Comparisons of Men With Full or Partial Eating Disorders, Men Without Eating Disorders, and Women With Eating Disorders in the Community
Abstract
OBJECTIVE: The authors compared 62 men who met all or most of the DSM-III-R criteria for eating disorders with 212 women who had similar eating disorders and 3,769 men who had no eating disorders on a wide variety of clinical and historical variables. METHOD: The groups of subjects were derived from a community epidemiologic survey performed in the province of Ontario that used the World Health Organization’s Composite International Diagnostic Interview. RESULTS: Men with eating disorders were very similar to women with eating disorders on most variables. Men with eating disorders showed higher rates of psychiatric comorbidity and more psychosocial morbidity than men without eating disorders. CONCLUSIONS: These results confirm the clinical similarities between men with eating disorders and women with eating disorders. They also reveal that both groups suffer similar psychosocial morbidity. Men with eating disorders show a wide range of differences from men without eating disorders; the extent to which these differences are effects of the illness or possible risk factors for the occurrence of these illnesses in men is not clear.
Men and boys with eating disorders have been the subject of occasional reports since Morton’s 1694 report (1), which included both a male and a female patient. In the first half of the 20th century, males with eating disorders were considered rare because eating disorders were assumed to be female-gender-bound (2).
This latter issue spawned two critical areas of debate. One argument has been that because eating disorders are so rare in males, the nature of the illness must somehow be atypical in males (3, 4). The second line of discussion has suggested that there must be something different about males who develop an eating disorder. For example, it has been suggested that a higher proportion of males with eating disorders might be homosexual (5, 6).
Examination of these two hypotheses has produced conflicting results. Most larger clinical series comparing men and women with eating disorders (7–10) have found minimal differences in their clinical presentation, psychometric measurements, or response to treatment (11).
Most previous reports have relied on hospital clinics for subjects for investigation and have not included appropriate control groups. This strategy may bias results by increasing symptom severity, washing out male-female symptom differences, or selecting a specialized population. To date, to our knowledge there has been no report of the characteristics of men with eating disorders selected from the general population. Olivardia et al. (12) reported on a group of 25 men recruited by advertisement from a local college; these men were compared with a group of men with an orthopedic condition and a group of women with bulimia nervosa. This study showed that men with eating disorders were different from the men with an orthopedic condition on most variables studied but were similar to the women with bulimia nervosa. Striegel-Moore et al. (13) studied a group of 98 men with eating disorders drawn from the records of U.S. Veteran’s Affairs medical centers and compared them with a matched set of men without eating disorders. This comparison showed higher rates of depression and substance use in the men with eating disorders than in the men without eating disorders.
We report here on a group of men with full and partial eating disorders derived from a large community epidemiologic sample. We compared these men with men who did not have eating disorders and with women who had eating disorders from the same community sample. This strategy allowed us to examine the two questions of interest—is the illness different in men or are men with the illness different—without the confounding factors associated with clinical samples.
Method
The subjects for this study were drawn from a community epidemiologic survey, the Mental Health Supplement to the Ontario Health Survey, referred to here as the Supplement. The nature of this sample and the selection are fully described elsewhere (14–16). Briefly, households across the province of Ontario were randomly sampled by using a multistage cluster design. Within each household one individual (aged 15 years or older) was randomly chosen for interview. Informed consent was obtained according to procedures conforming to Canadian federal legislative requirements. A 76% response rate resulted in a sample size of 9,953. The sample was weighted to adjust for nonresponse and to reconcile its age-gender profile with that of the 1991 Ontario census.
Subjects were interviewed face-to-face by trained interviewers for 1–2 hours; the interviewers used the University of Michigan’s version of the World Health Organization (WHO) Composite International Diagnostic Interview (17), which generates both DSM-III-R and ICD-10 diagnoses. Reliability and validity of the parent Composite International Diagnostic Interview instrument were found to be good in WHO field trials (17, 18), and the modifications focused on improved flow and comprehensibility of the items (19). Subjects were assessed for lifetime and current anxiety disorders, affective disorders, eating disorders, the use and abuse of alcohol and other substances, and antisocial personality disorder. Respondents older than 64 years of age were given a shortened version of the Composite International Diagnostic Interview to minimize interview burden. Since the version for older respondents excluded eating disorders, results are limited to the 15–64-year-old respondents. Binge-eating disorder was not assessed in the original survey because the syndrome had not yet been fully defined.
The presence of a lifetime full or partial eating disorder was defined in the same way for both men and women. Full eating disorder syndromes were defined by using the DSM-III-R classification system. Required criteria for anorexia nervosa included abnormally low body weight (defined as 15% below the Canadian standard weight for age and height), overconcern with weight and shape, a self-perception of being overweight when others felt the respondent to be too thin, and, for women, three consecutively missed menstrual periods. Partial syndrome anorexia nervosa required meeting the first criterion (low body weight) but did allow one negative response to the remaining criteria (weight loss, body image concerns, concerns about weight loss, or, for women, amenorrhea).
Both full and partial syndrome bulimia nervosa required recurrent episodes of binge eating. In addition, full syndrome respondents met the diagnostic criteria of frequency (3 or more months of binge eating at least twice a week), having weight and shape concerns, feeling a lack of control over their eating behavior, and having one or more compensatory behaviors. Partial syndrome respondents were those meeting all but one of these criteria.
Men without eating disorders were defined as those respondents who showed no evidence of either full or partial syndrome eating disorders in their lifetime. They could, however, qualify for one of the other Composite International Diagnostic Interview/DSM-III-R diagnoses assessed in the Supplement.
Statistical Procedures
Results are presented as raw numbers, prevalence estimates, and weighted percentages. For the comparisons of subjects with and without eating disorders, the subgroups were treated as clinical samples (i.e., unweighted) because of the small numbers of men with eating disorders. Odds ratios and chi-square analyses were used for categorical variables, and analysis of variance was used for continuous measures. Significance was set at 0.01 because of the multiple comparisons.
Results
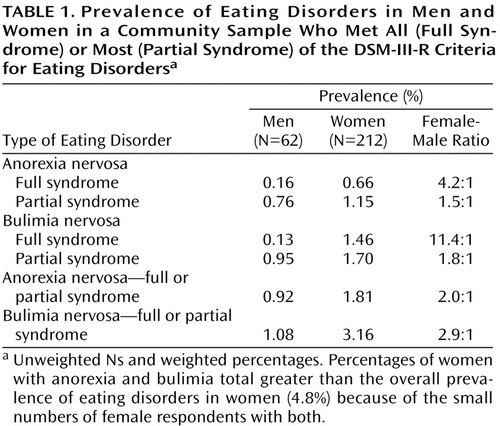
The prevalence rate (weighted) of full or partial eating disorders for men was 2.0%, compared with 4.8% for women. The female-male ratio of full or partial syndrome anorexia nervosa was 2.0:1; for full or partial syndrome bulimia nervosa, it was 2.9:1.
Table 1 presents the diagnostic breakdown for the men and women suffering from an eating disorder. The rate for full syndrome eating disorders (anorexia nervosa and bulimia nervosa combined) in men was 0.3%, compared with 2.1% for women. There was a significant difference in the overall rates of full and partial syndrome in men and women (χ2=15.34, df=3, p<0.002). When these were broken down by type of eating disorder (Table 1), the most marked differences were lower rates of full syndrome bulimia in men than in women, with the reverse holding for partial syndrome bulimia.
Analysis of variance showed a significant lowering of age at onset of eating disorder in the group of subjects born after 1959 (F=7.72, df=2, 61, p<0.001) with no significant gender difference (F=3.64, df=1, 61, n.s.) or gender-birth cohort interaction (F=2.10, df=2, 61, n.s.). Comparisons of a variety of clinical symptom variables showed no significant differences between men and women with eating disorders.
Table 2 presents rates of lifetime psychiatric comorbidity for the three groups. Compared with men without eating disorders, men with eating disorders had significantly higher rates in virtually all areas of comorbidity assessed, with significant odds ratios ranging from 2.84 to 8.94. By contrast, their rates showed few statistical differences from those of their female counterparts with eating disorders.
Further analysis showed that men with eating disorders had higher rates of having one (χ2=23.18, df=2, p<0.001), two or more (χ2=28.73, df=2, p<0.001), or three or more (χ2=52.85, df=2, p<0.001) comorbid psychiatric diagnoses compared with men without eating disorders.
We compared the men with and without eating disorders on a wide variety of family history and early life experience variables, as we had in a previous report on women with eating disorders (11). Men with and without eating disorders did not differ on the majority of these variables. Women with eating disorders reported higher rates of sexual abuse (odds ratio=4.79) and serious sexual abuse (odds ratio=6.25) than men with eating disorders. In general, rates for men with eating disorders fell in between those for women with eating disorders and men without eating disorders.
Table 3 presents quality of life variables. Although overall satisfaction ratings were fairly high, men with eating disorders reported more problems and less satisfaction on virtually all variables than men without eating disorders, but men with eating disorders were statistically indistinguishable from women with eating disorders.
Discussion
To our knowledge, these results represent the first detailed examination of a group of males with full and partial syndrome eating disorders in the community. It is important to consider the validity of our sample. Despite the respectable size of the total sample, the number of men who met all the criteria for an eating disorder was very small. The addition of men who met most of the criteria to our analysis may have biased the results of our study. However, previous comparisons of full and partial bulimia nervosa derived from the same data set showed few differences on the variables reported here, suggesting some validity to the strategy we used. In addition, several other authors (12, 13) have made similar comparisons pooling patients with full and partial syndromes.
Two further limitations to the study include the lack of assessment of most axis II variables in the initial survey and our inability, because of limitations in the questionnaire based on DSM-III-R, to estimate reliably the prevalence of binge-eating disorder (which was introduced in DSM-IV).
Other studies of nonclinical samples of men with full and partial eating disorders have also found that partial syndromes are more common in men than the full syndrome (13, 20, 21). In two articles reporting on comparisons between men and women, the ratios of partial to full eating disorders in women and men were 1.6:1 in one study (20) and 1.1:1 in the second (21). In our study, the rate was 2:1. In contrast, studies of samples derived from clinical populations have found the partial syndrome to be less common (5, 13). Few specific comparisons have been made between men with full and partial eating disorders in these reports, but data presented in these articles suggest that the male subjects with partial syndrome eating disorders were very similar to men with the full syndrome.
Our comparisons are interesting in several ways. We found few differences between men and women with eating disorders on the available clinical variables. The similar ratios of anorexia nervosa and bulimia nervosa in the two groups as well as the very similar patterns of age at onset and birth cohort effect add to the now substantial body of evidence suggesting that the illness is the same in nature for both sexes. The relatively small differences seen in prevalence of eating disorders when partial syndrome cases were considered is a new finding and deserves further study. In future work on this data set, we will attempt to determine whether these partial syndrome cases represent less severe illness or whether they are artifacts of the diagnostic hierarchies used to analyze the data.
Men with eating disorders showed striking differences from men without eating disorders. Although the significantly higher rates of psychiatric diagnoses in men with eating disorders than in those without eating disorders could be explained as a consequence of the eating disorders, they could also represent a factor leading these men to be more vulnerable to the development of an eating disorder. It is notable that there were few differences in rates of comorbidity between men and women with eating disorders, aside from the expected gender-specific differences in the rates of alcoholism and depression. The investigation of comorbidity may be a new avenue for the examination of how men with eating disorders differ from men without eating disorders. Several other studies have reported findings that are in keeping with this report in terms of higher rates of depression and substance abuse in men with eating disorders (5, 12, 13). Sexual orientation, although an obvious area of investigation, was deemed too sensitive a topic for a government-sponsored survey and unfortunately was not assessed.
Examination of variables assessing quality of life suggested that the quality of life of men with eating disorders was not as good as that of men without eating disorders. These results are more understandable as reactions to the existence of a severe, chronic illness, such as an eating disorder, rather than as factors that might have existed before the development of the eating disorder. These results also support the argument that eating disorders are similar for men and women in that both genders report similar levels of unhappiness with their current life situation.
In summary, our results lend credence to the hypothesis that eating disorders are similar illnesses in men and women. Our study also shows that the ratio of the occurrence of anorexia nervosa and bulimia nervosa, associated comorbidity, and psychosocial morbidity are very similar in both genders.
The question of whether men with eating disorders might be different from other men deserves further investigation. The results of this study suggest a qualified yes—they have more psychiatric disorders and appear to suffer from greater life dissatisfaction than men without eating disorders. Further examination of these variables might shed some additional light on factors that predispose both men and women to the development of an eating disorder.
 |
 |
 |
Presented in part at the Seventh International Conference on Eating Disorders, New York, April 26–28, 1996. Received April 29, 1998; revisions received Nov. 22, 1999, and Aug. 2, 2000; accepted Oct. 16, 2000. From the Department of Psychiatry, The Toronto Hospital Centre for Addiction and Mental Health, and the Department of Psychiatry, University of Toronto. Address reprint requests to Dr. Woodside, Department of Psychiatry, The Toronto Hospital, 200 Elizabeth St., Toronto, Ont., Canada M5G 2C4; [email protected] (e-mail). Supported by grants from the Ontario Ministry of Health and the Ministry of Community and Social Services to the Ontario Mental Health Foundation. The authors thank Ms. Cathy Spegg for assistance in the analysis of the data, Ms. Shirley Sinclair for assistance in the preparation of the manuscript, and the investigators from the Clarke Institute and McMaster University, chaired by Dr. Dan Offord, for designing and implementing the survey.
1. Morton R: Phthisologica, or, A Treatise of Consumption. London, S Smith and B Walford, 1694Google Scholar
2. Bruch H: Eating Disorders: Anorexia Nervosa, Obesity, and the Person Within. New York, Basic Books, 1973Google Scholar
3. Cobb S: Borderlines of Psychiatry. Cambridge, Mass, Harvard University Press, 1950Google Scholar
4. Selvini-Palazolli M: The meaning of body for anorexia nervosa patients: psychotherapeutic implications, in Proceedings of the 6th International Congress on Psychotherapy. Basel, Switzerland, Karger, 1965, pp 96–103Google Scholar
5. Carlat DJ, Camargo CA Jr, Herzog DB: Eating disorders in males: a report on 135 patients. Am J Psychiatry 1997; 154:1127–1132Google Scholar
6. Herzog DB, Norman DK, Gordon C, Pepose M: Sexual conflict and eating disorders in 27 males. Am J Psychiatry 1984; 141:989–990Link, Google Scholar
7. Crisp AH, Burns T: Primary anorexia nervosa in the male and female: a comparison of clinical features and prognosis, in Males With Eating Disorders. Edited by Andersen AE. New York, Brunner/Mazel, 1990, pp 77–99Google Scholar
8. Edwin DH, Andersen AE: Psychometric testing in 76 males with eating disorders. Ibid, pp 116–130Google Scholar
9. Woodside DB, Garner DM, Rockert W, Garfinkel PE: Eating disorders in males: insights from a clinical and psychometric comparison with females. Ibid, pp 100–115Google Scholar
10. Sharp CW, Clark SA, Dunan JR, Blackwood DHR, Shapiro CM: Clinical presentation of anorexia nervosa in males:24 new cases. Int J Eat Disord 1994; 15:125–134Google Scholar
11. Woodside DB, Kaplan AS: Day hospital treatment in males with eating disorders—response and comparison to females. J Psychosom Res 1994; 38:471–475Crossref, Medline, Google Scholar
12. Olivardia R, Pope HG Jr, Mangweth B, Hudson JI: Eating disorders in college men. Am J Psychiatry 1995; 152:1279–1285Google Scholar
13. Striegel-Moore RH, Garvin V, Dohm FA, Rosenheck RA: Psychiatric comorbidity of eating disorders in men: a national study of hospitalized veterans. Int J Eat Disord 1999; 25:399–404Crossref, Medline, Google Scholar
14. Offord DR, Boyle MH, Campbell D, Cochrane J, Goering PN, Lin E, Rhodes A, Wong M: Mental Health in Ontario: Selected Findings From the Mental Health Supplement to the Ontario Health Survey. Toronto, Queen’s Printer for Ontario, 1990Google Scholar
15. Boyle MH, Offord DR, Campbell D, Catlin G, Goering P, Lin E, Racine YA: Mental Health Supplement to the Ontario Health Survey: methodology. Can J Psychiatry 1996; 41:549–558Crossref, Medline, Google Scholar
16. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB: Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry 1995; 152:1052–1058Google Scholar
17. Wittchen H-U: Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 1994; 28:57–84Crossref, Medline, Google Scholar
18. Kessler RC, Olfson M, Berglund PA: Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am J Psychiatry 1998; 155:62–69Link, Google Scholar
19. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
20. Taraldsen KW, Eriksen L, Gotestam KG: Prevalence of eating disorders among Norwegian women and men in a psychiatric outpatient unit. Int J Eat Disord 1996; 20:185–190Crossref, Medline, Google Scholar
21. Szabo P, Tury F: Prevalence of clinical and subclinical forms of anorexia and bulimia nervosa among working females and males. Orv Hetil 1995; 136:1829–1835Google Scholar



