Is Age at Symptom Onset Associated With Severity of Memory Impairment in Adults With Obsessive-Compulsive Disorder?
Abstract
OBJECTIVE: Age at onset is a potentially important marker for neurobiological features of obsessive-compulsive disorder (OCD). This study examined the relationship between age at symptom onset and memory impairment in adults with OCD. METHOD: The authors used the Rey-Osterrieth Complex Figure Test and the California Verbal Learning Test to compare memory functioning of 37 adult OCD patients with self-reported childhood onset of symptoms (onset at less than 18 years of age) with that of 31 patients with adult-onset symptoms. RESULTS: No differences were found between the two groups on any of the verbal and nonverbal memory measures. CONCLUSIONS: Self-reported age at symptom onset is not associated with memory performance in adult patients with OCD according to tests previously found to be sensitive to frontal-striatal system dysfunction and impairment in OCD. Such dysfunction appears to be a consistent feature of OCD in adults, regardless of age at initial symptom onset.
Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts and repetitive, ritualistic behaviors that lead to substantial impairments in functioning. Several lines of evidence link OCD with distinct patterns of brain dysfunction and cognitive impairment. Evidence for frontal-striatal models of OCD comes from elevated rates of OCD in individuals with basal ganglia disorders and from functional neuroimaging studies indicating hyperfunction in the orbitofrontal and anterior cingulate cortex as well as the caudate nuclei. Neuropsychological investigations have also linked OCD with specific patterns of cognitive impairment. In three recent investigations (1–3), subjects with OCD were found to have impairments in verbal and nonverbal episodic memory; these impairments were related to difficulties in using efficient learning strategies.
Incidence rates of OCD show a bimodal distribution, with one peak around age 10 and another during young adulthood (4). These two profiles of onset may be associated with different subtypes of the disorder. For example, juvenile-onset OCD can be distinguished from adult-onset OCD by stronger familial loading, male predominance, and higher rates of tics and neurological symptoms (4). Despite the demonstrated relevance of age at onset, its effect on neuropsychological functioning is unclear. Although Behar et al. (5) reported that children with OCD exhibited deficits on some neuropsychological measures of executive function, more recent studies (6) have not found differences between children with and without OCD. The present study examined the association between age at symptom onset and episodic memory impairment in adults with OCD.
Method
Study participants were 68 adult outpatients with OCD. After complete description of the study to the subjects, written informed consent was obtained from all who participated. Each subject completed a neuropsychological test battery that included the Rey-Osterrieth Complex Figure Test (7) and the California Verbal Learning Test (8). This study used the combined study groups from three previous neuropsychological investigations of OCD (1–3). Detailed descriptions of the administrative and scoring procedures for the Rey-Osterrieth Complex Figure Test and California Verbal Learning Test are provided in these earlier reports. Briefly, the Rey-Osterrieth Complex Figure Test provides a measure of construction ability and nonverbal recall, and the California Verbal Learning Test assesses verbal organization and memory.
Age at symptom onset was determined during a structured diagnostic interview by asking patients to recall the initial onset of their obsessions or compulsions. For 28 patients, age at symptom onset was also obtained during the first treatment visit, several weeks after the interview. All but one of the participants reported the same age at symptom onset during both interviews, suggesting high reliability of recall.
Thirty-seven patients were classified as having child-onset OCD (before age 18), and 31 were classified as having adult-onset OCD (age 18 and older). The mean age at symptom onset for the child-onset patients was 10.3 (SD=3.3, median=10, range=5–17), and the mean age at symptom onset for the adult-onset patients was 24.7 (SD=6.2, median=24, range=18–50). Nineteen (51%) of the child-onset and 17 (55%) of the adult-onset participants were women.
There were no differences between the two groups in current age, estimated verbal intelligence (vocabulary subtests of the WAIS-R or Shipley Institute of Living Scale [9], converted into z scores), number of years of education, proportion of patients receiving medication treatment, total number of comorbid conditions, frequency of specific comorbid disorders, or Yale-Brown Obsessive Compulsive Scale (10) scores (for the child-onset patients, mean=20.3, SD=5.3; for the adult-onset patients, mean=22.0, SD=5.8). The child-onset group reported significantly lower levels of depression on the Beck Depression Inventory (mean=11.7, SD=7.2) than the adult-onset group (mean=16.4, SD=9.0) (F=5.49, df=1, 63, p=0.02).
Results
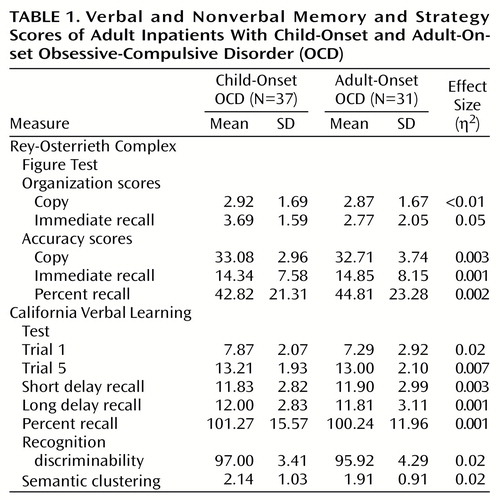
We examined Rey-Osterrieth Complex Figure Test and California Verbal Learning Test organization strategy and accuracy scores using mixed-model analysis of variance (ANOVA) with one between-subjects factor (group) and one within-subjects factor (condition). Condition refers to copy and immediate recall for Rey-Osterrieth Complex Figure Test organization and accuracy scores, and to trial 1, trial 5, short delay trial, and long delay trial for the California Verbal Learning Test. Mean scores on the Rey-Osterrieth Complex Figure Test and California Verbal Learning Test for the child-onset and adult-onset groups are presented in Table 1.
Analyses yielded no significant interactions or main effects of group for accuracy and organization scores on the Rey-Osterrieth Complex Figure Test and the California Verbal Learning Test. Multiple one-way ANOVAs also indicated no significant effects of group for the other Rey-Osterrieth Complex Figure Test and California Verbal Learning Test variables (i.e., Rey-Osterrieth Complex Figure Test accuracy percent recall and California Verbal Learning Test percent recall, recognition discriminability, and semantic clustering). Thus, both groups showed similar learning rates, recall, and strategy scores on both tests.
Significant within-subjects main effects for condition were found for Rey-Osterrieth Complex Figure Test accuracy scores (F=439.23, df=1, 66, p<0.001) and the California Verbal Learning Test scores (F=102.43, df=3, 44, p<0.001).
Because the study groups differed in depression levels, we reanalyzed the data using Beck Depression Inventory scores as a covariate. Results were identical to those without this covariate: no significant interactions were found for group by condition, and no main effects were found for group. As a further precautionary step, we examined the distribution of ages at symptom onset for the entire study group and found a trimodal distribution, with peaks at ages 8–10, 15–18, and 24–25. Based on this characteristic of our distribution, we ran all analyses again using a three-group design, and all findings remained nonsignificant (p>0.13). Finally, we correlated age at symptom onset as a continuous measure with our dependent variables; again, all correlations were nonsignificant.
Discussion
Adult patients with early and later onset of OCD symptoms did not differ on any of the measures of verbal and nonverbal strategic memory. It is noteworthy that these same patients were impaired on these measures when compared with matched healthy subjects and published norms (1–3). Our current results, with measures previously shown to be sensitive to frontal-striatal dysfunction, indicate that age at symptom onset is not a marker for differential memory impairment in adults with OCD. Likewise, because the duration of the disorder is linked with age at symptom onset (the two groups had different mean ages at onset but the same mean age at assessment), our findings speak against disease duration as a determinant of memory impairment.
The current study has some potential limitations. First, age at symptom onset was ascertained on the basis of retrospective self-report. Although participants were consistent in their reports of age at symptom onset, we cannot verify that their recall was accurate. Statistical power and the possibility of type II error are also potential concerns in any study reporting negative results. Nonetheless, all between-group effect sizes were uniformly small. Our results are further strengthened by their consistency with previous studies of children with OCD, which have not found neuropsychological impairment or brain structural volume to be correlated with age at symptom onset or illness duration (6, 11). Our results are also limited to memory and do not preclude that age at symptom onset is a marker for other important cognitive or clinical characteristics of OCD.
Previous work has shown that differences in brain morphology exist in both children and adults with OCD, but cognitive impairment has not been consistently detected in children with the disorder (5, 6). Our group has hypothesized that cognitive deficits may emerge during development in a manner that parallels normal frontal-striatal system maturation (11). Our results cannot address when strategic memory deficits may emerge, but they suggest that memory deficits are a reliable feature of OCD in adults, regardless of age at symptom onset. Longitudinal studies are needed to clarify the relationship between symptom onset and frontal-striatal dysfunction over the course of development.
 |
Received Feb. 4, 2000; revision received July 5, 2000; accepted July 28, 2000. From the Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston. Address reprint requests to Dr. Savage, Cognitive Neuroscience Group, Department of Psychiatry, 149-9102, Massachusetts General Hospital, Bldg. 149, 13th St., Charlestown, MA 02129-2060; [email protected] (e-mail). Supported by NIH grant MH-01230 and the Massachusetts General Hospital David Judah Research Fund. The authors thank Dr. David Shera of the Massachusetts General Hospital Biostatistics Unit for statistical consultation.
1. Savage CR, Baer L, Keuthen NJ, Brown HD, Rauch SL, Jenike MA: Organizational strategies mediate nonverbal memory impairment in obsessive-compulsive disorder. Biol Psychiatry 1999; 45:905–916Crossref, Medline, Google Scholar
2. Savage CR, Deckersbach T, Wilhelm S, Rauch SL, Baer L, Reid T, Jenike MA: Strategic processing and episodic memory impairment in obsessive-compulsive disorder. Neuropsychology 2000; 14:141–151Crossref, Medline, Google Scholar
3. Deckersbach T, Otto MW, Savage CR, Baer L, Jenike MA: The relationship between semantic organization and memory in obsessive-compulsive disorder. Psychother Psychosom 2000; 69:101–107Crossref, Medline, Google Scholar
4. Geller D, Biederman J, Jones J, Park K, Schwartz S, Shapiro S, Coffey B: Is juvenile obsessive-compulsive disorder a developmental subtype of the disorder? a review of the pediatric literature. J Am Acad Child Adolesc Psychiatry 1998; 37:420–427Crossref, Medline, Google Scholar
5. Behar D, Rapoport JL, Berg CJ, Denckla MB, Mann L, Cox C, Fedio P, Zahn T, Wolfman MG: Computerized tomography and neuropsychological test measures in adolescents with obsessive-compulsive disorder. Am J Psychiatry 1984; 141:363–369Link, Google Scholar
6. Beers SR, Rosenberg DR, Dick EL, Williams T, O’Hearn KM, Birmaher B, Ryan CM: Neuropsychological study of frontal lobe function in psychotropic-naive children with obsessive-compulsive disorder. Am J Psychiatry 1999; 156:777–779Abstract, Google Scholar
7. Osterrieth PA: Le test de copie d’une figure complex: contribution à l’étude de la perception et de la memoire. Arch Psychol 1944; 30:286–350Google Scholar
8. Delis DC, Kramer JH, Kaplan E, Ober BA: The California Verbal Learning Test Manual. New York, Psychological Corp, 1987Google Scholar
9. Shipley Institute of Living Scale. Los Angeles, Western Psychological Services, 1991Google Scholar
10. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006–1011Google Scholar
11. Savage CR, Rauch SL: Cognitive deficits in obsessive-compulsive disorder (letter). Am J Psychiatry 2000; 158:1182Link, Google Scholar



