Shortened Duration of Untreated First Episode of Psychosis: Changes in Patient Characteristics at Treatment
Abstract
OBJECTIVE: This study examined whether duration of untreated psychosis can be shortened in patients with first episodes of DSM-IV schizophrenia spectrum disorders and whether shorted duration alters patient appearance at treatment. METHOD: Two study groups were ascertained in the same Norwegian health care sector: one from 1993–1994 with usual detection methods and one from 1997–1998 with early detection strategies that included education about psychosis. RESULTS: Patients with early detection had a shorter median duration of untreated psychosis by 21.5 weeks than patients with usual detection. The number with psychosis was greater in the early detection group; the number with schizophrenia was less. Early detection patients had more substance abuse and were younger, better adjusted premorbidly, and less ill. CONCLUSIONS: Early detection can shorten duration of untreated psychosis and help more patients when they are less severely ill. Given the devastation of psychosis, this is a significant treatment advance.
The duration of untreated psychosis in first episodes of schizophrenia spectrum disorders can be long and may correlate with poorer outcome (1). We examined whether duration of untreated psychosis can be reduced and whether this changes how such patients appear at treatment. We compared two groups with first episodes of schizophrenia spectrum disorders from the Rogaland, Norway, health care sector that were ascertained in 1993–1994 and 1997–1998. During 1997–1998 an early detection system was constructed by using special detection teams and educational campaigns about psychosis, all detailed elsewhere (2). The early detection teams were modeled after the early psychosis program created by McGorry and colleagues (3). In the present study, we compared the 1993–1994 group assessed with usual methods of detection and the 1997–1998 group assessed with methods for early detection of psychosis for duration of untreated psychosis and their symptoms at first treatment.
Method
Our 1993–1994 study (4) was aimed at determining the duration of untreated psychosis in a group of consecutively admitted patients with first episodes of DSM-III-R schizophrenia spectrum disorders from the central and southern sectors of Rogaland County, Norway (population=260,000). Patients meeting screening criteria for a first psychotic episode completed a diagnostic Structured Clinical Interview for DSM-III-R with a clinical researcher trained to reliability. Only one patient refused to participate. Psychosis onset was defined as the time point when patients scored 4 or more on at least one of the positive psychotic symptoms of the Positive and Negative Syndrome Scale (5). The symptom had to have lasted throughout the day for several days or occurred several times a week and could not have been limited to a few brief moments (DSM-III-R duration criteria). For brief psychosis or psychosis not otherwise specified, these symptoms had to have lasted for at least 1 day. The duration of untreated psychosis was the time between the onset of psychosis and initiation of adequate treatment as rated by research team consensus after consideration of all available information. Premorbid functioning was assessed with the Premorbid Adjustment Scale (6) and substance abuse with the Clinician Rating Scale (7). For this study, DSM-III-R diagnoses were converted to DSM-IV diagnoses by one of us (T.K.L.).
The group with early detection of psychosis consisted of consenting patients with a first episode of schizophrenia spectrum disorders, as per DSM-IV criteria, from the same catchment area and diagnosed with the same assessment instruments in 1997–1998. Written informed consent was obtained from all patients. Data analysis included two-tailed t tests for normally distributed data, Mann-Whitney U tests for skewed data, and chi-square or Fisher’s exact probability tests for categorical data.
Results
The group with usual detection of psychosis consisted of 43 patients, and the group with early detection comprised 66 patients. Male patients in the early detection group were significantly younger by 3.5 years than male patients in the usual-detection group (mean=24.0 years, SD=6.2; mean=27.5, SD=7.4, respectively) (t=2.1, df=65, p=0.04). There were no differences between the groups in gender distribution (usual detection: 65% male; early detection: 59% male), age at onset of psychosis (mean=26.3 years, SD=8.4; mean=25.2, SD=7.8), or marital status (single: 86%; 77%).
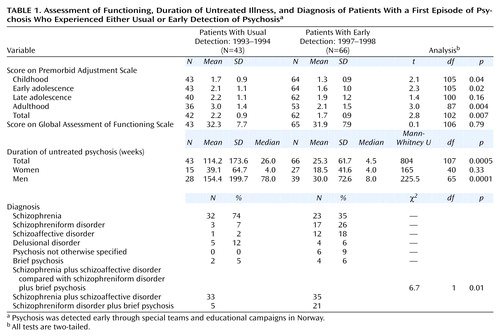
Table 1 compares data on premorbid functioning, global functioning, duration of untreated psychosis, and diagnosis. The early detection group’s premorbid adjustment scores were significantly better than those of the usual-detection group. We found no differences in Global Assessment of Functioning Scale scores, probably reflecting the effects of an active psychotic state at admission. The duration of untreated psychosis was significantly shorter for the women in the group with early detection, and there were more earlier forms of DSM-IV schizophrenia spectrum disorders than in the group with usual detection.
Positive and Negative Syndrome Scale symptom profiles at baseline showed clear differences between the groups. Mean values were less severe in the early detection group than in the usual-detection group: positive symptoms (usual detection: mean=21.4, SD=4.8; early detection: mean=17.6, SD=5.2) (t=3.9, df=106, p=0.0001), negative symptoms (mean=19.8, SD=6.8; mean=15.9, SD=7.5) (t=2.7, df=106, p=0.008), and general symptoms (mean=40.5, SD=88.9; mean=31.9, SD=10.7) (t=4.3, df=106, p=0.0001). There was more substance abuse (limited to drugs) in the early detection group (Clinician Rating Scale [7]: 1=abstinence, 2=use without impairment, 3=abuse, 4=dependence, 5=severe dependence) (usual detection: mean=1.3, SD=0.6; early detection: mean=1.9, SD=1.1) (t=–3.4, df=106, p=0.001).
A major difference with the 1997–1998 group was our ability to screen and treat patients with a first episode of psychosis in outpatient clinics. The 1997–1998 group, therefore, had more patients who were never hospitalized. Although we assumed that a few patients were treated without hospitalization in 1993–1994, we could not be sure, so we repeated all analyses for the hospitalized patients only and found the same differences between groups on all major variables (data available from Dr. Larsen).
Discussion
Our major finding is that a system for early detection of psychosis succeeded in shortening the duration of untreated psychosis in patients with first episodes of schizophrenia spectrum disorders. The early detection patients were more numerous, younger, and had better premorbid adjustment, less severe psychosis, and more frequent drug abuse. Overall, it appears that persons are identified as patients when symptom levels reach a certain threshold, and the system for early detection, by raising consciousness of that threshold, recruited psychotic patients who were experiencing earlier forms of schizophrenia spectrum disorders.
A major drawback of this study is its historical design, which could not control for major sources of population, measurement, and treatment variance between groups. We tried to minimize this by selecting patients from the same health care sector and groups with only 4 years’ difference between them, using the same assessment instruments, and restricting comparisons to baseline measures that were unaffected by treatment differences. A major strength of the study is the well-organized nationalized mental health care system of Rogaland County, Norway, which provides treatment to most, if not all, patients in the sector with serious mental disorders. As such, ascertainment of patients with psychosis provided a reasonable estimate of the population’s frequency of disorders over a given time period.
The overall reduction in the relative frequency of cases of schizophrenia in Rogaland in 1997–1998 is probably more apparent than real. Follow-up studies can show to what degree patients with earlier-appearing schizophrenia spectrum disorders, such as schizophreniform disorder, will later be diagnosed with schizophrenia spectrum disorders, such as schizophrenia. Early detection may also identify patients who are missed by usual detection systems because of better functioning and briefer symptom periods or because of drug abuse that masks psychotic symptoms. These are, nevertheless, patients with bona fide psychotic illnesses who may ultimately enter the treatment system later in more symptomatic and/or compromised states. We are confident that the early detection system neither identified false positive cases of illness nor falsely inflated the overall frequency of schizophrenia spectrum disorders. We feel the early detection system better reflected an approximation of all patients with psychosis in the county than the usual-detection system.
In conclusion, our study indicates that well-orchestrated educational campaigns and early detection teams are capable of bringing patients with first episodes of psychosis into treatment much earlier than otherwise. Psychosis, per definition, is an active disease that is unpredictable, dangerous, stigmatizing, and destructive to individual capacity and reputation. As such, we regard early detection as a significant addition to treatment delivery systems. We feel an important question has been answered; it is within our power to bring effective treatment earlier to our most needy psychiatric patients.
 |
Presented at the International Congress on Schizophrenia Research, Santa Fe, N. Mex., April 21–25, 1999. Received Aug. 24, 2000; revisions received Jan. 10 and April 23, 2001; accepted May 3, 2001. From the Department of Psychiatry, Yale University, New Haven, Conn.; Roskilde Psychiatric Hospital, Roskilde, Denmark; Rogaland Psychiatric Hospital, Ullevaal Hospital, and the Departments of Psychiatry and Behavioral Sciences, University of Oslo. Address reprint requests to Dr. Larsen, Rogaland Psychiatric Hospital, University of Oslo, Norway, P.O. Box 1163 Hillevåg, 4095 Stavanger, Norway; [email protected] (e-mail). Supported by the Norwegian National Research Council, the Norwegian Department of Health and Social Affairs, and the Oslo County Department of Health and Social Affairs (Drs. Vaglum, Johannessen, Larsen, Horneland, Friis, Melle, Opjordsmoen, Guldberg, and Moe). Also funded by the Stanley Foundation, the Regional Research Foundation for Roskilde County, Denmark, Lundbeck, Lilly, and Janssen Pharmaceuticals, and Roskilde County Psychiatric Hospital, Roskilde, Denmark (Drs. Simonsen and Haahr). Also supported by a National Alliance for Research on Schizophrenia and Depression Distinguished Investigator Award and NIMH grant MH-01654 (Dr. McGlashan) and a National Alliance for Research on Schizophrenia and Depression Young Investigator Award (Dr. Larsen).
1. McGlashan TH: Duration of untreated psychosis: marker or determinant of course? Biol Psychiatry 1999; 46:899-907Crossref, Medline, Google Scholar
2. Johannessen JO, McGlashan TH, Larsen TK, Horneland M, Joa I, Mardal S, Kvebæk R, Friis S, Melle I, Opjordsmoen S, Siemonsen E, Ulrik H, Vaglum P: Early detection strategies for untreated first-episode psychosis. Schizophr Res 2001; 51:39-46Crossref, Medline, Google Scholar
3. McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ: EPPIC: an evolving system of early detection and optimal management. Schizophr Bull 1996; 22:305-326Crossref, Medline, Google Scholar
4. Larsen TK, McGlashan TH, Johannessen JO, Vibe-Hansen L: First-episode schizophrenia, II: premorbid patterns by gender. Schizophr Bull 1996; 22:257-270Crossref, Medline, Google Scholar
5. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13:261-276Crossref, Medline, Google Scholar
6. Cannoon-Spoor HE, Potkin SG, Wyatt RJ: Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 1982; 8:470-484Crossref, Medline, Google Scholar
7. Drake RE, Osher FC, Noordsy DL, Hurlbut SC, Teague GB, Beaudett MS: Diagnosis of alcohol use disorders in schizophrenia. Schizophr Bull 1990; 16:57-67Crossref, Medline, Google Scholar



