Association of the TaqI A Polymorphism of the Dopamine D2 Receptor Gene With Predisposition to Neuroleptic Malignant Syndrome
Abstract
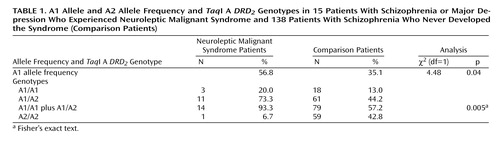
OBJECTIVE: The pathophysiology of neuroleptic malignant syndrome is mainly explained by a central hypodopaminergic state. The familial occurrence of neuroleptic malignant syndrome suggests the involvement of a genetic mechanism in the predisposition to the syndrome. Therefore, the authors examined the association between the TaqI A polymorphism of the dopamine D2 receptor gene (DRD2), which alters DRD2 density and function, and the development of neuroleptic malignant syndrome. METHOD: The subjects were 15 psychiatric patients who had developed neuroleptic malignant syndrome (12 patients with schizophrenia and three with major depression) and 138 patients with schizophrenia who had never developed neuroleptic malignant syndrome. The TaqI A genotypes, A1 and A2 alleles, were determined by the polymerase chain reaction method. RESULTS: The frequency of the A1 allele was significantly higher in the patients who had developed neuroleptic malignant syndrome (56.8%) than in the patients who had not (35.1%). The proportion of the A1 carrier was significantly higher in the patients with neuroleptic malignant syndrome (14 [93.3%] of 15 patients) than in those without the syndrome (79 [57.2%] of 138 patients). CONCLUSIONS: These findings suggest that the TaqI A DRD2 polymorphism is associated with the predisposition to neuroleptic malignant syndrome.
Neuroleptic malignant syndrome is a rare but potentially fatal complication of neuroleptic drugs (1). The syndrome is characterized by hyperpyrexia, extrapyramidal symptoms, catatonic symptoms, and autonomic disturbances. The pathophysiology of neuroleptic malignant syndrome has been explained mainly by a central hypodopaminergic state (2–4), although other neurotransmitters such as serotonin may be associated with it (5).
There have been several reports on the familial occurrence of neuroleptic malignant syndrome (2, 6, 7), suggesting that a genetic mechanism is involved in the predisposition to this syndrome. Therefore, we analyzed the coding sequences of the dopamine D2 receptor gene (DRD2) in 12 patients who had experienced neuroleptic malignant syndrome (8). Although one patient had a rare heterozygote for the Pro310Ser variant in exon 7, the allele frequency was not significantly different in these patients from that in a control group.
The human DRD2 gene contains a TaqI restriction fragment length polymorphism, creating the A1 and A2 alleles (9). Studies using postmortem brains showed that the subjects with one or two A1 alleles had lower DRD2 density in the striatum (10) and caudate nuclei (11) than those without this allele, and these results have been confirmed in vivo with positron emission tomography (12). Functionally, the A1 allele has been associated with diminished dopaminergic activity and reduced glucose metabolism in brain regions with abundant dopamine receptors (11). These findings suggest the possibility that carriers of A1 show higher DRD2 blockade by neuroleptic drugs and are more prone to develop neuroleptic malignant syndrome than noncarriers.
The goal of the present study was to examine the association between the TaqI A DRD2 polymorphism and the development of neuroleptic malignant syndrome.
Method
The subjects were 15 Japanese psychiatric patients who had developed neuroleptic malignant syndrome defined according to the criteria of Pope et al. (13). Six of the patients were men and nine were women; their mean age was 42.5 years (SD=14.3). Twelve of the patients were suffering from schizophrenia and three from major depression diagnosed according to DSM-III-R. The comparison subjects were 138 Japanese patients with schizophrenia who had never developed neuroleptic malignant syndrome. Fifty-five of these patients were men and 83 were women; their mean age was 43.6 (SD=12.5).
The mean dose of neuroleptic in haloperidol equivalents and the duration of neuroleptic exposure were 10.4 mg/day (SD=6.7) and 127.7 days (SD=195.9), respectively, for the patients who had experienced neuroleptic malignant syndrome and 11.4 mg/day (SD=1.4) and 470.0 days (SD=645.4), respectively, for the comparison patients. This study was approved by the Ethics Committee of Hirosaki University Hospital. After complete description of the study to the subjects, written informed consent to participate was obtained from the patients and their families.
Ten ml of blood was obtained from each patient, and DNA was isolated from peripheral leukocytes by a guanidinium isothiocyanate method. The TaqI A DRD2 genotypes, the A1 and A2 alleles, were determined by the polymerase chain reaction method (14).
The statistical analyses were performed with chi-square test with Yates’s correction or Fisher’s exact test (if the number of subjects in the cell was smaller than five) for categorical variables (e.g., gender distribution, allele frequency, and genotype distribution) and Student’s t test for continuous variables (e.g., age and neuroleptic dose). A two-tailed p value of 0.05 or less was regarded as statistically significant. All analyses were performed by using SPSS 8.0.1J for Windows (SPSS Japan, Inc., Tokyo).
Results
There were no significant differences in age (t=0.34, df=151, p=0.74), gender distribution (χ2=0.000, df=1, p=1.00), and neuroleptic dose (t=0.63, df=14.129, p=0.54) between the neuroleptic malignant syndrome patients and the comparison patients.
The A1 allele frequency was significantly higher in the neuroleptic malignant syndrome patients than in the comparison patients (Table 1). The proportion of the A1 carrier was significantly higher in the neuroleptic malignant syndrome group than in the comparison group (Table 1). The odds ratio of neuroleptic malignant syndrome occurrence in the A1 carriers compared with the noncarriers was 10.5 (95% confidence interval=1.34– 81.76).
Discussion
Several studies (2–4) have suggested that a central hypodopaminergic state is a basic part of the underlying pathophysiology in neuroleptic malignant syndrome. More specifically, Jauss et al. (15), using single photon emission computed tomography, found a close association between the extent of DRD2 blockade by neuroleptic drugs and the development of neuroleptic malignant syndrome. In a patient with schizophrenia, the DRD2 blockade in the basal ganglia was complete during a neuroleptic malignant syndrome episode but unremarkable when the patient was free from the syndrome.
We recently reported that patients with schizophrenia who had the A1 allele showed greater prolactin response (16) and better therapeutic response (17) to nemonapride, a selective dopamine antagonist, than patients without this allele. These findings indicate that A1 carriers show higher DRD2 blockade by neuroleptic drugs than noncarriers.
In the present study, the A1 allele frequency was significantly higher in the patients who had experienced neuroleptic malignant syndrome than in patients who had not had the syndrome. Surprisingly, 93.3% of the neuroleptic malignant syndrome patients carried one or two A1 alleles, and this proportion was significantly higher than it was among the comparison patients. The risk of developing neuroleptic malignant syndrome was estimated to be 10.5 times higher in the A1 carriers than in the noncarriers. These results suggest that the A1 allele is associated with the predisposition to neuroleptic malignant syndrome. It is likely that because of lower DRD2 density (10–12), the A1 carriers have a higher chance than the noncarriers of showing excessive DRD2 blockade by neuroleptic drugs, leading to the development of neuroleptic malignant syndrome.
It is still unclear how the TaqI A polymorphism, which is located 10 kb into the 3′ untranslated region of the DRD2 gene, affects the expression of this gene (9). Most probably, this polymorphism reflects linkage disequilibrium with some unidentified mutations that alter DRD2 density (9). Therefore, in the event of clarification of those gene mutations, their relationships with the development of neuroleptic malignant syndrome should be examined.
A possible clinical implication of our findings are that A1 carriers could receive potentially lower doses of neuroleptics if this polymorphism were used in a pharmacogenomic screening procedure. To confirm these findings, further replicated studies should be performed with larger numbers of subjects.
 |
Received Nov. 6, 2000; revision received March 29, 2001; accepted April 25, 2001. From the Department of Neuropsychiatry, Hirosaki University School of Medicine; the Department of Neuropsychiatry, Yamagata University School of Medicine; Yamagata, Japan; the Department of Neuropsychiatry, Ehime University School of Medicine, Matsuyama, Japan; and Kuroda Hospital, Japan. Address reprint requests to Dr. Kondo, Department of Neuropsychiatry, Hirosaki University School of Medicine, Hirosaki 036-8562, Japan; [email protected] (e-mail).
1. Kellam AMP: The (frequently) neuroleptic (potentially) malignant syndrome. Br J Psychiatry 1990; 157:169-173Crossref, Medline, Google Scholar
2. Otani K, Horiuchi M, Kondo T, Kaneko S, Fukushima Y: Is the predisposition to neuroleptic malignant syndrome genetically transmitted? Br J Psychiatry 1991; 158:850-853Crossref, Medline, Google Scholar
3. Otani K, Mihara K, Okada M, Kaneko S, Fukushima Y: Crossover reaction between haloperidol and amoxapine for NMS (letter). Br J Psychiatry 1991; 159:889Crossref, Medline, Google Scholar
4. Otani K, Mihara K, Kondo T, Okada M, Kaneko S, Fukushima Y: Treatment of neuroleptic malignant syndrome with levodopa. Hum Psychopharmacol 1992; 7:217-221Crossref, Google Scholar
5. Young C: A case of neuroleptic malignant syndrome and serotonin disturbance. J Clin Psychopharmacol 1997; 17:65-66Crossref, Medline, Google Scholar
6. Deuschl G, Oepen G, Hermle L, Kindt H: Neuroleptic malignant syndrome: observations on altered consciousness. Pharmacopsychiatry 1987; 20:168-170Crossref, Medline, Google Scholar
7. Hosty G: Neuroleptic malignant syndrome in two sisters. Irish J Psychol Med 1992; 9:122-123Crossref, Google Scholar
8. Ram A, Cao Q, Keck PE, Pope HG, Otani K, Addonizio G, McElroy SL, Kaneko S, Redlichova M, Gershon ES, Gejman PV: Structural change in dopamine D2 receptor gene in a patient with neuroleptic malignant syndrome. Am J Med Genet 1995; 60:228-230Crossref, Medline, Google Scholar
9. Grandy DK, Litt M, Allen L, Bunzow JR, Marchionni M, Makam H, Reed L, Magenis RE, Civelli O: The human dopamine D2 receptor gene is located on chromosome 11 at q22-q23 and identifies a TaqI RFLP. Am J Hum Genet 1989; 45:778-785Medline, Google Scholar
10. Thompson J, Thomas N, Singleton A, Piggott M, Lloyd S, Perry EK, Morris CM, Perry RH, Ferrier IN, Court JA: D2 dopamine receptor gene (DRD2) TaqI A polymorphism: reduced dopamine D2 receptor binding in the human striatum associated with the A1 allele. Pharmacogenetics 1997; 7:479-784Crossref, Medline, Google Scholar
11. Noble EP: The D2 dopamine receptor gene: a review of association studies in alcoholism and phenotypes. Alcohol 1998; 16:33-45Crossref, Medline, Google Scholar
12. Jönsson EG, Nöthen MM, Grünhage F, Farde L, Nakashima Y, Propping P, Sedvall GC: Polymorphisms in the dopamine D2 receptor gene and their relationships to striatal dopamine receptor density of healthy volunteers. Mol Psychiatry 1999; 4:290-296Crossref, Medline, Google Scholar
13. Pope HG Jr, Keck PE Jr, McElroy SL: Frequency and presentation of neuroleptic malignant syndrome in a large psychiatric hospital. Am J Psychiatry 1986; 143:1227-1233Link, Google Scholar
14. Grandy DK, Zhang Y, Civelli O: PCR detection of the TaqA RFLP at the DRD2 locus (abstract). Hum Mol Genet 1993; 2:2197Crossref, Medline, Google Scholar
15. Jauss M, Krack P, Franz M, Klett R, Bauer R, Gallhofer B, Dorndorf W: Imaging of dopamine receptors with [123I]iodobenzamide single-photon emission-computed tomography in neuroleptic malignant syndrome. Mov Disord 1996; 11:726-728Crossref, Medline, Google Scholar
16. Mihara K, Kondo T, Suzuki A, Yasui N, Nagashima U, Ono S, Otani K, Kaneko S: Prolactin response to nemonapride, a selective antagonist for D2 like dopamine receptors, in schizophrenic patients in relation to Taq1A polymorphism of DRD2 gene. Psychopharmacology (Berl) 2000; 149:246-250Crossref, Medline, Google Scholar
17. Suzuki A, Mihara K, Kondo T, Tanaka O, Nagashima U, Otani K, Kaneko S: The relationship between dopamine D2 receptor polymorphism at the Taq1 A locus and therapeutic response to nemonapride, a selective dopamine antagonist, in schizophrenic patients. Pharmacogenetics 2000; 10:335-341Crossref, Medline, Google Scholar



