One-Year Recovery and Relapse Rates of Children With a Prepubertal and Early Adolescent Bipolar Disorder Phenotype
Abstract
OBJECTIVE: The study examined 1-year recovery and relapse rates for mania in subjects who met criteria for a prepubertal and early adolescent bipolar disorder phenotype. METHOD: Outpatients identified by consecutive new-case ascertainment were assessed by means of separate child and parent interviews, consensus conferences, and blind best estimates. The definition of the prepubertal and early adolescent bipolar disorder phenotype was DSM-IV mania with elation and/or grandiosity as one criterion. RESULTS: Of 93 subjects seen at baseline, 89 were seen at 1 year (95.7% retention). The rate of recovery from mania was 37.1%, and the rate of relapse after recovery was 38.3%. No covariates were significantly associated with recovery or relapse. CONCLUSIONS: The low recovery and high relapse rates supported the study hypothesis of poor outcomes, which was made on the basis of similarity between the characteristics of the prepubertal and early adolescent bipolar disorder phenotype (long episode duration and high prevalence of mixed mania, psychosis, and rapid cycling) and those of severe bipolar disorder in adults.
Studies of adults with bipolar disorder have reported a childhood onset in as many as 59% of cases (1) and earlier onset of bipolar disorder in more recently born cohorts (2). Therefore, it is expected that more adult bipolar disorder patients will give histories of childhood mania and that knowledge about a prepubertal and early adolescent bipolar disorder phenotype will aid practitioners.
This paper reports 1-year recovery and relapse rates from an ongoing study of the characteristics and course of a prepubertal and early adolescent bipolar disorder phenotype (3–5). To our knowledge, this is the first report of such data.
Method
Subjects were recruited by consecutive new-case ascertainment from pediatric and psychiatric sites (3, 4). A method for differentiating prepubertal and early adolescent bipolar disorder phenotype from attention deficit hyperactivity disorder (ADHD) was needed, because symptoms such as hyperactivity and distractibility are criteria for both mania and ADHD. To address this need, the prepubertal and early adolescent bipolar disorder phenotype required current mania or hypomania with elation and/or grandiosity as one criterion (3–5). Use of this phenotype permitted a diagnosis of mania without the use of the criteria that overlapped with those for ADHD, ensured that subjects had at least one of the two cardinal features of mania (i.e., elation and grandiosity), and allowed investigation of a child phenotype that was most likely to be continuous with adult bipolar disorder (3–5).
A comprehensive battery was given at baseline and at 6 and 12 months to mothers and children separately. Research nurses were blinded to the subjects’ diagnosis at baseline because the subjects with the prepubertal and early adolescent bipolar disorder phenotype were interviewed concurrently with two comparison groups without bipolar disorder (3, 4). Psychopathology was assessed with a semi-structured interview, the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) (4, 6), and in consensus conferences that examined all research, school, and medical records. Research nurses were trained to 100% interrater reliability on five consecutive interviews (as both interviewer and observer) for each WASH-U-KSADS item (6). In addition, interrater reliability between on-site WASH-U-KSADS mania ratings and off-site blind ratings (made on the basis of the narrative documentation that accompanies each WASH-U-KSADS mania item) were excellent (kappa=0.74–1.00) (6). Six-month stability of both bipolar disorder diagnoses (85.7%) and individual mania criteria were also very high (5). Furthermore, the WASH-U-KSADS has been validated in comparison with parent and teacher reports (6). Subjects needed to have a Children’s Global Assessment Scale (7) score of ≤60 to ensure moderate or severe impairment. Naturalistic treatment data were collected with the Longitudinal Interval Followup Evaluation (8), and puberty was determined with the Duke scale (9). “Mixed mania” was identified on the basis of overlapping time periods for the WASH-U-KSADS items on mania/hypomania and major depressive disorder. Rapid cycling was defined as four episodes per year (3, 4). Ultrarapid cycling was defined as five to 364 and ultradian as ≥365 episodes per year, respectively (3, 4). In ultradian cycling, mania needed to occur for ≥4 hours per day (3, 4). Recovery was defined as no syndromal DSM-IV mania or hypomania for ≥2 weeks, and relapse was defined as syndromal criteria for mania or hypomania and a Children’s Global Assessment Scale score of ≤60 for ≥2 weeks. After complete description of the study to parents and children, written informed consent was obtained from parents and written assent was obtained from children. Recovery and relapse were estimated with the Kaplan-Meier statistic. Cox modeling was used to test covariates, which included baseline age; gender; puberty status; presence of mixed mania, psychosis, ultradian rapid cycling, comorbid ADHD, comorbid oppositional defiant disorder, or comorbid conduct disorder; and use of antimanic medication. Antimanic medication was defined as neuroleptics, anticonvulsants, and lithium. Details of medication use were reported previously (5).
Results
Four of the 93 subjects with the prepubertal and early adolescent bipolar disorder phenotype interviewed at baseline dropped out by 1 year (95.7% retention). There were no significant demographic differences between dropouts and continuers. Baseline characteristics of the 89 subjects seen at 1 year included: mean age=10.9 years (SD=2.7), current episode duration=3.6 years (SD=2.5), and Children’s Global Assessment Scale score=43.3 (SD=7.7). Fifty-one subjects (57.3%) were prepubertal. Eighty subjects (89.9%) showed elation, and 76 (85.4%) showed grandiosity. Fifty-three subjects (59.6%) met criteria for psychosis, 48 (53.9%) for mixed mania, 69 (77.5%) for ultradian rapid cycling, 77 (86.5%) for ADHD, and 67 (75.3%) for oppositional defiant disorder. Only 45 subjects (50.6%) were taking an antimanic drug from baseline to 1 year. Recovery and relapse rates estimated with the Kaplan-Meier statistic were 37.1% (95% confidence interval [CI]=27.0–47.1) and 38.3% (95% CI=14.8–61.9), respectively (Figure 1). No covariates were significantly associated with recovery or relapse.
Discussion
Because the phenotype included elation and/or grandiosity, these findings may not generalize to other samples. Comparisons, however, are problematic due to differences in methods. Faraone et al. (10), for example, did not interview child subjects, used lay raters, did not use a scale developed for prepubertal mania, and ascertained for ADHD.
The low rate of antimanic drug use suggests that practitioners have not yet recognized cases of bipolar disorder in children (5). In this regard, WASH-U-KSADS definitions of elation and grandiosity are the same as the definitions of those DSM-IV criteria used in making a diagnosis of bipolar disorder in adults (4, 6), but the manifestations of the criteria are child age-dependent (11). For example, a grandiose bipolar disorder adult called the President to tell him how to run the country, while a manic child repeatedly called school officials to tell them how to run the school.
Adults with continuous rapid cycling have been reported to have a chronic, treatment-resistant course over decades (12). Follow-up of subjects with the prepubertal and early adolescent bipolar disorder phenotype will be necessary to establish if their ultradian cycling is child-age limited or continuous into an ultradian cycling adult-age course.
Received March 28, 2000; revision received Aug. 11, 2000; accepted Oct. 17, 2000. From the Department of Psychiatry, Washington University School of Medicine. Address reprint requests to Dr. Geller, Department of Psychiatry, Washington University School of Medicine, 660 S. Euclid Ave., Box 8134, St. Louis, MO 63110; [email protected] (e-mail). Supported by NIMH grant R01 MH-53063 (to Dr. Geller).
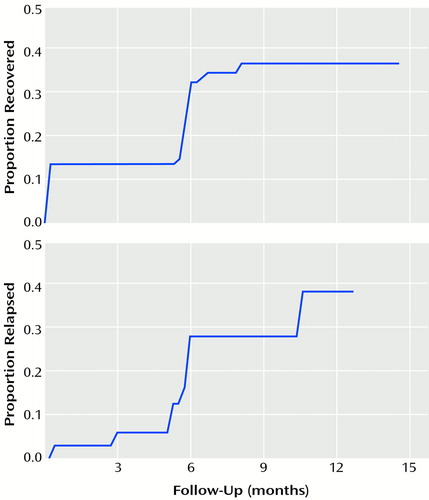
Figure 1. One-Year Recovery and Relapse Rates for 89 Subjects With a Prepubertal and Early Adolescent Bipolar Disorder Phenotypea
aRecovery and relapse rates estimated with the Kaplan-Meier statistic. Recovery rate=37.1% (95% CI=27.0–47.1); relapse rate=38.3% (95% CI=14.8–61.9).
1. Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM: The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994; 31:281–294Crossref, Medline, Google Scholar
2. Gershon ES, Hamovit JH, Guroff JJ, Nurnberger JI: Birth-cohort changes in manic and depressive disorders in relatives of bipolar and schizoaffective patients. Arch Gen Psychiatry 1987; 44:314–319Crossref, Medline, Google Scholar
3. Geller B, Williams M, Zimerman B, Frazier J, Beringer L, Warner K: Prepubertal and early adolescent bipolarity differentiate from ADHD by manic symptoms, grandiose delusions, ultra-rapid or ultradian cycling. J Affect Disord 1998; 51:81–91Crossref, Medline, Google Scholar
4. Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo CA: Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 2000; 10:157–164Crossref, Medline, Google Scholar
5. Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo CA: Six-month stability of a prepubertal and early adolescent bipolar disorder phenotype. J Child Adolesc Psychopharmacol 2000; 10:165–173Crossref, Medline, Google Scholar
6. Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello M, Soutullo C: Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry (in press)Google Scholar
7. Bird HR, Canino G, Rubio-Stipec M, Ribera JC: Further measures of the psychometric properties of the Children’s Global Assessment Scale. Arch Gen Psychiatry 1987; 44:821–824Crossref, Medline, Google Scholar
8. Keller MB, Lavori PW, McDonald-Scott P, Endicott J, Andreasen N, Van Eerdewegh MM: The reliability of retrospective treatment reports. Psychiatry Res 1983; 9:81–88Crossref, Medline, Google Scholar
9. Duke PM, Litt IF, Gross RT: Adolescents’ self-assessment of sexual maturation. Pediatrics 1980; 66:918–920Medline, Google Scholar
10. Faraone SV, Biederman J, Mennin D, Wozniak J, Spencer T: Attention-deficit hyperactivity disorder with bipolar disorder: a familial subtype? J Am Acad Child Adolesc Psychiatry 1997; 36:1378–1387Google Scholar
11. Geller B, Luby J: Child and adolescent bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1997; 36:1168–1176Google Scholar
12. Goodwin FK, Jamison KR: Manic-Depressive Illness. New York, Oxford University Press, 1990, pp 22–55, 127–151Google Scholar



