Childhood Abuse and Lifetime Psychopathology in a Community Sample
Abstract
OBJECTIVE: The authors assessed lifetime psychopathology in a general population sample and compared the rates of five psychiatric disorder categories between those who reported a childhood history of either physical or sexual abuse and those who did not. METHOD: A modified version of the Composite International Diagnostic Interview and a self-completed questionnaire on child abuse were administered to a probability sample (N=7,016) of Ontario residents 15 to 64 years of age. RESULTS: Those reporting a history of childhood physical abuse had significantly higher lifetime rates of anxiety disorders, alcohol abuse/dependence, and antisocial behavior and were more likely to have one or more disorders than were those without such a history. Women, but not men, with a history of physical abuse had significantly higher lifetime rates of major depression and illicit drug abuse/dependence than did women with no such history. A history of childhood sexual abuse was also associated with higher rates of all disorders considered in women. In men, the prevalence of disorders tended to be higher among those who reported exposure to sexual abuse, but only the associations with alcohol abuse/dependence and the category of one or more disorders reached statistical significance. The relationship between a childhood history of physical abuse and lifetime psychopathology varied significantly by gender for all categories except for anxiety disorders. Although not statistically significant, a similar relationship was seen between childhood history of sexual abuse and lifetime psychopathology. CONCLUSIONS: A history of abuse in childhood increases the likelihood of lifetime psychopathology; this association appears stronger for women than men.
The relationship between a history of maltreatment during childhood and adult psychopathology has been well recognized in clinical populations (1, 2). Although fewer in number than clinical studies, several population-based community surveys have been carried out to examine the relationship between retrospective reports of child abuse and lifetime psychiatric morbidity in the community. The focus of these surveys has been primarily to assess the association between sexual abuse in childhood and adult emotional disorders, predominantly in women (3, 4). Previous studies (4–7), which include a meta-analysis comprising both clinical and community studies (4), indicate a relationship in women between exposure to sexual abuse during childhood and a wide range of psychiatric disorders, including depression, substance abuse, anxiety disorders, and suicidal behavior. A second meta-analysis that included both men and women concluded that there was a relationship between exposure to sexual abuse during childhood and both depression and general impairment in psychological adjustment (3). Fergusson et al. (8) assessed the relationship between a history of childhood sexual abuse and psychiatric morbidity in both male and female subjects, but the study consisted exclusively of 18-year-olds. One of the few surveys to include a representative sample of adult men was a supplement to the Los Angeles Epidemiologic Catchment Area (ECA) study (9, 10); sexual abuse during childhood was found to be a nonspecific correlate that increased vulnerability for a variety of emotional disorders, including major depressive episodes, anxiety disorders, and substance use disorders (9, 10).
Much less attention has been given to measuring the association between physical abuse and psychiatric morbidity. Duncan and colleagues (11) examined the relationship between a childhood history of serious physical assault and emotional impairment in a national sample of women. They found that those who reported such victimization experienced higher rates of depression, posttraumatic stress disorder (PTSD), and substance abuse. Similarly, Mullen and colleagues (12) found an association between childhood exposure to physical abuse and psychopathology in their community sample of women. One study considered childhood exposure to physical abuse in a group of subjects from upstate New York (13), but the focus was adolescents and young adults. One of the few surveys to explore the relationship between a childhood history of physical and sexual abuse in a representative sample of both men and women was the National Comorbidity Survey (14). Kessler and colleagues found that being “physically attacked” (the only act of physical abuse considered) was associated with a broad range of psychiatric disorders, including mood, anxiety, and addictive disorders.
This article presents findings from the Mental Health Supplement to the Ontario Health Survey about the relationship between a history of childhood physical and sexual abuse and five major psychiatric disorder categories. A previous article showed that a childhood history of physical or sexual abuse was common among Ontario residents (15). This report assesses the strength of reported childhood maltreatment as a correlate of psychiatric morbidity among those 15 years of age and older while controlling for age, sex, parental education, and current family income. The diagnostic categories considered in this article were those that had a sample size sufficient for examining their relationship with presence or absence of physical and sexual abuse.
Method
Sample
In 1990, the Ontario Ministry of Health sponsored the Ontario Health Survey, a comprehensive survey to gather information about the physical health of provincial residents. For the Mental Health Supplement, one respondent within a household participating in the Ontario Health Survey was randomly selected for participation; he or she was interviewed between November 1990 and March 1991. Excluded from the survey were homeless persons, people in institutions, foreign service personnel, First Nations people living on reserves, and persons residing in extremely remote locations. A detailed description of the survey design has been previously published (16). The data reported here are for the 15–64-year-old subjects in the sample, since respondents older than 64 were given a shortened diagnostic interview because of concern about interview burden (17).
Measures
The Composite International Diagnostic Interview (18) was used to determine the lifetime prevalence of psychiatric disorders. This measure is a standardized interviewer-administered questionnaire for the evaluation of mental disorders from DSM-III-R and ICD-10. The specific instrument used was the University of Michigan version of the Composite International Diagnostic Interview, which includes modifications to improve its usefulness in a general population survey (17, 19). For example, a diagnostic screening evaluation preceded the Composite International Diagnostic Interview so that respondents answered these questions before learning that a “no” response reduced the number of follow-up questions. Field trials of this interview have shown good interrater reliability, test-retest reliability, and validity for the majority of psychiatric diagnoses with the exception of psychosis (17, 20).
This article examines five major categories of psychiatric illness: 1) anxiety disorders (social phobia, simple phobia, agoraphobia, panic disorder, or generalized anxiety disorder); 2) major depressive disorder; 3) alcohol abuse/dependence; 4) illicit drug abuse/dependence; and 5) antisocial behavior (i.e., conduct disorder for those 15 to 17 years of age and antisocial personality disorder for those 18 to 64 years of age). Presence of a disorder from one or more of these five categories comprised the sixth category, “any psychiatric disorder.”
The Child Maltreatment History Self-Report (15), a self-administered questionnaire, was used to assess the childhood history of physical and sexual abuse. Respondents were asked about their experiences when they were “growing up” of physical and sexual abuse committed by an adult. The definition of physical abuse included six categories: being pushed, grabbed, or shoved; having something thrown at them; being kicked, bitten, or punched; getting hit with something; being choked, burned, or scalded; or being physically attacked in some other way. Slapping or spanking, even if it occurred often, was not included in the definition of physical abuse. Sexual abuse was defined as unwanted experiences committed by an adult that fell within four categories: repeated indecent exposure, sexual threats, touching of the child’s sex parts, and attempting sex with or sexually attacking the child. The definitions for both types of abuse include a broad range of exposures in terms of severity. The Child Maltreatment History Self-Report is described in detail in a separate publication (15). The physical abuse questions were based on several of the violence items included in the Conflict Tactics Scales (21), an instrument that has been shown to have acceptable psychometric properties. The questions dealing with sexual abuse were based on the instrument used for the National Population Survey (22), a Canadian survey of sexual abuse (often referred to as the “Badgley Report”). The bulk of the Mental Health Supplement to the Ontario Health Survey interview was conducted face-to-face. However, the Child Maltreatment History Self-Report was completed by respondents in private and returned to the interviewer in a sealed envelope.
The correlates considered included age, sex, and socioeconomic status. Socioeconomic status was measured by 1) education level (complete versus incomplete secondary school education) of the parent who provided the family’s major financial support during the respondent’s childhood and 2) current family income (above or below the poverty line as derived from income, urban/rural residence, and household size).
Statistical Procedures
Individual responses to the Mental Health Supplement to the Ontario Health Survey were weighted to obtain unbiased point estimates, based on the probability of selection in the sample (16). Weighting procedures were used to account for patterns of nonresponse. Poststratification weighting was applied to bring the age and sex distribution of the sample into agreement with that of the Ontario population in 1990 (16).
The statistical analyses were carried out by using Survey Data Analysis Software (SUDAAN for Windows, release 7.5.3, Research Triangle Institute, Research Triangle Park, N.C.), which makes statistical adjustments for survey design effects (23). Bivariate analyses compared respondents who reported a childhood history of physical abuse to those without a history of physical abuse; these analyses were repeated for childhood history of sexual abuse. Logistic regression models with forced entry of relevant variables were used to derive crude odds ratios and odds ratios adjusted for age, sex, parental education, and current family income as well as odds ratios for the interaction of childhood history of physical or sexual abuse and gender in predicting psychiatric morbidity.
It should be noted that for the separate analyses of childhood physical and sexual abuse, the group of respondents who reported exposure to abuse did not exclude those who had experienced both types of maltreatment. Similarly, the comparison group in each case was only free of the type of child abuse considered within each analysis; those who did not report a history of physical abuse may still have reported a history of sexual abuse and vice versa. This analysis was selected because despite the large size of the overall sample, eliminating those respondents with a history of physical abuse from the sexual abuse analyses would have resulted in insufficient power to detect between-group differences.
Results
Of the 14,758 households eligible for the Ontario Health Survey, 13,002 (88.1%) participated. Of those, 9,953 (76.5%) took part in the Mental Health Supplement for an overall response rate of 67.4%. Nonparticipation was primarily due to inability to contact the occupant, followed by unwillingness to participate. A detailed description of the sample is provided elsewhere (16). Of the 8,116 individuals 15 to 64 years of age, data were analyzed for 7,016 respondents after excluding those with missing information on the relevant variables. Briefly, of these remaining respondents, 47.6% (N=3,338) were male, 62.7% (N=4,399) reported being married or in a common law union, 61.7% (N=4,329) described their main activity as working, and 13.6% (N=954) indicated that their family income was below the poverty line.
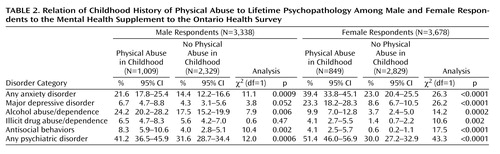
The age of the male (mean=36.1 years, 95% confidence interval [CI]=35.2–36.9) and female (mean=36.0 years, 95% CI=35.3–36.6) survey respondents was similar. Table 1 outlines the prevalence by gender of lifetime psychopathology, history of childhood physical and sexual abuse, and socioeconomic status. The lifetime prevalence of the five psychiatric disorder categories for male and female survey respondents with and without a history of physical abuse are summarized in Table 2; findings for sexual abuse are provided in Table 3.
For both male and female respondents, the likelihood of lifetime prevalence of the specified major psychiatric disorders was increased by a history of childhood physical or sexual abuse. Among female subjects, the association with childhood physical and sexual abuse was statistically significant for all disorders, including the sixth category of “any psychiatric disorder.” Two disorders did not show a statistically significant effect among male respondents with a childhood history of physical abuse compared to those without such a history: major depressive disorder and illicit drug abuse/dependence, although the former approached statistical significance. While men who reported childhood exposure to sexual abuse had higher rates of psychiatric disorder, only the association with alcohol abuse/dependence reached statistical significance.
Table 4 presents the crude and adjusted odds ratios from the logistic regression analyses. Adjusting for respondent age, sex, and socioeconomic status had little appreciable impact on the strength of association between exposure to abuse and psychiatric disorder. In every instance the strength of association (odds ratio) between a history of child abuse and psychiatric disorder was larger in magnitude for women than men. For all categories of psychiatric illness except for anxiety disorders, there was a significant interaction with gender for childhood history of both physical abuse and any abuse. Only in the prediction of lifetime anxiety disorders was there a significant interaction with gender for childhood history of sexual abuse, although the interaction approached statistical significance for major depressive disorder and antisocial behavior (Table 4).
Discussion
This article highlights three main findings from the Mental Health Supplement to the Ontario Health Survey: 1) a history of physical or sexual abuse during childhood is strongly associated with lifetime psychopathology; 2) physical abuse is at least as important a correlate for psychiatric morbidity as sexual abuse; and 3) the relationship between psychiatric illness and history of childhood maltreatment tends to be stronger for women than for men. This survey cannot provide information about cause and effect relationships. As other authors have emphasized, it may not be the history of abuse itself that leads to greater vulnerability for psychiatric illness but rather confounding social and familial factors associated with both the experience of child abuse and greater risk of disorder (8, 12). These include dysfunctional family environments (associated with both physical and sexual abuse) and poverty (associated with physical abuse) (24). (While the Mental Health Supplement to the Ontario Health Survey assessed parental education and current family income, it was not possible to assess childhood history of poverty.) A longitudinal study that uses nonabused siblings as control subjects and begins in early childhood before the onset of disorder is a study design that could address these issues.
The Mental Health Supplement to the Ontario Health Survey relied on retrospective reports to assess the prevalence of a childhood history of physical and sexual abuse. While some suggest that the presence of emotional impairment may influence memory of events, there is little scientific evidence to support the claim that recall of experiences in childhood is altered by psychiatric symptoms or disorder (25, 26).
The survey findings suggest that childhood physical and sexual abuse are nonspecific correlates of psychiatric illness; there does not appear to be a specific association between either of these subcategories of child maltreatment and one particular psychiatric disorder category. However, one of the most important findings of this study is that the association between a history of child abuse and psychopathology varies by gender. With the exception of anxiety disorders, the relationship between childhood exposure to physical abuse and psychopathology was stronger for women than for men. The relationship between childhood exposure to sexual abuse and psychopathology followed a similar pattern but did not achieve the same patterns of statistical significance because of limited power.
Since many community surveys that have collected information about child maltreatment and psychiatric morbidity have focused exclusively on women (27), few comparisons are possible. In the supplement to the Los Angeles ECA Study (9), relative to nonabused subjects, women with a history of childhood sexual abuse experienced higher lifetime rates of all psychiatric disorders except antisocial personality disorder, while abused men had higher rates of substance abuse/dependence. The authors hypothesized that gender differences could be due to the small number of men in the sample or to variations in circumstances of abuse.
Using data from the National Comorbidity Survey (28), Kessler and colleagues found, among a subsample of respondents who had been exposed to at least one trauma, that women had much higher odds of developing PTSD than men (odds ratio=6.13). Conversely, in a separate article (14), Kessler and colleagues concluded that there was no systematic sex difference in the associations between childhood adversities (which included such interpersonal traumas as being physically attacked and sexual molestation) and a range of psychiatric disorders (excluding PTSD). These DSM-III-R diagnoses included those examined in the Mental Health Supplement to the Ontario Health Survey.
It is possible that the nature and duration of the reported abuse are dissimilar for men and women. Cutler and Nolen-Hoeksema (29) suggested that women experience more severe forms of abuse than do men. In the Mental Health Supplement to the Ontario Health Survey, although female and male respondents reported similar rates of severe physical abuse in childhood (9.2% and 10.7%, respectively) (15), physical abuse was still a stronger predictor of psychiatric illness in women than in men. The survey’s definition of severe physical abuse took likelihood of injury and frequency into account but did not include duration, age at onset of abuse, or relationship with perpetrator, which are some of the factors considered in the sexual abuse literature (5).
A related issue is the overlap between reports of child physical and sexual abuse. Among female respondents who reported childhood physical abuse, 33% also had a history of sexual abuse, while the corresponding figure for male respondents was only 8%. In contrast, 56% of male and 56% of female respondents who reported childhood sexual abuse also gave a history of physical abuse. Perhaps differences in the degree of overlap between men and women led to differences in the association with psychiatric disorders. Unfortunately, the survey sample was not of sufficient size to examine this issue more closely.
Gender differences in reporting retrospective information about abuse in childhood may have contributed to this effect. An article by Widom and Morris (30) suggested that among individuals with a history of documented sexual abuse in childhood, far fewer men than women considered their early childhood experiences as sexual abuse.
It is well documented in the literature that both physical and sexual abuse are associated with a range of adverse circumstances (12). It may be that history of physical or sexual abuse is a marker for other adverse experiences in childhood that are more common among women than men. Since the Mental Health Supplement to the Ontario Health Survey involved retrospective collection of data, detailed information about factors such as family dysfunction or income level while growing up was not available.
Perhaps the experience of physical or sexual abuse in childhood affects women differently from men because of the biological and psychological mechanisms involved in the trauma. Studies examining the impact of child maltreatment suggest that dysfunction of the hypothalamic-pituitary-adrenal axis may contribute to the development of negative outcomes such as depressive symptoms following exposure to trauma (31, 32). However, samples to date have generally involved female subjects only (31) or too few male subjects (32) to examine the effect of gender. As for psychological mechanisms that may operate differently among men and women, Cutler and Nolen-Hoeksema (29) suggest that women may be more likely to blame themselves for the abuse or may have a type of affect regulation that increases their vulnerability to negative circumstances. These areas merit further investigation, since understanding differences in risk may assist in developing effective treatments.
Since the Mental Health Supplement to the Ontario Health Survey was a cross-sectional survey, we cannot draw any conclusions about the causal role of childhood maltreatment in the development of psychiatric disorders from these findings. Nevertheless, on the basis of this community survey of more than 7,000 residents of Ontario, both physical and sexual abuse appear to be important markers for a higher likelihood of a range of psychiatric disorders in both men and women.
 |
 |
 |
 |
Received July 7, 2000; revision received Feb. 6, 2001; accepted April 19, 2001. From the Canadian Centre for Studies of Children at Risk; the Department of Psychiatry, University of Toronto, Toronto; and the Department of Psychiatry, Harvard Medical School, Boston. Address reprint requests to Dr. MacMillan, Canadian Centre for Studies of Children at Risk, McMaster University, 1200 Main St. West, Patterson Bldg., Box 2000, Hamilton, Ontario, L8N 3Z5 Canada; [email protected] (e-mail). Supported in part by the Ontario Ministries of Health; Ontario Community and Social Services; the Ontario Mental Health Foundation; Wyeth-Ayerst Canada Inc. Canadian Institutes of Health Research (CIHR) Clinical Research Chair in Women’s Mental Health; a William T. Grant Faculty Scholar Award (Dr. MacMillan); and a CIHR Scientist Award (Dr. Boyle). The authors thank the Family Violence Research Seminar Group at the Family Research Laboratory, University of New Hampshire, for their comments on earlier drafts of this article.
1. McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, Ryden J, Derogatis LR, Bass EB: Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA 1997; 277:1362-1368Crossref, Medline, Google Scholar
2. Brown GR, Anderson B: Psychiatric morbidity in adult inpatients with childhood histories of sexual and physical abuse. Am J Psychiatry 1991; 148:55-61Link, Google Scholar
3. Jumper SA: A meta-analysis of the relationship of child sexual abuse to adult psychological adjustment. Child Abuse Negl 1995; 19:715-728Crossref, Medline, Google Scholar
4. Neumann DA, Houskamp BM, Pollack VE, Briere J: The long-term sequelae of childhood sexual abuse in women: a meta-analytic review. Child Maltreat 1996; 1:6-16Crossref, Google Scholar
5. Weiss EL, Longhurst JG, Mazure CM: Childhood sexual abuse as a risk factor for depression in women: psychosocial and neurobiological correlates. Am J Psychiatry 1999; 156:816-828Link, Google Scholar
6. Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA: Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry 2000; 57:953-959Crossref, Medline, Google Scholar
7. Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP: Childhood sexual abuse and mental health in adult life. Br J Psychiatry 1993; 163:721-732Crossref, Medline, Google Scholar
8. Fergusson DM, Horwood LJ, Lynskey MT: Childhood sexual abuse and psychiatric disorder in young adulthood, II: psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry 1996; 35:1365-1374Crossref, Medline, Google Scholar
9. Stein JA, Golding JM, Siegel JM, Burnam MA, Sorenson SB: Long-term psychological sequelae of child sexual abuse, in Lasting Effects of Child Sexual Abuse. Edited by Wyatt GE, Powell GJ. Newbury Park, Calif, Sage Publications, 1988, pp 135-154Google Scholar
10. Burnam MA, Stein JA, Golding JM, Siegel JM, Sorenson SB, Forsythe AB, Telles CA: Sexual assault and mental disorders in a community population. J Consult Clin Psychol 1988; 56:843-850Crossref, Medline, Google Scholar
11. Duncan RD, Saunders BE, Kilpatrick DG, Hanson RF, Resnick HS: Childhood physical assault as a risk factor for PTSD, depression, and substance abuse: findings from a national survey. Am J Orthopsychiatry 1996; 66:437-448Crossref, Medline, Google Scholar
12. Mullen PE, Martin JC, Romans SE, Herbison GP: The long-term impact of the physical, emotional, and sexual abuse of children: a community study. Child Abuse Negl 1996; 20:7-21Crossref, Medline, Google Scholar
13. Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP: Childhood maltreatment increases risk for personality disorders during early adulthood. Arch Gen Psychiatry 1999; 56:600-606Crossref, Medline, Google Scholar
14. Kessler RC, Davis CG, Kendler KS: Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 1997; 27:1101-1119Crossref, Medline, Google Scholar
15. MacMillan HL, Fleming JE, Trocmé N, Boyle MH, Wong M, Racine YA, Beardslee WR, Offord DR: Prevalence of child physical and sexual abuse in the community: results from the Ontario Health Supplement. JAMA 1997; 278:131-135Crossref, Medline, Google Scholar
16. Boyle MH, Offord DR, Campbell D, Catlin G, Goering P, Lin E, Racine YA: Mental Health Supplement to the Ontario Health Survey: methodology: Can J Psychiatry 1996; 41:549-558Google Scholar
17. Offord DR, Boyle MH, Campbell D, Goering P, Lin E, Wong M, Racine YA: One-year prevalence of psychiatric disorder in Ontarians 15 to 64 years of age. Can J Psychiatry 1996; 41:559-563Crossref, Medline, Google Scholar
18. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
19. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
20. Wittchen HU: Reliability and validity studies of the WHO—Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 1994; 28:57-84Crossref, Medline, Google Scholar
21. Straus MA: The Conflict Tactics Scales and its critics: an evaluation and new data on validity and reliability, in Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Edited by Straus MA, Gelles RJ. New Brunswick, NJ, Transaction, 1990, pp 49-73Google Scholar
22. Badgley RF, Allard HA, McCormick N, Proudfoot PM, Fortin D, Ogilvie D, Rae-Grant Q, Gélinas P-M, Pépin L, Sutherland S: Sexual Offences Against Children: Catalogue Number J2-50/1984E. Ottawa, Department of Supply and Services, 1984Google Scholar
23. Levy PS, Lemeshow S: Sampling of Populations: Methods and Applications. New York, John Wiley & Sons, 1999Google Scholar
24. MacMillan HL, Niec AC, Offord DR: Child physical abuse: risk indicators and prevention, in Recent Advances in Pediatrics, vol 14. Edited by David TJ. Edinburgh, Churchill Livingstone, 1995, pp 53-68Google Scholar
25. Brewin CR, Andrews B, Gotlib IH: Psychopathology and early experience: a reappraisal of retrospective reports. Psychol Bull 1993; 113:82-98Crossref, Medline, Google Scholar
26. Robins L, Schoenberg SP, Holmes SJ, Ratcliff KS, Benham A, Works J: Early home environment and retrospective recall: a test for concordance between siblings with and without psychiatric disorders. Am J Orthopsychiatry 1985; 55:27-41Crossref, Medline, Google Scholar
27. Finkelhor D: Current information on the scope and nature of child sexual abuse. Future Child 1994; 4:31-53Crossref, Medline, Google Scholar
28. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048-1060Crossref, Medline, Google Scholar
29. Cutler SE, Nolen-Hoeksema S: Accounting for sex differences in depression through female victimization: childhood sexual abuse. Sex Roles 1991; 24:425-438Crossref, Google Scholar
30. Widom CS, Morris S: Accuracy of adult recollections of childhood victimization, part 2: childhood sexual abuse. Psychol Assess 1997; 9:34-46Crossref, Google Scholar
31. De Bellis MD, Chrousos GP, Dorn LD, Burke L, Helmers K, Kling MA, Trickett PK, Putnam FW: Hypothalamic-pituitary-adrenal axis dysregulation in sexually abused girls. J Clin Endocrinol Metab 1994; 78:249-255Medline, Google Scholar
32. Kaufman J, Birmaher B, Perel J, Dahl RE, Moreci P, Nelson B, Wells W, Ryan ND: The corticotropin-releasing hormone challenge in depressed abused, depressed nonabused, and normal control children. Biol Psychiatry 1997; 42:669-679Crossref, Medline, Google Scholar



