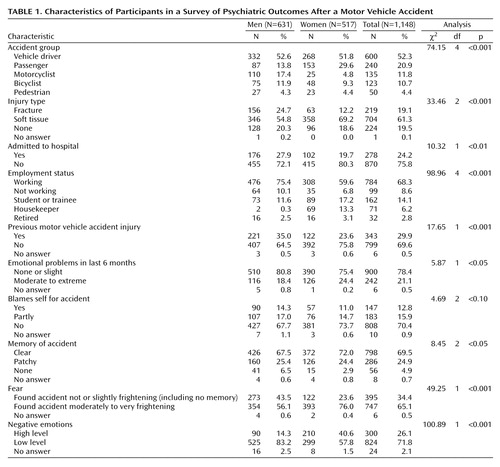
Of the 1,441 eligible patients 1,148 (80%) completed a questionnaire at baseline. At 3 months, 865 (75%) of the 1,148 participants completed a follow-up questionnaire, and at 1 year 773 (67%) did so. Table 1 shows some of the characteristics of the participants. Just over half were men, and half were younger than 30 years old. The mean age of the total group was 32.47 years (SD=13.10). Men and women did not differ significantly in age: the mean age of the men was 32.64 (SD=12.96), and the mean age of the women was 32.93 (SD=13.28). The majority suffered soft tissue injuries (abrasions or lacerations) only. Seven in 10 said they could remember the accident clearly, and two-thirds rated the accident as moderately to very frightening.
Comparison of Participants With Nonparticipants and Dropouts
To examine selection bias, we compared the 293 eligible people who did not take part in the study with the 1,148 participants on demographic and medical factors available from the hospital notes. Initial participation was not related to accident group (being a vehicle driver, passenger, motorcyclist, bicyclist, or pedestrian). Women were significantly more likely to participate (82% [N=517] of the 628 women compared with 78% [N=631] of the 813 men) (χ2=4.85, df=1, p<0.05), as were those over age 30 (84% [N=552] of those older than 30 compared with 76% [N=596] of those 30 years old or younger) (χ2=11.13, df=1, p<0.01). More of those who were admitted to the hospital participated in the study (89% [N=278] of those who were hospitalized compared with 77% [N=870] of those who were not hospitalized) (χ2=19.49, df=1, p<0.001).
The 375 participants who dropped out of the study during the follow-up year were compared with the 773 who remained in the study. Women were more likely to remain in the study for the whole year than men, as were those over age 30. Employment status at first assessment was also related to continuing participation: only 52% (N=51) of the 99 subjects who were out of work or off sick completed the 1-year questionnaire, compared with 94% (N=30) of the 32 retired subjects and 70% (N=594) of the 855 subjects who were employed or were minding the home (χ2=26.65, df=4, p<0.001). Patients who were admitted to the hospital after the accident were also more likely to remain in the study than those who were not admitted (80% [N=222] of 278 compared with 63% [N=551] of 870) (χ2=26.15, df=1, p<0.001). However, none of the other predictor variables measured at first assessment or at 3 months were related to subsequent participation.
Characteristics
Table 1 summarizes the characteristics of the participants. There were a number of gender differences. More men than women suffered fractures and were admitted to the hospital, and men were more likely to have been injured in a previous road accident. More men also said they were to blame for the accident, but this was because more women were passengers. Women were significantly more likely to report emotional difficulties in the month before the accident and more fear and emotional distress after the accident.
Frequency, Onset, and Course of Psychiatric Disorders
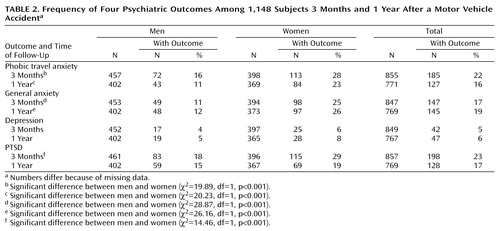
A third of the subjects reported psychiatric outcomes after the accident. In view of the overrepresentation of women among the participants, Table 2 shows the frequency of each of our four main categories of psychiatric disorders for men and women. More women than men had phobic travel anxiety and general anxiety at 3 months and 1 year and PTSD at 3 months. More passengers, both male and female, had phobic travel anxiety at 1 year than drivers (data not shown). Age and employment status were not associated with psychological outcome for men or women.
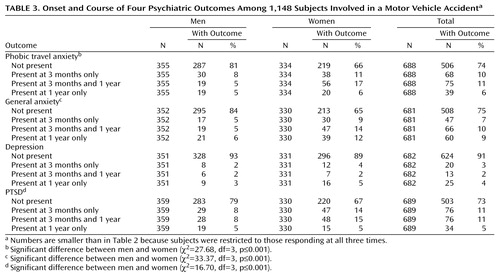
Table 3 shows the onset and course of each type of disorder for subjects for whom information was available at all three assessments; there were marked similarities in course for the four outcomes. In the majority of cases, onset of the disorder was within 3 months of the accident. The disorder was persistent at 1 year in about half of the subjects with phobic travel anxiety (52% [N=75]), general anxiety (58% [N=66]), and PTSD (50% [N=76]) but in only 39% (N=13) of those with depression (data not shown). Late onset between 3 months and 1 year was reported by around 5% of subjects for each type of psychiatric outcome. A small number of people (N=35) had another accident between the 3-month and 1-year assessment, and this was associated with late-onset general anxiety (13% [N=8] of 60 subjects with late-onset general anxiety compared with only 4% [N=27] of 611 subjects with early-onset or no anxiety) (χ2=7.07, df=1, p<0.01) but not with phobic travel anxiety, PTSD, or depression (data not shown).
Litigation
At 1 year, 31 (58%) of the 536 people who felt they were not to blame for the accident were claiming compensation. Among these subjects, gender and age were not related to being a claimant, but those who were working were less likely to claim than those who were out of work, retired, or at home.
Comorbidity
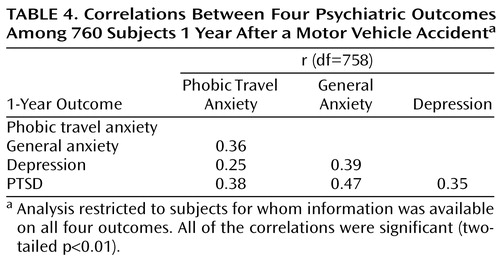
There was considerable overlap among the psychological outcomes after phobic travel anxiety, PTSD, general anxiety, and depression at both 3 months and 1 year, but sizable proportions of individuals with psychological outcomes had only one or two types of psychiatric disorder. This is shown in a correlation matrix (Table 4) and in a Venn diagram (Figure 1). For simplicity of presentation, Figure 1 does not include depression; there were only 10 people with depression who did not have general anxiety as well.
Predictors of Outcomes at 1 Year
The results of the logistic regression analyses for the three anxiety disorders are shown in Table 5. A number of variables were significant (p<0.003) for the prediction of depression when entered on their own (baseline negative emotions, and 3-month health and financial problems, anger, and rumination). The results of logistic regression for depression are not shown because there were no significant predictors of depression after adjustment.
As might be expected given the overlap among the outcomes, a number of predictor variables entered separately into the regression were common to phobic travel anxiety, general anxiety, and PTSD. Among the baseline variables, these were previous emotional problems in the month before the accident, previous low levels of confidence as a passenger, finding the accident frightening, and dissociative symptoms and a high level of negative emotions after the accident. The tendency to worry predicted general anxiety, and variables measuring aspects of travel mainly predicted phobic travel anxiety. Medical variables other than hospital admission were not significant predictors of any outcomes before or after adjustment.
All of the cognitive measures taken at 3 months were predictors of phobic travel anxiety, general anxiety, and PTSD when entered singly. Financial and health problems and litigation at 3 months also predicted these three outcomes and were the only significant single predictors of depression (data not shown). Thought suppression was a more powerful predictor for men than women (data not shown).
After adjustment for the remaining predictor variables, the unique predictors of each outcome were rather different. Phobic travel anxiety was predicted by baseline travel measures, previous emotional problems, and finding the accident frightening, but not by any of the 3-month maintaining factors. For PTSD, rumination and negative interpretations of intrusive recollections at 3 months were the only remaining significant predictors. Rumination and negative interpretations also remained significant for general anxiety, together with two baseline measures, gender and previous emotional problems.
Discussion
This paper confirms and extends evidence of the characteristics of four categories of psychiatric outcomes often seen after a motor vehicle accident (11, 13). Although there is considerable overlap, the four disorders may occur separately and are different in onset and course. There were marked differences between men and women in the frequency and course of all psychiatric outcomes after motor vehicle accidents.
Most previous research on outcomes after motor vehicle accidents has concentrated on the comorbidity of PTSD and depression. The present results show that general anxiety is also common, as is another posttraumatic syndrome, phobic travel anxiety. Phobic travel anxiety can be both distressing and markedly disabling, leading to avoidance of travel or of situations or circumstances that are reminders of the accident, such as passing the place of the accident, similar road conditions, or traveling in a vehicle of the same make or color.
Although the large size and nature of our study group are important advantages, there are some limitations to our study. Findings refer only to patients who attended an emergency department. The information was collected by self-report. One-fifth of the potential sample did not take part in the initial assessment, and they differed from participants in some important respects. Women, subjects older than 30, and admitted patients were overrepresented among participants, affecting the generalizability of the results. Diagnostic categories were used rather than clinical diagnoses defined by recognized criteria for outcomes other than PTSD. However, the findings are consistent with those of a previous interview study that had a high response rate (11).
Predictors of 1-Year Outcome
We considered predictor variables identified in previous research on PTSD, anxiety, and depression, together with variables related to travel. Several predictor variables were common to all four types of psychiatric disorder, but there were also differences. Most notably, variables related to travel predicted phobic travel anxiety but not the other outcomes. For example, male and female passengers did worse than drivers. It is not clear why this should be, but it is possible that lack of control over events on the road makes passengers feel more threatened. Motorcyclists were eight times more likely than men suffering other types of accidents to describe phobic travel anxiety. In the earlier study (11), 42% of motorcyclists had given up their motorcycles 1 year after an accident.
For those who developed PTSD and general anxiety, cognitive and social factors measured at 3 months were generally better predictors than initial emotional response and characteristics of the accident. In particular, persistent health problems, rumination about the accident, and negative interpretations of intrusive recollections were strong predictors of 1-year outcome, increasing the probability of a patient suffering anxiety or PTSD four to seven times. Explanations of the reasons why some people develop phobic travel anxiety rather than general anxiety or PTSD are speculative. It may be that some victims overgeneralize the specific danger of driving, whereas others feel more threatened in general.
Our findings can be seen as reflecting the complex psychological meaning of a motor vehicle accident, whether or not there is injury. It may be perceived to be life-threatening and frightening. There can be continuing physical problems and disability interfering with everyday life and ambitions. Financial loss and anxiety are frequent. There may be guilt. It is to be expected that the varied meanings of different types of accident and injury to individuals will result in a wide range of psychological outcomes.
Clinical and Policy Implications
The finding that at least a third of consecutive patients who came to an emergency department following a motor vehicle accident suffered persistent psychiatric disorders has important implications both for the psychological care of people who have suffered medically minor physical injuries and for wider social policies. It is likely that those at high risk of chronic difficulties could be recognized clinically soon after the accident and be offered early treatment. It is reasonable to expect that a clinical assessment instrument based on the rather simple self-report variables described in this and our other research (13) could substantially improve the accuracy of recognition of those at risk who might benefit from early psychological treatment. There is a need for research to demonstrate that early identification is both possible and effective.
The findings also emphasize the predictive importance of medical and other maintaining factors, such as continuing health problems, cognitions, litigation, and financial difficulty, during the months after the accident. This suggests opportunities for psychological interventions and for changes in the organization of care to improve outcome. A current Oxford randomized controlled trial is evaluating the effectiveness of cognitive behavior therapy in treating PTSD identified in the year following an motor vehicle accident. Apart from improvements in medical and psychological care, there are wider policy implications. Litigation is a continuing reminder of the accident that may interfere with a natural tendency toward symptom resolution. Changes in compensation procedures, as have been discussed in relation to whiplash neck injury (20), might also have considerable benefits.
We conclude that awareness of all the psychiatric outcomes after motor vehicle accidents and the development of clinically useful procedures for early recognition and prediction of chronic problems should contribute to planning changes in medical and legal procedures and the introduction of psychological interventions that will contribute to the management of a very large public health problem.
 |
 |
 |
 |
 |
Received Nov. 12, 1999; revisions received July 12 and Dec. 1, 2000; accepted Jan. 16, 2001. From the University of Oxford, Department of Psychiatry, Warneford Hospital. Address reprint requests to Professor Mayou at the University of Oxford, Department of Psychiatry, Warneford Hospital, Oxford OX3 7JX, U.K.; [email protected] (e-mail).
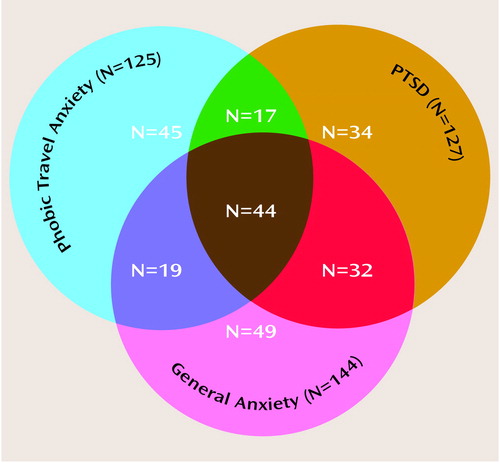
Figure 1. Prevalence of Three Anxiety Outcomes Among 1,148 Subjects 1 Year After a Motor Vehicle Accidenta
aFour subjects for whom there was incomplete information on all three outcomes were excluded.
1. Kendler KS, Karkowski LM, Prescott CA: Stressful life events and major depression: risk period, long-term contextual threat, and diagnostic specificity. J Nerv Ment Dis 1998; 186:661-669Crossref, Medline, Google Scholar
2. Breslau N, Davis GC, Peterson E: Traumatic events and post-traumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216-222Crossref, Medline, Google Scholar
3. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984-991Crossref, Medline, Google Scholar
4. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048-1060Google Scholar
5. McFarlane AC, Papay P: Multiple diagnoses in post-traumatic stress disorder in the victims of a natural disaster. J Nerv Ment Dis 1992; 180:498-504Crossref, Medline, Google Scholar
6. Green BL, Lindy JD, Grace MC, Leonard AC: Chronic posttraumatic stress disorder and diagnostic comorbidity in a disaster sample. J Nerv Ment Dis 1992; 180:760-766Crossref, Medline, Google Scholar
7. Bleich A, Koslowsky M, Dolev A, Lerer B: Post-traumatic stress disorder and depression. Br J Psychiatry 1997; 170:479-482Crossref, Medline, Google Scholar
8. Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK: Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry 1998; 155:630-637Link, Google Scholar
9. Blanchard EB, Hickling EJ, Taylor AE, Loos W: Psychiatric morbidity associated with motor vehicle accidents. J Nerv Ment Dis 1995; 183:495-504Crossref, Medline, Google Scholar
10. Blanchard EB, Buckley TC, Hickling EJ, Taylor AE: Posttraumatic stress disorder and comorbid major depression: is the correlation an illusion? J Anxiety Disord 1998; 12:21-37Crossref, Medline, Google Scholar
11. Mayou R, Bryant B, Duthie R: Psychiatric consequences of road traffic accidents. Br Med J 1993; 307:647-651Crossref, Medline, Google Scholar
12. Koren D, Arnon I, Klein E: Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry 1999; 156:367-373Abstract, Google Scholar
13. Hickling EJ, Blanchard EB: The International Handbook of Road Traffic Accidents and Psychological Trauma: Current Understanding, Treatment and Law. Oxford, UK, Pergamon Press, 1999Google Scholar
14. Ehlers A, Mayou RA, Bryant B: Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. J Abnorm Psychol 1998; 107:508-519Crossref, Medline, Google Scholar
15. Foa EB, Riggs DS, Dancu CV, Rothbaum BO: Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress 1993; 6:459-473Crossref, Google Scholar
16. Zigmond AS, Snaith RP: The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67:361-370Crossref, Medline, Google Scholar
17. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473-483Crossref, Medline, Google Scholar
18. Mayou RA, Bryant BM: Effects of road accidents on travel. Injury 1994; 25:457-460Crossref, Medline, Google Scholar
19. Ehlers A, Steil R: Maintenance of intrusive memories in posttraumatic stress disorder: a cognitive approach. Behavioural and Cognitive Psychotherapy 1995; 23:217-249Crossref, Medline, Google Scholar
20. Cassidy JD, Carroll LJ, Cote P, Lemstra M, Berglund A, Nygren A: Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med 2000; 342:1179-1186Google Scholar



