Antidepressant Treatment of Depression in the Finnish General Population
Abstract
OBJECTIVE: Antidepressant use has increased in the last decade, but whether depression continues to be undertreated is unknown. The authors investigated the prevalence of antidepressant treatment and its predictors in a recent general population sample of depressed subjects. METHOD: As part of the Finnish Health Care Survey, in 1996 a representative sample of Finns (N=5,993) aged 15–75 years underwent a standardized face-to-face interview that used the DSM-III-R criteria for major depressive episode. RESULTS: Only 13% of subjects with a major depressive episode during the preceding 12 months (70 of 557) reported current use of an antidepressant. In logistic regression models, use of psychiatric services for depression, regular use of any other medication, more than 1 month of sick leave, and smoking were associated with antidepressant treatment. CONCLUSIONS: Most depressed subjects in 1996 in Finland were not receiving antidepressant treatment despite the several-fold increase in antidepressant use in the 1990s.
From general population studies there is overwhelming evidence of serious undertreatment of individuals with depression (1). However, since the introduction of the newer antidepressants, antidepressant use has grown markedly worldwide. For example, in Finland antidepressant use increased over fourfold between 1989 and 1998 after the introduction of selective serotonin reuptake inhibitors (SSRIs) (2). Is depression still undertreated?
Only a minority of people with depression seek treatment. In the National Comorbidity Survey only 28% of the respondents with major depression (in 1990 to 1992) reported having used health care services during the previous year because of their symptoms (3); comparable findings emerged from a telephone interview study in the Toronto metropolitan area in 1996–1997 (4). In two general population studies undertaken between 1988 and 1994, just 7% of young adults with a current major depressive episode (5) and 18% of subjects with a major depressive episode in the past year (6) were currently taking antidepressant medication. In the European DEPRES II study (7), 30% of depressed subjects with health care contact in 1994 were receiving antidepressant treatment. However, both help seeking and provision of treatment may have increased over time. In the present study we investigated the prevalence of antidepressant use among subjects with a major depressive episode in the Finnish general population in 1996.
Method
The present study formed part of the Finnish Health Care Survey, in which subjects in a random population sample of Finns were interviewed face-to-face by professional interviewers in 1996 (8). The sample analyzed comprised 5,993 subjects aged 15–75 years (details of sampling are provided in references 8 and 9). The depression section of the Short Form of the University of Michigan Composite International Diagnostic Interview (9, 10), including the DSM-III-R criteria for major depressive episode, was used to assess depression. The overall diagnostic agreement of the short form with the full Composite International Diagnostic Interview for major depressive episode is 93% (10). The age-adjusted prevalence of depression during the preceding 12 months was 9.3% (N=557) (9). The interview also included questions concerning the use of health care services and all medication use. All subjects participating in this study gave formal consent.
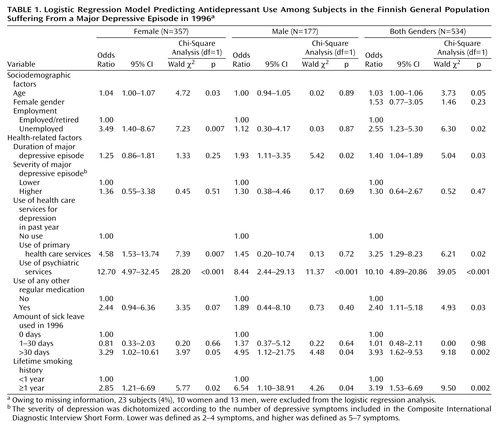
Age, gender, severity and duration of the major depressive episode, number of chronic conditions, number of medications, duration of sick leave (during 1996, irrespective of diagnosis), marital status, family income, education, employment, type of residential area, alcohol use, and smoking status were the variables chosen for logistic regression models, with antidepressant use as the dependent variable. All these variables were first analyzed alone in logistic regression models adjusted for age, sex, and the severity and duration of the major depressive episode. The final multivariate logistic regression model for antidepressant use included all the significant variables (p<0.05) adjusted as just described. The severity of depression was dichotomized according to the number of depressive symptoms included in the Composite International Diagnostic Interview Short Form: lower (3–5 symptoms) versus higher (6–8 symptoms). Age and duration of the major depressive episode were examined as continuous variables, the latter in 3-month intervals. Primary health care services included care provided by health centers and occupational public, private, and other medical services; psychiatric services included public and private services provided by a psychiatrist. SPSS version 9.0 was used for statistical analyses (Chicago, SPSS).
Results
Of the 557 subjects with a major depressive episode during the previous 12 months, 27% (151 of 557) reported that they had used health care services because of their depressive symptoms. Only 11% (61 of 557) had used primary health care services, another 16% (90 of 557) had used psychiatric services. Of the subjects with a major depressive episode, 13% (70 of 557) reported current use of antidepressant medication. Novel antidepressants such as SSRIs and moclobemide were used by 41 subjects, while 38 used other antidepressants, mainly tricyclic antidepressants. Benzodiazepine medication was used by 14% (77 of 557), and 4% (22 of 557) used neuroleptic medication; overall, 23% of the subjects with a major depressive episode (126 of 557) reported any use of psychotropic medication.
The main predictors of antidepressant use (Table 1) were the use of psychiatric services for depression, cumulative sick leave of more than 1 month, smoking for more than 1 year, and any other regular use of medication. In gender-specific analyses the duration of the major depressive episode was associated with antidepressant use among men, while older age, the use of primary health care services for depression, and unemployment were associated with antidepressant use among women.
Discussion
We found that in the Finnish general population in 1996, depression was still largely undertreated, despite the several-fold increase in the use of antidepressants during the 1990s. Only 13% of the subjects with a major depressive episode during the previous year currently received antidepressant medication.
We know of no other large-scale general population studies conducted with face-to-face interviews for which there are reports of antidepressant use for depression in the latter half of the 1990s. While this study was based on a large, nationally representative general population sample (8, 9), used a standardized interview to determine the presence of depression (9, 10), and carefully evaluated the use of medication, some methodological limitations exist. Information on medications was restricted to current use, while the prevalence of major depressive episodes involved the preceding 12 months. Subjects may thus have used antidepressants and discontinued that treatment before the interview. However, even among subjects with current or very recent major depressive episodes, the prevalence of antidepressant use never exceeded 25%. This limitation is thus unlikely to have undermined the validity of the overall finding of undertreatment, although it may have caused underestimation of antidepressant use. Nonmedical treatments of depression were not investigated. Finally, our findings concern major depressive episode, not strictly defined unipolar major depression.
In studies from the late 1980s and early 1990s (5–7) and a recent telephone interview study (4), 7%–18% of depressed subjects were receiving antidepressant treatment. The present finding from the latter 1990s that only 13% (up to 25% for recently diagnosed subjects) of people with major depressive episodes are using antidepressants suggests that still far too few depressed subjects receive antidepressant treatment.
We found, after controlling for the severity and duration of depression, that the use of psychiatric services because of depression was the strongest predictor of antidepressant treatment. This is consistent with findings from Ontario in 1990–1991 (6). The use of primary health care services was associated with antidepressant treatment only among women. Our findings also suggest that duration of sick leave may be a factor independently related to the use of antidepressants. Overall, our findings indicate that depression is still largely undertreated in the general population, despite the major increase in use of antidepressants in the 1990s.
 |
Received Nov. 28, 2000; revisions received April 9 and May 8, 2001; accepted May 11, 2001. From the Department of Mental Health and Alcohol Research, National Public Health Institute; the Department of Psychiatry, Helsinki City Eastern Health Center; and the Department of Psychiatry, University of Oulu, Finland. Address reprint requests to Dr. Isometsä, Department of Mental Health and Alcohol Research, National Public Health Institute, Mannerheimintie 166, FIN-00300 Helsinki, Finland; [email protected] (e-mail). Supported by the Finnish Foundation for Psychiatric Research. The authors thank Professor Jaakko Kaprio for statistical advice and Mr. Olli Kiviruusu for technical assistance.
1. Hirschfeld RMA, Keller MB, Panico S, Arons BS, Barlow D, Davidoff F, Endicott J, Froom J, Goldstein M, Gorman JM, Guthrie D, Marek RG, Maurer TA, Meyer R, Phillips K, Ross J, Schwenk TL, Sharfstein SS, Thase ME, Wyatt RJ: The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA 1997; 227:333-340Crossref, Google Scholar
2. Finnish Statistics on Medicines 1998. Helsinki, National Agency for Medicines and Social Insurance Institution, 1999Google Scholar
3. Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry 1999; 156:115-123Link, Google Scholar
4. Ohayon MM, Shapiro CM, Kennedy SH: Differentiating DSM-IV anxiety and depressive disorders in the general population: comorbidity and treatment consequences. Can J Psychiatry 2000; 45:166-172Crossref, Medline, Google Scholar
5. Druss BG, Hoff RA, Rosenbeck RA: Underuse of antidepressants in major depression: prevalence and correlates in a national sample of young adults. J Clin Psychiatry 2000; 61:234-237Crossref, Medline, Google Scholar
6. Parikh SV, Lesage AD, Kennedy SH, Goering PN: Depression in Ontario: under-treatment and factors related to antidepressant use. J Affect Disord 1999; 52:67-76Crossref, Medline, Google Scholar
7. Tylee A, Gastpar M, Lepine J-P, Mendlewicz J: DEPRES II: a patient survey of the symptoms, disability and current management of depression in the community. Int Clin Psychopharmacol 1999; 14:139-151Medline, Google Scholar
8. Arinen S, Häkkinen U, Klaukka T, Klavus J, Lehtonen R, Aro S: Health and the use of health services in Finland: main findings of the Finnish Health Care Survey 1995/96 and changes from 1987, in Official Statistics of Finland, 1998. Helsinki, STAKES, National Research and Development Centre for Welfare and Health, 1998 (http://www.stakes.fi/thty/terva/index.html)Google Scholar
9. Lindeman S, Hämäläinen J, Isometsä E, Kaprio J, Poikolainen K, Heikkinen M, Aro H: The 12-month prevalence and risk factors for major depressive episode: representative sample of 5993 adults. Acta Psychiatr Scand 2000; 102:178-184Crossref, Medline, Google Scholar
10. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods in Psychiatr Res 1998; 7:171-185Crossref, Google Scholar



