Clozapine-Associated Reduction in Arrest Rates of Psychotic Patients With Criminal Histories
Abstract
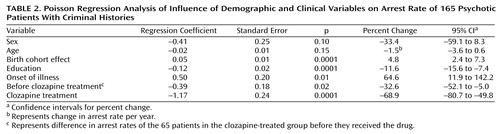
OBJECTIVE: The authors examined the relationship between treatment with clozapine and rates of arrest of psychotic outpatients with criminal histories. METHOD: Patients who had been given a DSM-IV psychotic diagnosis were selected from an urban outpatient clinic database. Background checks performed on 360 patients identified 165 (45.8%) with positive criminal histories in Massachusetts. The authors reviewed the charts of these patients to determine several variables, including whether and when they had received clozapine. A Poisson regression model was used to regress arrest rates against the variables of age, sex, onset of illness, birth cohort, and clozapine treatment. Risk ratios (i.e., percent change in arrest rates) were then calculated by computing the exponential of the Poisson regression coefficients. RESULTS: The 165 patients included in the analysis had a total of 1,126 arrests. The mean number of arrests was 6.8. Differences were found between the 65 patients who received clozapine and the 100 patients who did not in number of arrests, sex, and onset of illness. The regression revealed significantly higher arrest rate estimates associated with more recent birth cohort (4.8%) and with onset of illness (64.6%) and lower arrest rate estimates associated with higher levels of education (11.6%), receiving clozapine (32.6%), and receiving clozapine during specific periods of time (68.9%). CONCLUSIONS: Clozapine’s effect on arrest rates in this group of patients is large enough to warrant further investigation. The data indicate that clozapine may reduce recidivism in subjects with criminal histories who are in need of antipsychotic medication.
The relationship between the mental health system and the criminal justice system is not fully understood. Studies conducted before deinstitutionalization showed that the mentally ill commit crimes at similar or lower rates than the general population (1, 2). More recent studies have demonstrated higher rates of criminal behavior for the mentally ill than for those who are not mentally ill (3, 4), prompting the question of whether criminalization of the mentally ill has occurred (5). In 1939, after noting that a rise in inpatient psychiatric populations corresponded with a decline in penal populations, Penrose (6) suggested that society tolerates a finite level of aberrant behavior, resulting in confinement of those whose behaviors exceed this limit. In society today a converse trend is apparent; studies indicate that between 6% and 15% of those incarcerated suffer from a major mental illness (7).
Studies examining factors contributing to arrests of the mentally ill have demonstrated four points. First, socioeconomic and demographic factors associated with an increased rate of crime in the general population are associated with crime in the mentally ill as well. These include youth, male sex, and low socioeconomic status (8) as well as history of previous arrests (9). Second, people with major mental illness who are arrested are likely to be noncompliant with medication (4) and exhibiting symptoms at the time of the offense (10). Third, people who have had multiple psychiatric admissions are more likely to be arrested (11). Finally, substance abuse is a predictor of criminal history among psychotic patients (8).
Few studies have examined the impact of treatment on recidivism, and, to our knowledge, none has looked at a specific agent in relationship to criminal behavior in psychotic illness. The atypical antipsychotic clozapine has been found to possess properties that would be expected to reduce criminal behavior in the mentally ill. Specifically, compared with conventional antipsychotics, clozapine is associated with lower rates of hospitalization (12), higher rates of treatment compliance (13), and less violent and aggressive behavior (14). In addition, case reports (15) and one retrospective study (16) have noted a decrease of substance abuse in patients with both a psychotic disorder and a substance abuse disorder who were treated with clozapine.
In the present study, we investigated the arrest rate of patients with psychotic illness who were treated in an urban mental health clinic. Specifically, our hypothesis was that clozapine treatment would reduce arrest rates. We generated this hypothesis in the course of working on a court evaluation unit, where we noticed that none of the patients who were being arrested and subsequently referred for forensic evaluation were receiving clozapine.
Method
Study Group
The Freedom Trail Clinic is an outpatient mental health clinic in an urban community. Five hundred fifty patients are followed through this clinic, which has a catchment area of 160,000 people. Typically, the clinic population consists of patients with low socioeconomic status who have chronic mental illnesses.
After the study was approved by our institutional review board, the names, birth dates, and Social Security numbers of all patients given a DSM-IV diagnosis of psychotic disorder were obtained from the database of the clinic. The diagnoses included were schizophrenia (all types), bipolar illness, depression with psychotic features, substance-induced psychotic disorder, psychosis secondary to a general medical condition, delusional disorder, brief and shared psychotic disorder, and psychosis not otherwise specified. This search yielded 378 patients followed at the clinic who had been given a psychotic diagnosis.
The names, birth date, and Social Security numbers of these patients were submitted to the Commonwealth of Massachusetts Criminal History Systems Board in compliance with the regulations pertaining to research (803 CMR 8:01–8:03). These regulations allow for criminal background checks to be performed in the Commonwealth of Massachusetts, without consent, provided the research is conducted for valid educational, scientific, or other public purposes. Researchers are held to a strict standard for maintaining subject anonymity; therefore, only one investigator (W.G.F.) had access to the criminal background data.
The criminal background data included the dates of arrests in Massachusetts as well as the nature and disposition of the charges. All background checks that indicated an arrest for criminal activity were verified to ensure that they contained the correct demographic information. However, we were unable to determine the rate of false negatives, which may occur using background checks as an instrument to determine outcome. We must assume that a small but distinct percentage of false negatives occurred because of clerical errors, the use of aliases, computer errors, and the like. We did not feel that this would influence our study substantially because we were interested in repeat offenders.
Of the 378 names submitted, data were missing for one and 17 were not fully processed by the Criminal Histories Systems Board, leaving 360 subjects on whom background checks were performed. Of these, 175 (48.6%) had at least one previous arrest.
A review was then conducted of the charts of these 175 patients. Data gathered included date of birth, race, sex, psychiatric diagnosis, date of onset of illness, and level of education. The dates of treatment with clozapine were also obtained for the patients who received this medication. These data were gathered from the charts of the patients in the study group by one of us (C.C.) to ensure reliability. Of the initial 175 patients, 10 were seen at the clinic less than twice and were excluded from the study. Data were analyzed for 165 patients; 65 (39.4%) of these patients had been treated with clozapine.
Subjects were considered to have an arrest point on a given date on the basis of the criminal background check. Dates that contained multiple charges were counted as one arrest point.
Data Analysis
Demographic characteristics were examined for differences between the 100 patients who had never received treatment with clozapine and the 65 who had received this medication. Chi-square tests were used when comparing categorical variables, and two-tailed Student’s t tests were used for continuous variables.
To address the question of influences on criminal behavior, arrest rates were regressed against several predictor variables in a longitudinal Poisson regression model. To determine arrest rate, we divided each subject’s course into 2-year intervals starting at his or her 18th birthday. In addition, an interval was further divided if the subject changed status within the interval with regard to the variables of interest (i.e., onset of the diagnosed illness, start of treatment with clozapine, end of treatment with clozapine, or end of the study period). The number of arrests of each subject was counted for each interval. Those counts were considered as Poisson-distributed and regressed against covariates of interest (the SAS procedure GENMOD was used) with exchangeable correlation (compound symmetry) of observations for the same subject. The exchangeable correlation structure assumes that each subject has his or her own specific arrest rate, which is then modified by factors such as age, onset of illness, and treatment.
The predictor variables in our Poisson regression model included age, sex, onset of illness, birth cohort, education level, and clozapine treatment. A risk ratio (i.e., percent change in arrest rates) was then calculated by computing the exponential of the regression coefficient (%[Δ]=[exp(coefficient)–1] × 100), which is similar to the way odds ratios are the exponential of logistic regression coefficients (17). We were unable to assess for changes in the nature of the charges because of the complexity that it would have added to the regression.
Results
Characteristics of the Study Group
The 165 patients with a positive criminal history in Massachusetts had a total of 1,126 arrests. The demographic characteristics of these patients are shown in Table 1. The mean number of arrests was 6.8 (SD=8.1, range=1–47, median=4, mode=1 [the mode occurred 36 times]). The percentage of subjects with one arrest was similar in the clozapine-treated group (21.5% [N=14]) and the group that had not received clozapine (22.0% [N=22]). The mean number of arrests of the 65 patients who received clozapine was 5.1 (SD=4.8, range=1–23, median=4, mode=1). The mean number of arrests of the 100 patients who had not received clozapine was 7.9 (SD=9.5, range=1–47, median=4, mode=1). This skew of the arrest data toward lower numbers of arrests can be seen in Figure 1. The arrest data are presented for descriptive purposes. Individual arrest counts were not adjusted for length of the time window. This is best seen in the Poisson regression analysis (i.e., in the descriptive statistics, one arrest in a 2-year interval would be viewed the same as one arrest in a 6-month interval).
The mean age of all 165 patients was 43 years (SD=9.3); according to analysis of variance (ANOVA), patients who had or had not received clozapine did not differ in age (F=0.104, df=1, 163, n.s.). Men were more likely than women to have received clozapine (χ2=4.8, df=1, p<0.03), and Caucasian patients were more likely than African American or Hispanic patients to have received this medication, although the group sizes of the last two categories were small (χ2=5.8, df=2, p<0.06). Date of onset of illness could be determined for only 161 patients. Those treated with clozapine had a younger mean age at illness onset, 21.4 (SD=5.7) versus 23.9 (SD=8.7) (F=3.96, df=1, 159, p<0.05). No difference was found in level of education between the patients who did or did not receive clozapine.
Arrest Rates
The results from the Poisson regression of arrest rate against age, sex, onset of illness, birth cohort, education level, and clozapine treatment are shown in Table 2. All coefficients were in the expected direction, and all were adjusted for the other predictors in the model. A decrease of approximately 2% per year in arrests was observed for the entire study group; this was not statistically significant but was left in the model because previous studies have demonstrated an association between age and number of arrests (18).
The significant birth cohort effect indicates that patients born in earlier decades had fewer arrests independent of age. This is consistent with other studies that have examined this effect (19). A 65% increase in arrest rates was observed to coincide with the onset of the illness. Higher education levels were significantly associated with lower arrest rates.
Breaking the study group down into those treated with clozapine and those who did not receive clozapine revealed two findings. First, before receiving this medication, the patients who received clozapine had lower rates of arrest than the patients who never received clozapine. Second, the arrest rates of the patients taking clozapine were significantly lower while they were taking the drug than before they were given the drug.
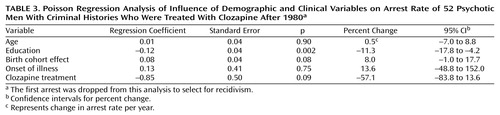
Finally, in an attempt to address the confounding factors of sex, birth cohort, the fact that clozapine was not in use until the late 1980s, and the large number of individuals with only one arrest in the study group, we reanalyzed a subset of the data. This subset consisted of data for men who were receiving clozapine, after the year 1980, with the first arrest dropped to select for recidivism. Data for 52 men were included in this analysis. As shown in Table 3, the results of this analysis are similar to the results for entire data set but with less statistical significance because of the reduced group size.
Discussion
To our knowledge, this study is the first to look at the effect of a single agent on criminal behavior of patients with psychotic illness. Within the limitations of the study, arrests appeared to decrease for patients taking clozapine. The reduction in arrest rates after patients started to take the drug was significant after age, sex, birth cohort, onset of illness, and education were controlled for.
Several confounding variables complicate the attribution of lower arrest rates to clozapine. Because treatment with clozapine demands weekly or biweekly blood draws, it is possible that one of the reasons these patients were selected for clozapine treatment was their greater compliance with treatment. Consistent with this possibility, before they started to take clozapine, patients in the clozapine group had lower mean arrest rates than the patients who never received the drug. However, clozapine produced a significant reduction in arrest rates above and beyond the baseline group effect.
It is possible that the clozapine treatment system rather than clozapine’s pharmacological effect contributed to the reduction in arrest rates because the treatment system includes frequent check-ins with a clinician. It could also be argued that improvements in cognition and organization associated with clozapine do not prevent criminal behavior but prevent getting arrested for such behavior. Although we do not believe this was a factor, it highlights problems that arise when using arrests as a measure of criminal behavior. It is difficult to prove our assumption that each patient has his or her own arrest rate modified by factors such as treatment, illness, and age. Arrests are the result of multiple factors and may not be a particularly valid measure of criminal behavior. The police officer on the scene makes the decision as to whether a person is arrested or brought to a hospital. This decision is influenced by a complex interaction between the severity of mental illness overtly demonstrated by the suspect and the severity of the crime (20).
The regression of clozapine treatment was confounded by age because many of the patients treated with clozapine received treatment through the end of the study. This factor is corrected for somewhat by including patients who did not receive clozapine in the age regression, allowing us to look at the age effect with less influence by treatment. In addition, we did not take into account the amount of time spent incarcerated or in the hospital, when the patients would not be counted as receiving clozapine and would have lower arrest rates due to less opportunity. This would bias the data toward reducing the effect of clozapine on arrest rates.
To the degree that clozapine reduces hospitalization rates, it increases the time that an individual patient is at risk for arrest, which would further diminish our ability to detect a pharmacological effect of clozapine on criminal behavior. Alternatively, at least one study (11) has identified lifetime number of arrests as being positively associated with lifetime number of psychiatric hospitalizations, so reducing hospitalization rates with clozapine may reduce arrest rates.
Further complicating the interpretation of our results is the fact that we were not able to include a variable for patients with both a psychotic illness and a substance abuse disorder. This is potentially quite important because substance abuse is a well-known contributor to criminal behavior. As noted, clozapine has the potential to reduce substance abuse in patients with both a psychotic illness and a substance abuse disorder (16). In addition, a recent study (21) has demonstrated that patients with both schizophrenia and a substance abuse disorder have shorter hospitalizations and more rapid improvement than patients with schizophrenia who do not have a substance abuse disorder. This is another important indicator that patients with substance abuse disorders respond differently to standard treatments.
The most important limitations of this study arise from the retrospective, naturalistic design. Because arrests are relatively infrequent events, a large, prospective, randomized trial of substantial duration will be necessary to provide a more rigorous test of our hypothesis.
Several points in our results bear further discussion. The observation that arrest rates increase by 65% after the onset of mental illness is an important one. This would seem to indicate that illness is playing some role in the arrests of these patients. We also observed a significant birth cohort effect, which predicts that a 20-year-old with psychosis in 1980 would be more likely to be arrested than a 20-year-old with psychosis in 1950. Taken together, these two observations further support the idea that criminalization of mental illness occurred during the period for which arrest data were available.
In conclusion, the effect of clozapine on arrest rates is large enough to warrant further investigation and to make some preliminary statements about treatment in patients with psychotic illness who have histories of criminal behavior. Our data indicate that clozapine may reduce recidivism in a criminal population in need of antipsychotic medication. Unfortunately, due to financial considerations, there is a propensity to underuse clozapine in correctional settings (22). The apparent reduction in criminal behavior associated with clozapine treatment is an important factor that requires further study. If it is replicated, it should be weighed carefully in the consideration of treatment options for forensic patients with psychosis.
 |
 |
 |
Presented in abstract form at the 2000 New Clinical Drug Evaluation Unit Annual Meeting, June 1, 2000. Received April 6, 2000; revisions received Aug. 2 and Sept. 24, 2000; accepted Aug. 31, 2000. From the Freedom Trail Clinic, Boston; and the Schizophrenia Program and Biostatistics Unit, Massachusetts General Hospital and Harvard Medical School Consolidated Department of Psychiatry. Address reprint requests to Dr. Frankle, Massachusetts General Hospital, Department of Psychiatry, MGH/McLean Residency, 50 Staniford St., 5th Floor, Boston, MA 02114-2517; [email protected] (e-mail). Support for statistical analysis was provided by the Massachusetts General Hospital Department of Psychiatry’s Biostatistics Unit.
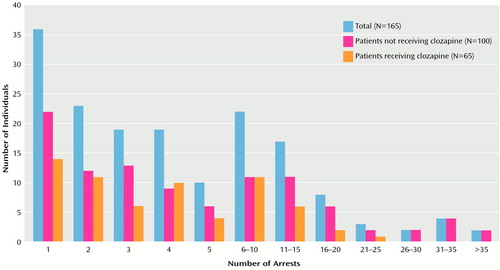
Figure 1. Distribution of Arrest Data for 165 Psychotic Patients With Criminal Histories Who Were or Were Not Treated With Clozapine
1. Pollack H: Is the paroled patient a menace to the community? Psychiatr Q 1938; 12:236–244Google Scholar
2. Cohen D, Freeman H: How dangerous to the community are the state hospital patients? Conn State Med J 1945; 9:697–700Google Scholar
3. Coid B, Lewis S, Reveley A: A study of psychosis and criminality. Br J Psychiatry 1993; 162:87–92Crossref, Medline, Google Scholar
4. McFarland BH, Faulkner LR, Bloom JD, Hallaux R, Bray JD: Chronic mental illness and the criminal justice system. Hosp Community Psychiatry 1989; 40:718–723Abstract, Google Scholar
5. Abramson M: The criminalization of mentally disordered behavior: possible side effects of a new mental health law. Hosp Community Psychiatry 1972; 23:101–105Abstract, Google Scholar
6. Penrose L: Mental disease and crime: outline of a comparative study of European statistics. Br J Med Psychol 1939; 18:1–15Crossref, Google Scholar
7. Lamb HR, Weinberger LE: Persons with severe mental illness in jails and prisons: a review. Psychiatr Serv 1998; 49:483–492Link, Google Scholar
8. Muntaner C, Wolyniec P, McGrath J, Pulver A: Arrest among psychotic inpatients: assessing the relationship to diagnosis, number of admissions, and social class. Soc Psychiatry Psychiatr Epidemiol 1998; 33:274–282Crossref, Medline, Google Scholar
9. Draine J, Solomon P, Meyerson A: Predictors of reincarceration among patients who received psychiatric services in jail. Hosp Community Psychiatry 1994; 45:163–167Abstract, Google Scholar
10. Kunjukrishnan R, Bradford J: Schizophrenia and major affective disorder: forensic psychiatric issues. Can J Psychiatry 1988; 33:723–733Crossref, Medline, Google Scholar
11. Solomon P, Draine J: Explaining lifetime criminal arrests among clients of a psychiatric probation and parole service. J Am Acad Psychiatry Law 1999; 27:239–251Medline, Google Scholar
12. Luchins DJ, Hanrahan P, Shinderman M, Lagios L, Fichtner CG: Initiating clozapine treatment in the outpatient clinic: service utilization and cost trends. Psychiatr Serv 1998; 49:1034–1038Google Scholar
13. Rosenheck R, Cramer J, Xu W, Thomas J, Henderson W, Frisman L, Fye C, Charney D: A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. N Engl J Med 1997; 337:809–815Crossref, Medline, Google Scholar
14. Glazer W, Dickson R: Clozapine reduces violence and persistent aggression in schizophrenia. J Clin Psychiatry 1998; 59(suppl 3):8–14Google Scholar
15. Albanese MJ, Khantzian EJ, Murphy SL, Green AI: Decreased substance use in chronically psychotic patients treated with clozapine (letter). Am J Psychiatry 1994; 151:780–781Medline, Google Scholar
16. Buckley P, Thompson PA, Way L, Meltzer HY: Substance abuse and clozapine treatment. J Clin Psychiatry 1994; 55(Sept suppl B):114–116Google Scholar
17. Diggle P, Liang K, Zeger S: Analysis of Longitudinal Data. New York, Clarendon Press, 1994, pp 162–166, 242Google Scholar
18. Harry B, Steadman H: Arrest rates of patients treated at a community mental health center. Hosp Community Psychiatry 1988; 39:862–866Abstract, Google Scholar
19. Hodgins S: Epidemiological investigations of the associations between major mental disorders and crime: methodological limitations and validity of the conclusions. Soc Psychiatry Psychiatr Epidemiol 1998; 33(suppl 1):29–37Google Scholar
20. Lamb HR, Grant RW: The mentally ill in an urban county jail. Arch Gen Psychiatry 1982; 39:17–22Crossref, Medline, Google Scholar
21. Ries R, Russo J, Wingerson D, Snowden M, Comtois K, Srebnik D, Roy-Byrne P: Shorter hospital stays and more rapid improvement among patients with schizophrenia and substance disorders. Psychiatr Serv 2000; 51:210–215Link, Google Scholar
22. Pinals DA, Buckley PF: Novel antipsychotic agents and their implications for forensic psychiatry. J Am Acad Psychiatry Law 1999; 27:7–22Medline, Google Scholar



