Postpartum Depression in Women Receiving Public Assistance: Pilot Study of an Interpersonal-Therapy-Oriented Group Intervention
Abstract
OBJECTIVE: This study investigated whether a preventive intervention based on the principles of interpersonal psychotherapy administered to pregnant women would reduce the risk of postpartum major depression. METHOD: Thirty-seven pregnant women receiving public assistance who had at least one risk factor for postpartum depression were randomly assigned to a four-session group intervention or to a treatment-as-usual condition. Thirty-five of the women completed the study. Structured diagnostic interviews were administered to assess for postpartum major depression. RESULTS: Within 3 months after they gave birth, six (33%) of the 18 women in the treatment-as-usual condition had developed postpartum major depression, compared with none of the 17 women in the intervention condition. CONCLUSIONS: A four-session interpersonal-therapy-oriented group intervention was successful in preventing the occurrence of major depression during a postpartum period of 3 months in a group of financially disadvantaged women.
About 10%–16% of parous women experience postpartum depression that is associated with more severe depressive symptoms, social dysfunction, and marital maladjustment than is depression unrelated to the postpartum period (1). Reducing the risk of postpartum depression in poor women is especially important because poverty is associated with twice the rate of postpartum depression (2) and because socioeconomic adversity amplifies the negative effects of postpartum depression on infant development (3). Poverty also limits access to resources such as mental health services that can reduce the deleterious effects of postpartum depression (2).
Postpartum depression is particularly amenable to prevention. There is a clear marker before its onset (childbirth) and a defined period of risk (the 3-month period after childbirth) (4). In addition, research has increased the feasibility of identifying high-risk mothers, and many risk factors for postpartum depression are amenable to change (5).
In general, preventive interventions, particularly those administered in a group format, appear to reduce postpartum depressive symptoms. To our knowledge, only two published studies (6, 7), to date, have examined the prophylactic efficacy of interventions in reducing postpartum depression. One of these studies (6) found that, in a group of high-risk women, 8% of the women who received a group intervention focusing on preparation for parenthood and social support developed depression in the 3 months after giving birth, compared with 16% of a control group. In contrast, the other study (7) showed a negligible percent difference in the occurrence of postpartum depression among high-risk women who were assigned to either a control group or a group intervention that provided general support. Limitations of this previous research are lack of randomization (6), poor compliance rates (6, 7), and use of an inadequate measure of postpartum depression (7).
The present study assessed the efficacy of a group intervention in reducing the occurrence of postpartum depression in pregnant women who were receiving public assistance and who had at least one risk factor for postpartum depression. The intervention was based on interpersonal therapy, an effective form of treatment for depression (8), targeting factors (e.g., poor social support, role transition, life stressors) that may play a crucial role in the onset of postpartum depression (5, 9). Interpersonal therapy is the only existing psychotherapy with efficacy data for the treatment of prenatal and postpartum depression (10, 11).
Method
Subjects for this study were pregnant women receiving public assistance who were at 20–32 weeks gestation and who were attending a prenatal clinic at a general hospital in the Northeast. After providing written informed consent, these women completed a survey that assessed for risk factors for postpartum depression (i.e., a previous episode of depression or postpartum depression, mild to moderate levels of depressive symptoms, poor social support, or a life stressor within the last 6 months). Participation for this phase of the study was very high (122 [90%] of 135 subjects).
Women who reported at least one predictor of postpartum depression were asked to participate in the next phase of the study (i.e., random assignment to either the intervention group or a treatment-as-usual condition). All subjects understood that whether or not they were assigned to the intervention condition, they would continue to receive the standard medical attention and treatment that is provided to all patients attending the prenatal clinic, irrespective of participation or refusal of participation in the research protocol.
Fifty percent of the women who were eligible (41 of 82 subjects) consented to participate in this phase of the study. Patients who met criteria for current major depression as determined by the depression module of the nonpatient version of the Structured Clinical Interview for DSM-IV (SCID) (12), were excluded from the study (N=4). The final study group included 37 women. After completion of the preintervention assessments, subjects were randomly assigned to one of the conditions. At any one time, each condition consisted of four to six women.
Before and after the intervention or treatment as usual, all subjects completed a Beck Depression Inventory (13) to assess the degree of depressive symptoms. At 3 months postpartum, all subjects were assessed for postpartum depression for the previous 3 months with the depression module of the SCID (12).
Briefly, the intervention, Survival Skills for New Moms, involved four 60-minute group sessions over a 4-week period. The first session consisted of a rationale for the program and psychoeducation on “baby blues” and postpartum depression. The second session focused on identifying role transitions, changes associated with role transitions, and goals for successfully managing role transitions, with an emphasis on transition to motherhood. The third session was concerned with setting goals, developing supports, and identifying potential interpersonal conflicts, especially once the baby was born. The fourth session taught skills for resolving interpersonal conflicts and reviewed the main themes of the intervention. Handouts based on the material presented in each session were given as well as session-related homework assignments.
The majority of the women (N=15, 88%) attended at least three of the four sessions. Only one woman from the intervention group and one woman from the treatment-as-usual condition dropped out of the study.
Results
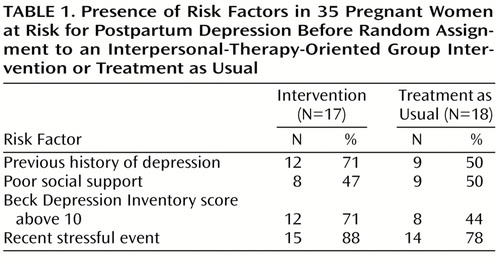
Of the 35 women who completed the study, 16 (46%) were Caucasian, 27 (77%) were single, and 27 (77%) had completed high school. The mean age of the subjects was 23.4 (SD=4.41, range=18–38). The mean preintervention Beck Depression Inventory score was 11.06 (SD=6.84), and the mean number of risk factors for postpartum depression was 2.60 (SD=1.90). Table 1 shows the number of women in each condition who reported presence of the different risk factors. There were no significant differences between these two groups on any demographic variables, number of risk factors, number of children, or parity. In addition, there were no significant differences between the two groups on any of the risk factors, namely, presence of a previous episode of depression, experience of a recent life stressor, poor social support, or level of depressive symptoms.
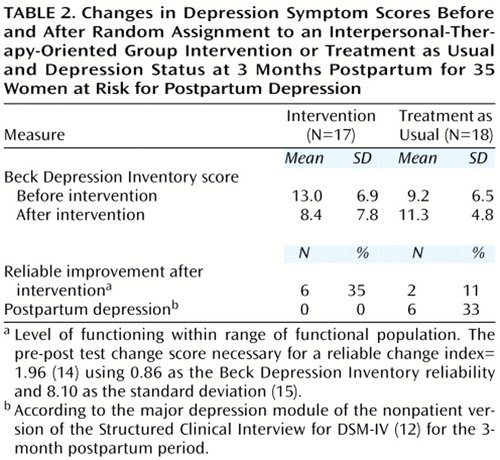
The change in Beck Depression Inventory scores before and after the intervention for the 17 women in the intervention group was significantly greater than that for the 18 women who received treatment as usual (t=3.50, df=33, p=0.001). Table 2 shows the mean pre- and postintervention scores, the percent of women with reliable improvement (i.e., those whose level of functioning moved within the range of the functional population after the intervention), and the number of women who met criteria for major depression within the 3-month postpartum period.
To calculate a reliable change index and cutoff score for the Beck Depression Inventory, we obtained a reliability estimate and descriptive statistics for the functional distribution of the Beck Depression Inventory from published studies (15, 16). As recommended by Jacobson and Truax (14), the reliable change index was greater than 1.96. A chi-square showed that women in the intervention group were significantly less likely to develop postpartum depression than were those in the treatment-as-usual group (p=0.02, Fisher’s exact test) (Table 2). Three of the women who developed postpartum depression had a previous history of depression. The study found that a history of depression, initial level of depressive symptoms, and primiparous status were not significantly related to the presence of postpartum depression.
Discussion
This preliminary study found that, in a group of financially disadvantaged women at risk for postpartum depression, a four-session antepartum group intervention prevented the occurrence of major depression within the 3-month postpartum period. However, 33% of the women who received treatment as usual reported postpartum major depression. It is possible that a longer follow-up period may have resulted in a similar rate of postpartum depression between the two conditions. However, research has demonstrated that the highest risk period for developing depression is during the first 3-month postpartum period and that 76% of women who develop postpartum depression over a 6-month period report that their depression began less than 5 weeks after delivery (17).
Our finding of significant efficacy of the group intervention differs from the results of previous studies (6, 7), possibly because of the higher compliance rate in the current study. Clearly, there would be important public health implications if the results of this trial were replicated in a larger trial, showing that this low-cost preventive intervention prevents the emotional and financial tolls associated with postpartum depression.
 |
 |
Received April 5, 2000; revision received Aug. 2, 2000; accepted Oct. 16, 2000. From the Department of Psychiatry and Human Behavior, Brown University and Woman and Infant Hospital, Providence, R.I.; and the Psychology Department, University of Miami. Address reprint requests to Dr. Zlotnick, Butler Hospital, 345 Blackstone Blvd., Providence, RI 02906; [email protected] (e-mail). Supported by a grant from the Klingenstein Third Generation Foundation and a grant from Brown University, Department of Psychiatry and Human Behavior.
1. O’Hara MW, Zekoski EM, Phillips LH, Wright EJ: Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 1990; 99:3–15Crossref, Medline, Google Scholar
2. Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP: Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol 1995; 63:445–453Crossref, Medline, Google Scholar
3. Murray L, Fiori-Cowley A, Hooper R, Cooper P: The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev 1996; 67:2512–2526Google Scholar
4. Wisner KL, Wheeler SB: Prevention of recurrent postpartum major depression. Hosp Community Psychiatry 1994; 45:1191–1195Google Scholar
5. Beck CT: A meta-analysis of predictors of postpartum depression. Nurs Res 1996; 45:297–303Crossref, Medline, Google Scholar
6. Elliott SA: Psychological strategies in the prevention and treatment of postnatal depression. Baillieres Clin Obstet Gynaecol 1989; 3:879–903Crossref, Medline, Google Scholar
7. Stamp GE, Williams AS, Crowther CA: Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized controlled trial. Birth 1995; 22:138–143Crossref, Medline, Google Scholar
8. Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, Glass DR, Pilkonis PA, Leber WR, Docherty JP, Fiester SJ, Parloff MB: National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 1989; 46:971–982Crossref, Medline, Google Scholar
9. O Hara MW: Childbearing, in Psychological Aspects of Women’s Reproductive Health. Edited by O’Hara MW, Reiter R, Johnson S, Milburn A, J Engeldinger. New York, Springer, 1995, pp 26–48Google Scholar
10. Stuart S, O’Hara MW: Treatment of postpartum depression with interpersonal psychotherapy. Arch Gen Psychiatry 1995; 52:75–76Crossref, Medline, Google Scholar
11. Spinelli MG: Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry 1997; 154:1028–1030Google Scholar
12. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1997Google Scholar
13. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
14. Jacobson NS, Truax P: Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 6:12–19Crossref, Google Scholar
15. Nietzel MT, Russel RL, Hemmings KA, Gretter ML: The clinical significance of psychotherapy for unipolar depression: a meta-analytic approach to social comparison. J Consult Clin Psychol 1987; 55:156–161Crossref, Medline, Google Scholar
16. Beck AT, Steer RA, Garbin MG: Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988; 8:77–100Crossref, Google Scholar
17. Cox JL, Murray D, Chapman G: A controlled study of the onset, duration and prevalence of postnatal depression. Br J Psychiatry 1993; 163:27–31Crossref, Medline, Google Scholar



