Stressful Life Events and Previous Episodes in the Etiology of Major Depression in Women: An Evaluation of the “Kindling” Hypothesis
Abstract
OBJECTIVE: Although previous evidence has suggested that the etiologic role of stressful life events in major depression is reduced in recurrent versus first-onset cases, this question deserves reexamination because of potential methodological limitations of the previous studies. METHOD: Members of female-female twin pairs from a population-based registry (N=2,395), who were interviewed four times over a period of 9 years, formed a study group that contained 97,515 person-months and 1,380 onsets of major depression. Discrete-time survival, proportional hazards model, and piece-wise regression analyses were used to examine the interaction between life event exposure and number of previous depressive episodes in the prediction of episodes of major depression. RESULTS: For those with zero to nine previous depressive episodes, the depressogenic effect of stressful life events declined substantially with increasing episode number. However, the association between stressful life events and major depression was not substantially influenced by additional episodes. This pattern of results was robust to the addition of indices of event severity, measures of genetic risk, and restriction to independent stressful life events. The same pattern was also seen upon examining within-person changes in number of episodes. CONCLUSIONS: The association between previous number of depressive episodes and the pathogenic impact of stressful life events on major depression is likely causal and biphasic. Through approximately nine episodes, the association between stressful life event exposure and risk of major depression progressively declines but is largely unchanged with further episodes. These results are consistent with the kindling hypothesis but suggest a threshold at which the mind/brain is no longer additionally sensitized to the depressive state.
Major depression is a recurrent disorder of complex etiology. While both short-term environmental adversities such as stressful life events (1) and long-term diatheses such as genetic risk factors (2–4) are important causal factors in major depression (5), we know little about how these factors act over time. A leading hypothesis, first articulated by Kraepelin (6), is that psychosocial stressors play a greater role in the initial than in subsequent episodes of depressive disorders. Over the course of illness, the onset of depressive episodes may become increasingly autonomous and less related to environmental adversities. More recently, this pattern has been hypothesized to result from a sensitization process to the state of depression (7). Analogous to animal electrophysiologic models, this has been termed “the kindling hypothesis.” This hypothesis can also be expressed in mental language (8):
Vulnerability to depressive relapse/recurrence is determined by the increased risk of particular negative patterns of information processing…increased reliance on these patterns of processing makes it easier for their future activation to be achieved on the basis of increasingly minimal cues.
These models predict that with recurrent episodes of major depression, the role of environmental stressors will progressively diminish. We know of seven English-language studies that have examined this question (9–15). All found that the proportion of individuals for whom stressful life events preceded their current episode of major depression was greater in those with a first versus recurrent episode.
However, these studies need to be interpreted in the context of five methodological issues. First, they all studied clinical samples, thereby introducing the possible confounding effect of help-seeking behavior. For example, a bias might arise if individuals with recurrent versus first episodes of depression were more willing to present for treatment in the absence of a major life stressor. Second, these studies all compared the proportion of affected individuals who reported a major stressful life event that preceded their onset of major depression or the average number of individual events. This approach is valid only if there are no changes in the base rate of stressful life events with repeated episodes of major depression, a questionable assumption. In statistical terms, the kindling hypothesis may be more appropriately evaluated as an interaction between the number of previous depressive episodes and stressful life events in the prediction of risk for an onset of major depression. Third, most studies divided their sample into only two groups (usually one versus two or more episodes [9, 10, 12, 13, 15]), although two studies examined three (11) and five groups (14), respectively. None had a sufficient sample size to explore the “dose-response curve” of number of previous depressive episodes and depressogenic effect of stressful life events. For example, does the impact of stressful life events on risk for major depression decline linearly with increasing number of previous depressive episodes or does the “kindling effect” maximize out at some number of previous depressive episodes? Fourth, stressful life events vary both in their depressogenic potential and their independence of the respondent’s behavior (16). An analysis of the relationship among previous depressive episodes, stressful life events, and risk for major depression should consider both the severity and independence of stressful life events. Fifth, these studies were all cross-sectional, comparing different patients in their first versus recurrent episodes. These studies cannot therefore determine whether the difference in the association between stressful life events and major depression in those with no versus multiple previous episodes is due to an effect of previous depressive episodes or to stable individual differences in event sensitivity in those with low versus high risk for major depression. Since those with recurrent major depression have a higher familial liability to illness than those with single episodes (3, 17–21), this difference might be mediated genetically. Therefore, one approach to this problem would be to control for interindividual differences in the level of familial risk to major depression. The most powerful approach, however, would be to follow individuals over time and examine whether, within individuals, the magnitude of the association between stressful life events and major depression changes as they accumulate more episodes of depressive illness.
In this study, we reexamine, addressing these methodological issues, the relationship among episode onset for major depression, number of previous depressive episodes, and stressful life events in a population-based sample of female twins followed longitudinally over four waves of personal interviews.
Method
The subjects in this study were members of Caucasian female-female twin pairs, born between 1934 and 1974, ascertained from the population-based Virginia Twin Registry (now part of the Mid-Atlantic Twin Registry). Twin pairs were eligible to participate if both members had previously responded to a mailed questionnaire, the response rate to which was approximately 64%. As detailed elsewhere (4), 88% of this group was first interviewed face-to-face in 1988–1989 and has subsequently been the subject of three additional telephone interview waves during the years 1990 to 1997. The rest of our female-female twin pair members were first interviewed face-to-face in 1992–1994 (counted as part of our wave 1) and interviewed a second time (as part of our wave 4 assessment) by telephone in 1996 and 1997. Signed informed consent was obtained before all face-to-face interviews, and verbal assent was obtained before all telephone interviews. Mean ages at each assessment wave were as follows: wave 1: mean=29.3 years (SD=7.7); wave 2: mean=31.6 (SD=7.5); wave 3: mean=35.1 (SD=7.5); and wave 4: mean=36.3 (SD=8.3).
The total number of twins who participated in any assessment wave was 2,395. The number of individuals (and resulting person-months) for each of the four waves of instruments was as follows: wave 1: N=2,164 (28,121 person-months); wave 2: N=2,003 (26,039 person-months); wave 3: N=1,899 (24,687 person-months); and wave 4: N=1,943 (25,259 person-months). Subject attrition across waves ranged from 8% to 15% (4). All assessments were separated by at least 13 months.
Assessment of Major Depression
The history of major depression was assessed by structured psychiatric interview based on the Structured Clinical Interview for DSM-III-R (SCID) (22, 23). At all interview waves, we assessed the occurrence over the last year of 14 individual symptoms, which represented the disaggregated nine “A criteria” for major depression in DSM-III-R (e.g., two items for criterion A4 to assess insomnia and hypersomnia). For each reported symptom, interviewers probed to ensure that it was due neither to physical illness nor medication. The respondents then had to aggregate symptoms reported over the last year into co-occurring syndromes. If depressive syndromes occurred, respondents were asked when they occurred and the months of their onset and remission. The diagnosis of major depression was made through a computer algorithm that incorporated the DSM-III-R criteria with the exception of criterion B2 (which excludes depressive syndromes considered to be “uncomplicated bereavement”). In 53 twins, the 1-year history of major depression and the dating of the depressive episode were assessed with excellent reliability (kappas of 1.00 and 0.97, respectively) (24).
At waves 1, 3, and 4, we also assessed the history of lifetime major depression before the last year, including total number of previous depressive episodes, by using the more traditional skip structure of the SCID. To assign individuals a number of previous depressive episodes that could be continuously updated over the ascertainment period, we began at wave 1 with the number of depressive episodes reported before the previous year (1LT). This number was updated by adding episodes reported during the year before the wave 1 interview (1LT+1LY) and updated again by adding episodes reported during the year before the wave 2 interview (1LT+1LY+2LY). This figure (1LT+1LY+2LY) was then compared with the number of lifetime episodes reported before the last year at wave 3 (3LT) and the larger of the two was taken and given the value of 3LT*. This was then updated by adding the number of new episodes reported during the year before the wave 3 interview (3LT*+3LY). This number (3LT*+3LY) was then compared with the number of lifetime episodes reported before the last year at wave 4 (4LT) and the larger of the two was taken and given the value of 4LT*. This was then updated by adding the number of new episodes reported during the year before the wave 4 interview (4LT*+4LY).
Assessment of Stressful Life Events
As detailed elsewhere (25, 26), in interview sections before those that covered major depression, we assessed the occurrence over the last year, to the nearest month, of 11 “personal” events (i.e., events that occurred primarily to the informant): assault, divorce/separation, major financial problems, serious housing problems, serious illness or injury, job loss, legal problems, loss of confidant, serious marital problems, robbery, and serious difficulties at work. We also assessed four classes of “network” events (i.e., events that occurred primarily to, or in interaction with, an individual in the respondent’s social network). These event classes consisted of 1) serious trouble getting along with an individual in the network, 2) a serious personal crisis of someone in the network, 3) death of an individual in the network, and 4) serious illness of someone in the network. We defined network as the respondent’s spouse, child, parent, co-twin, and other nontwin siblings. The items assessing these events were similar but not always identical over waves. In addition, we lacked an assessment of housing problems at wave 1 and network crises at wave 2. In wave 1, we assessed the interrater reliability for the occurrence and dating of our stressful life event categories and found them to be in the good to excellent range, with kappas equaling 0.93 and 0.82, respectively (N=53) (25).
In waves 3 and 4 only, each reported stressful life event was rated by the interviewer on its level of long-term contextual threat and dependence (26). After Brown (27), long-term contextual threat was rated on a 4-point scale: minor, low moderate, high moderate, and severe. In these analyses, all months were scored on a 5-point scale for which 1 through 5 reflected the most severe long-term contextual threat rating of any event that occurred in that month (a score of 0 meant no event occurrence). Therefore, the odds ratios in these analyses reflect the increased risk for a depressive onset for each unit on this long-term contextual threat scale.
Dependence, reflecting the contribution of the respondent to the stressful life event, was also rated on a 4-point scale: clearly independent, probably independent, probably dependent, and clearly dependent. In these analyses, we dichotomized stressful life events as those clearly or probably independent versus those clearly or probably dependent. Reliability of our ratings of long-term contextual threat and dependence were determined by both an interrater and test-retest design. Interrater reliability was assessed by having experienced interviewers, blind to the original codings, review tape recordings of the interview sections in which 92 randomly selected individual stressful life events were evaluated. Test-retest reliability was obtained by blindly reinterviewing 191 respondents at a mean interval of 4 weeks. We obtained 173 scored life events that were reported to have occurred within 1 month of one another and, we assumed, represented the same event. Spearman correlations and weighted kappas (28) were used to assess test-retest reliability (long-term contextual threat: rs=0.60 and kappa=0.41; dependence: rs=0.77 and kappa=0.63) and interrater reliability (long-term contextual threat: rs=0.69 and kappa=0.67; dependence: rs=0.89 and kappa=0.79) for these 4-point scales.
Statistical Analysis
We sought to clarify whether the association between stressful life events and major depression changed as a function of previous depressive episodes by using an event history analysis with a discrete-time approach (29–31). The unit of these analyses was the “person-month.” Data used in these analyses were collected at up to four different interview waves with an individual twin and always concerned onsets and events that occurred within the last year. For each of these months, we recorded which, if any, stressful life events had occurred and whether an episode of major depression had started. Each observation record also included three covariates: age, the hazard rate for major depression for that month (to account for the fact that episodes of major depression were not entirely evenly distributed over the last year) and genetic risk for major depression, indexed by zygosity and co-twin lifetime history for major depression (25). When a twin experienced an episode of major depression, she was censored until recovery, at which time she reentered the study group with the previous depressive episodes variable updated. In addition, our cohort had a number of women who reported having chronic depression that began before our period of ascertainment. These individuals were not considered to have an onset of major depression in the first study month and were censored from the group for the period they reported meeting criteria for major depression.
These analyses treat each individual person-month as an independent observation with the risk of having an onset of major depression modeled as the dependent variable in a logistic regression. Allison (29, 31) has shown that, under the assumption of independence of the individual observations, given one “failure” event per subject, such a model produces the true maximum likelihood estimators and artifactually inflates neither the sample size nor the test statistic. Some of our twins reported multiple depressive onsets. However, by including previous depressive episodes as a covariate, we accounted for the major source of nonindependence of individual person-months. Any residual violations of this assumption will result in standard error estimates that are downward biased, while parameter estimation is unlikely to be affected. The odds ratio for major depression given stressful life events is calculated from the logistic regression coefficient after controlling for all the aforementioned covariates. In these analyses, we examine only the onset of major depression in the month of event occurrence, as most of the depressogenic impact of stressful life events occurs shortly after the stressful life event (25, 26). Although our hypotheses were nearly always directional, two-tailed p values are reported.
To examine the interaction between stressful life events and previous depressive episodes in the prediction of major depression, we had to properly specify the relationship between previous depressive episodes and risk for major depression, which was complex and clearly nonlinear (Figure 1). To capture this nonlinearity, we used a piece-wise, discrete-time survival logistic regression (32). This model assumes that the relationship between previous depressive episodes and major depression can be best captured by two distinct straight lines instead of one. Over part of the range of previous depressive episodes, one linear relationship best describes the relationship between previous depressive episodes and risk for major depression. Over the remainder of the range of previous depressive episodes, the model assumes that the association between previous depressive episode and major depression is best described by a different linear component. The key then becomes to find the inflection point between these two lines, which we did by maximizing the likelihood of the regression model. The odds ratio for the second section of the regression line represents the change in the regression relationship, so to determine the slope and odds ratio of the second portion of the curve, it is necessary to multiply the two odds ratios.
Results from these analyses represent both within-individual and across-individual differences in the relationship between stressful life events and major depression with increasing numbers of previous depressive episodes. It was also important to isolate for examination solely the within-individual changes in sensitivity to the depressogenic effects of stressful life events. Our attempts to do this with discrete-time survival analysis proved intractable, since the requirement to estimate each individual’s survival curve in our large sample exceeded available memory. Therefore, we used a fixed-effects partial likelihood Cox proportional hazards model as described by Allison (33) with the addition of multiple time-dependent failures (e.g., depressive onsets). Life events were treated as time-dependent covariates. The analysis is stratified by subject, so that we can examine the within-person changes in the strength of the association between stressful life events and depressive onsets as a function of number of previous depressive episodes.
Results
Our analyses began with a total of 104,106 person-months of observation. In the basic model, one or more data points were missing in 156 person-months, and 2,994 person-months were censored because the individual was in an episode of major depression during that month. This left us with a total of 100,956 person-months that contained 1,419 onsets of major depression. In analyses that required information about the lifetime history of major depression in the co-twin, our sample consisted of 97,515 person-months with 1,380 depressive onsets.
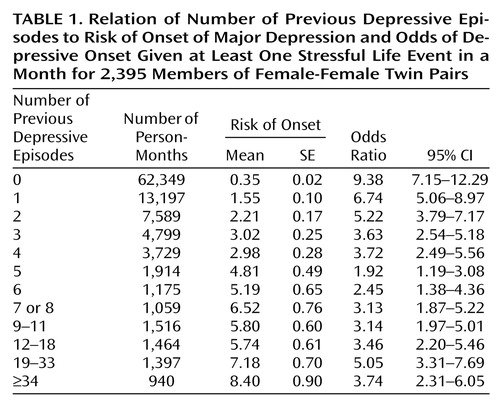
Before formal analysis, we explored the shape of the relationship between the number of previous depressive episodes and risk for depressive episodes. To do so, we divided person-months into 12 groups as a function of number of previous depressive episodes. As seen in Table 1, each of these groups, except the last, contained at least 1,000 person-months. We then calculated the rate of depressive onsets in each group of person-months, and this varied from 220/62,349=0.35% for those with no previous depressive episodes to 79/940=8.40% for those with 34 or more previous depressive episodes. As seen in Figure 1 and Table 1, the relationship was biphasic: the risk for a depressive episode rose steeply as the number of previous depressive episodes increased from none to approximately eight or nine. As the number of previous depressive episodes increased beyond this point, the risk for major depression dipped slightly and then rose again but at a much slower rate.
Discrete-Time Survival Models
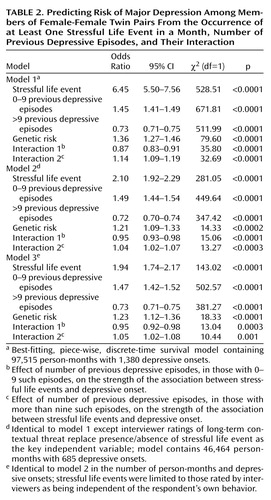
We present in detail results for the models in which we attempted to predict, for each month, the risk of a depressive onset from the occurrence of one or more stressful life events (coded as a dichotomous variable), the number of previous depressive episodes, and their interaction. Given the shape of the relationship revealed in Figure 1, we fitted model 1 with two linear components (i.e., a piece-wise regression), determining the optimal inflection point by testing sequentially each point from one to 12 previous depressive episodes. For this and all subsequent models, the best model likelihood was seen for an inflection point at nine previous depressive episodes. Only 5,299 person-months (5.2% of the total) had nine or more previous depressive episodes, so our analyses will focus on the first linear component, which contains most of our data.
As seen in Table 2, the occurrence of one or more stressful life events, with an odds ratio of 6.45, had a strong impact on the risk for a depressive onset. The impact of the number of previous episodes was divided into two regression lines of differing slope. From zero to nine, the number of previous depressive episodes strongly predicted an increasing risk for a depressive episode with an odds ratio of 1.45. For more than nine previous episodes, the odds ratio was 0.73 × 1.45=1.06. Once an individual had accumulated at least nine previous depressive episodes, the increased risk associated with each additional episode was modest, although statistically significant. Also, as expected, the rate of depressive onsets was significantly predicted by level of genetic risk.
Our key hypothesis predicted an interaction in the prediction of risk for major depression between the number of previous depressive episodes and stressful life events. Specifically, we predicted that with an increasing number of previous depressive episodes, the strength of the association between stressful life events and depressive onsets would diminish. For those person-months in individuals with zero to nine previous depressive episodes, we saw exactly this kind of interaction (χ2=35.80, df=1, p<0.0001; odds ratio=0.87). This odds ratio means that for each additional previous depressive episode from zero to nine, the strength of the association between stressful life events and depressive onsets declined approximately 13%. There was also a significant interaction between number of previous depressive episodes and stressful life events in predicting major depression for those with nine or more previous episodes (χ2=32.69, df=1, p<0.0001; odds ratio=0.87 × 1.14=0.99). As the number of previous depressive episodes increased beyond nine, the strength of the association between stressful life events and depression continued to decline but at a much slower rate (approximately 1% per episode).
To illustrate these results, we calculated, from the raw data, the odds ratio between major depression and one or more stressful life events as a function of the number of previous depressive episodes (Table 1 and Figure 1). The interaction between stressful life events and previous depressive episodes from zero to nine in the prediction of depressive onsets is clearly seen. For individuals with no previous depressive episodes, life event occurrence and the onset of major depression is strongly associated (odds ratio=9.38). The odds ratio, however, drops swiftly to the range of 2 to 3 as the number of previous depressive episodes increases to five through eight. The interaction between stressful life events and nine or more previous depressive episodes in the prediction of major depression cannot be clearly seen with this raw data, since there appears to be no overall change in the strength of the association between stressful life event and major depression as the number of previous depressive episodes further increases.
In the last two waves of personal interviews, we collected information on long-term contextual threat and dependence for each individual stressful life event. Including data from subjects who reported a lifetime history of major depression in the co-twin provided 46,464 person-months of exposure and 685 onsets of major depression. Model 2 was identical to model 1 except that we used the long-term contextual threat ratings assigned by the interviewers as the key independent measure. That is, instead of predicting onsets of major depression from the presence or absence of a stressful life event in a given month, we now predicted depressive onsets from a 5-point scale ranging from no event to an event of maximal long-term contextual threat. The best-fit model was qualitatively very similar to that seen with model 1 (Table 2). We found strong main effects for the impact of genetic factors, stressful life events, both components of the regression line for number of previous depressive episodes, and strong evidence in favor of the kindling effects in that both interactions between previous depressive episodes and stressful life events were highly significant.
Our two previous models had included all stressful life events including those likely to be a result of the respondent’s own actions. Therefore, our final model was restricted only to those life events rated by interviewers as probably or definitely independent of the respondent’s own behavior. Although the number of person-months with stressful life events declined, the overall pattern of findings was remarkably similar. The significance of the main effect of stressful life events declined due to the reduced number of events. However, both the main effects of the number of previous depressive episodes as well as the interactions between the number of previous depressive episodes and stressful life events were similar to that seen with the previous models (Table 2).
Within-Person Analyses
The final question we sought to answer was whether the change in sensitivity to the effects of stressful life events over episodes varied within as well as across individuals.
To address this question, we used a fixed-effects partial likelihood Cox proportional hazards model (33) with the addition of multiple time-dependent failures and time-dependent covariates. Because of limited power, we only examined the first linear component of the relationship between previous depressive episodes and risk for major depression (i.e., between zero and nine previous depressive episodes). We began by fitting this model to the entire data set, estimating a single underlying hazard function. The parameter estimates of this model were quite similar to those found with our discrete-time survival analyses (Table 1). In particular, we found a highly significant interaction between number of previous depressive episodes and the occurrence of one or more stressful life events (b=–0.13, χ2=33.85, df=1, p<0.0001; odds ratio=0.88). Next, we stratified by individual, assuming a separate hazard function for each person in the sample. The magnitude of the interaction between previous depressive episodes and stressful life events was essentially unchanged (b=–0.12, χ2=11.74, df=1, p=0.0006, odds ratio=0.89). These results indicate that the observed decline in the association between stressful life events and depressive onsets with increasing numbers of previous depressive episodes is a true within-individual phenomenon and cannot be explained by systematic differences between the kind of individuals who have a low versus high number of previous depressive episodes.
Discussion
The goal of this study was to clarify the impact of the number of previous depressive episodes on the association between the occurrence of stressful life events and the risk for depressive episodes. Consistent with the kindling hypothesis, previous research had suggested that the strength of the relationship between stressful life events and major depression declined with an increasing number of previous depressive episodes (9–15). However, these previous studies had at least several potential methodological limitations that we were able to address in our analyses. We first review our results and then interpret them in the light of these potential methodological issues.
In examining the raw data on previous depressive episodes, stressful life events, and depressive onsets in our sample of over 100,000 person-months of exposure, two facts became clear. First, the number of previous depressive episodes had a strong effect on the association between stressful life events and depressive onsets. Second, the shape of this relationship was biphasic. An increase in previous depressive episodes impacted much more strongly on the relationship between stressful life events and major depression when the number of previous depressive episodes was less than 10.
We modeled this biphasic relationship by using discrete-time survival analysis and piece-wise regression. Across all models, the best fit was found when the point of inflection in the biphasic regression curve was set at nine previous depressive episodes. We then presented the parameters of a series of best-fit models. Qualitatively, the models all told the same story. As shown by numerous previous investigators (e.g., references 34–38), stressful life events were strong risk factors for the onset of major depression. The main effect of previous depressive episodes was divided into two portions. When the number of previous depressive episodes was nine or fewer, each additional previous depressive episode conveyed a large increased risk for a depressive onset. After nine previous depressive episodes, each additional episode conveyed a much smaller increased risk.
Our real interest, however, was in testing whether, as predicted by the kindling model, we would observe an interaction between previous depressive episodes and stressful life events in the prediction of risk for major depression. Indeed, we found strong and consistent evidence for a negative interaction. That is, with each new previous depressive episode, the association between stressful life events and onsets of major depression became progressively weaker. This effect was striking between zero and six to eight previous depressive episodes. These results are consistent with prediction of the kindling hypothesis.
Given the nonexperimental nature of these results, a careful review of possible sources of biases is warranted. First, because our twins were selected from a birth-certificate-based twin registry, these results cannot plausibly result from the confounding effect of help-seeking behavior. Second, by testing the kindling hypothesis as an interaction between stressful life events and previous depressive episodes, we ensured that our results could not be influenced by changes in the base rate of stressful life events with increasing number of previous depressive episodes, which was indeed seen in our data. Third, the severity of stressful life events was positively and significantly correlated with the number of previous depressive episodes. That is, individuals with large numbers of previous depressive episodes on average had more severe kinds of stressful life events. In the last two waves of our sample, on the basis of information provided by the respondent, interviewers rated each individual stressful life event on a measure of severity (long-term contextual threat [27]). Controlling for the severity of stressful life events produced no substantial change in the pattern of results.
Fourth, the greatest interpretational difficulty with previous studies of the kindling hypothesis is the problem of clarifying the causal relationship between previous depressive episodes and the association between stressful life events and major depression. While the pattern of results from these cross-sectional studies could result from a causal impact of previous depressive episodes on event sensitivity, a noncausal explanation is also plausible. Assume that we could divide individuals into two groups, the first of which has a low liability to major depression so that depressive episodes only occur in the setting of severe stressful life events. The second group, which has high liability to major depression, frequently has episodes without substantial environmental stress. In a cross-sectional study of depressed patients, the mixture of these two groups would produce an apparent association between number of previous depressive episodes and the stressful life event-major depression relationship. This would occur because the first group would predominate in those with no previous depressive episodes (where the association between stressful life events and major depression would be strong) and the second group would be more common in those with recurrent episodes (where the association between stressful life events and major depression association would be weak).
We proposed two ways to address this critical interpretational difficulty. Because of the twin structure of our data, we controlled for the level of genetic risk to major depression in all of our analyses. Because of the longitudinal nature of our data, we could also examine within-individual changes in event sensitivity with increasing previous depressive episodes. For example, imagine an individual twin whom we interviewed over all four waves and who therefore had 52 person-months of observations in our data. Assume that she had her first depressive episode in months 9 to 11 and a second episode in months 40 to 44. We could compare the strength of the association between the occurrence of stressful life events and the risk for major depression in months 1–9 (when she had no previous depressive episodes), 12–40 (when she had one previous depressive episode) and 45–52 (when she had two previous depressive episodes). (She would be censored from analysis for months 10 and 11 and 41–44 when she was in a depressive episode.) Controlling for interindividual differences in liability to major depression, these analyses strongly supported a causal interpretation of the kindling effect because they showed a substantial reduction in the strength of the association between stressful life events and major depression within individuals as they accumulated more previous depressive episodes over time.
These results should be interpreted in the context of six potential methodological limitations. First, the study group was entirely female, and it cannot be assumed that the same relationship between previous depressive episodes, stressful life events, and major depression would be seen in male subjects. Second, all participants were twins. However, twins have rates of psychiatric symptoms (39) and disorders (40) similar to the general population. Because the subjects came from twin pairs, nonindependence of observations from members of a pair is a potential concern. We have previously examined the correlation in twin pairs for the key dependent variable (month of occurrence of a depressive onset) in this group, and it was too low (kappa=0.01) to be of practical concern (26). To further examine the possible magnitude of this problem, we re-ran model 1 by using general estimating equations (41) to correct for the correlations in twin pairs. The parameter estimates changed trivially.
Third, as in most such studies, stressful life events and the onset of major depression were rated retrospectively over the 1-year period before interview. Although stressful life events were assessed in a separate and earlier section of the interview than major depression, part of the observed association could be spurious and result from biased recollection.
Fourth, the reliability of the assessment of lifetime major depression in community samples is modest (42, 43). As the 1-year periods of assessment in our longitudinal sample were not contiguous, the accuracy of our assessments of depressive episodes in the intervening periods is likely to be of only moderate accuracy. Also, among those who report a lifetime history of major depression, the number of reported previous depressive episodes is also of only moderate reliability. In this study, short-term test-retest for number of previous depressive episodes, as assessed by a Spearman rank correlation was 0.48 (N=192; p<0.0001), similar to that found previously (44, 45).
Fifth, these analyses included 18 twins with a lifetime diagnosis of mania or hypomania (46). Since the kindling process may differ in bipolar and unipolar illness, we reran model 1 excluding these twins. The results did not change substantially.
Finally, we assumed that when a stressful life event and depressive onset occurred in the same month, the stressful life event came first. In a section of the interview separate from that which evaluated stressful life events, respondents with a depressive syndrome in the last year were asked, “Did something happen to make you feel that way or did the feeling just come on you ‘out of the blue?’ ” We have examined, in two separate waves of our data, twins who reported a stressful life event and a depressive onset occurring in the same month, and who answered this question in sufficient detail to examine. We found that 84% (25) and 85% (26) responded with the stressful life event they had previously reported as occurring in the same month. In none of the remaining cases did the interview indicate that the stressful life event occurred as a result of the onset of a depressive episode.
Conclusions
Although methodological artifacts cannot be excluded, our results provide strong support for the hypothesis that the strength of the association between stressful life events and depressive onsets declines with increasing number of previous depressive episodes. These findings also suggest that, whatever the biological or psychological process that underlies this phenomenon (Post [7] suggested gene transcription), it is “saturable.” That is, most of the changes that occur do so in the first few episodes of illness. If this phenomenon results from the brain or mind learning to become depressed, this learning appears to occur intensely over the first few episodes of illness and then, with further episodes, either slows down or stops altogether.
 |
 |
Received July 19, 1999; revision received Jan. 11, 2000; accepted March 9, 2000. From the Departments of Psychiatry and Human Genetics, Medical College of Virginia of Virginia Commonwealth University, Richmond; and the Virginia Institute for Psychiatric and Behavioral Genetics. Address reprint requests to Dr. Kendler, Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Box 980126, Richmond, VA 23298-0126.Supported by grants from NIMH (MH-40828), the National Institute on Alcohol Abuse and Alcoholism (AA-09095), and a Research Scientist Award (MH-01277) to Dr. Kendler. The Virginia Twin Registry, established by W. Nance, M.D., Ph.D., and maintained by L. Corey, Ph.D., is supported by NIH grants HD-26746 and NS-31564.The authors thank Sarah Burns, M.A., and Frank Butera, M.S., for their supervision of the data collection.
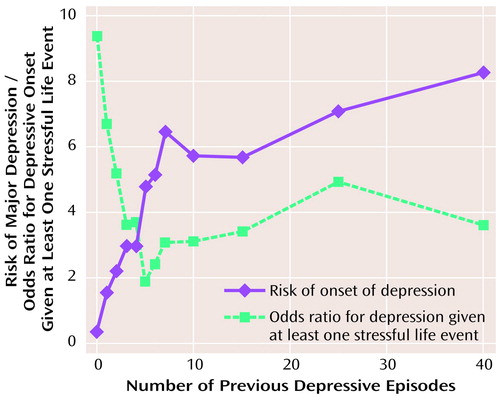
Figure 1. Nature of the Relationship Between the Number of Previous Depressive Episodes and 1) the Monthly Risk for Onset of Major Depression and 2) the Odds Ratio Between the Occurrence of at Least One Stressful Life Event in a Month and the Probability of a Depressive Onset in That Montha
aFor sample sizes, standard errors, and confidence intervals (CIs) for these results, see Table 1
1. Kessler RC: The effects of stressful life events on depression. Ann Rev Psychol 1997; 48:191–214Crossref, Medline, Google Scholar
2. Tsuang MT, Faraone SV: The Genetics of Mood Disorders. Baltimore, Johns Hopkins University Press, 1990Google Scholar
3. McGuffin P, Katz R, Watkins S, Rutherford J: A hospital-based twin register of the heritability of DSM-IV unipolar depression. Arch Gen Psychiatry 1996; 53:129–136Crossref, Medline, Google Scholar
4. Kendler KS, Prescott CA: A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry 1999; 56:39–44Crossref, Medline, Google Scholar
5. Kendler KS, Kessler RC, Neale MC, Heath AC, Eaves LJ: The prediction of major depression in women: an integrated etiologic model. Am J Psychiatry 1993; 150:1139–1148Google Scholar
6. Kraepelin E: Manic-Depressive Insanity and Paranoia. Translated by Barclay RM, edited by Robertson GM. Edinburgh, E & S Livingstone, 1921Google Scholar
7. Post RM: Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 1992; 149:999–1010Google Scholar
8. Segal ZV, Williams JM, Teasdale JD, Gemar M: A cognitive science perspective on kindling and episode sensitization in recurrent affective disorder. Psychol Med 1996; 26:371–380Crossref, Medline, Google Scholar
9. Perris H: Life events and depression, part 2: results in diagnostic subgroups, and in relation to the recurrence of depression. J Affect Disord 1984; 7:25–36Crossref, Medline, Google Scholar
10. Dolan RJ, Calloway SP, Fonagy P, De Souza FVA, Wakeling A: Life events, depression and hypothalamic-pituitary-adrenal axis function. Br J Psychiatry 1985; 147:429–433Crossref, Medline, Google Scholar
11. Ezquiaga E, Gutierrez JLA, Lopez AG: Psychosocial factors and episode number in depression. J Affect Disord 1987; 12:135–138Crossref, Medline, Google Scholar
12. Cassano GB, Akiskal HS, Musetti L, Perugi G, Soriani A, Mignani V: Psychopathology, temperament, and past course in primary major depressions. Psychopathology 1989; 22:278–288Crossref, Medline, Google Scholar
13. Ghaziuddin M, Ghaziuddin N, Stein GS: Life events and the recurrence of depression. Can J Psychiatry 1990; 35:239–242Crossref, Medline, Google Scholar
14. Brown GW, Harris TO, Hepworth C: Life events and endogenous depression. Arch Gen Psychiatry 1994; 51:525–534Crossref, Medline, Google Scholar
15. Bruce ML: Divorce and psychopathology, in Adversity, Stress, and Psychopathology. Edited by Dohrenwend BP. New York, Oxford University Press, 1997, pp 219–234Google Scholar
16. Brown GW, Sklair F, Harris TO, Birley JLT: Life events and psychiatric disorders, I: some methodological issues. Psychol Med 1973; 3:74–87Crossref, Medline, Google Scholar
17. Gershon ES, Weissman MM, Guroff JJ, Prusoff BA, Leckman JF: Validation of criteria for major depression through controlled family study. J Affect Disord 1986; 11:125–131Crossref, Medline, Google Scholar
18. Bland RC, Newman SC, Orn H: Recurrent and nonrecurrent depression: a family study. Arch Gen Psychiatry 1986; 43:1085–1089Google Scholar
19. Weissman MM, Merikangas KR, Wickramaratne P, Kidd KK, Prusoff BA, Leckman JF, Pauls DL: Understanding the clinical heterogeneity of major depression using family data. Arch Gen Psychiatry 1986; 43:430–434Crossref, Medline, Google Scholar
20. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: The clinical characteristics of major depression as indices of the familial risk to illness. Br J Psychiatry 1994; 165:66–72Crossref, Medline, Google Scholar
21. Kendler KS, Gardner CO, Prescott CA: Clinical characteristics of major depression that predict risk of depression in relatives. Arch Gen Psychiatry 1999; 56:322–327Crossref, Medline, Google Scholar
22. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A population-based twin study of major depression in women: the impact of varying definitions of illness. Arch Gen Psychiatry 1992; 49:257–266Crossref, Medline, Google Scholar
23. Spitzer RL, Williams JBW: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1985Google Scholar
24. Cohen J: A coefficient of agreement for nominal scales. Educational and Psychol Measurement 1960; 20:37–46Crossref, Google Scholar
25. Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, Eaves LJ: Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiatry 1995; 152:833–842Link, Google Scholar
26. Kendler KS, Karkowski L, Prescott CA: Stressful life events and major depression: risk period, long-term contextual threat and diagnostic specificity. J Nerv Ment Dis 1998; 186:661–669Crossref, Medline, Google Scholar
27. Brown GW: Life events and measurement, in Life Events and Illness. Edited by Brown GW, Harris TO. New York, Guilford, 1989, pp 3–45Google Scholar
28. Fleiss JS, Cohen J, Everett BS: Large sample standard errors of kappa and weighted kappa. Psychol Bull 1969; 72:323–327Crossref, Google Scholar
29. Allison PD: Discrete-time methods for the analysis of event histories, in Sociological Methodology. Edited by Leinhardt S. San Francisco, Jossey-Bass, 1982, pp 61–98Google Scholar
30. Laird N, Olivier D: Covariance analysis of censored survival data using log-linear analysis techniques. J Am Statistical Assoc 1981; 76:231–240Crossref, Google Scholar
31. Allison PD: Survival Analysis Using the SAS System: A Practical Guide, 2nd ed. Cary, NC, SAS Institute, 1995Google Scholar
32. Neter J, Wasserman W, Kutner MH: Applied Linear Statistical Models, 3rd ed. Edited by Hercher RT Jr, Shiell E. Boston, Irwin, 1990Google Scholar
33. Allison PD: Fixed-effects partial likelihood for repeated events. Sociological Methods and Res 1996; 25:207–222Crossref, Google Scholar
34. Paykel ES: Contribution of life events to causation of psychiatric illness. Psychol Med 1978; 8:245–253Crossref, Medline, Google Scholar
35. Brown GW, Harris TO: Social Origins of Depression: A Study of Psychiatric Disorder in Women. London, Tavistock, 1978Google Scholar
36. Costello CG: Social factors associated with depression: a retrospective community study. Psychol Med 1982; 12:329–339Crossref, Medline, Google Scholar
37. Surtees PG, Miller PM, Ingham JG, Kreitman NB, Rennie D, Sashidharan SP: Life events and the onset of affective disorder: a longitudinal general population study. J Affect Disord 1986; 10:37–50Crossref, Medline, Google Scholar
38. Bebbington PE, Sturt E, Tennant C, Hurry J: Misfortune and resilience: a community study of women. Psychol Med 1984; 14:347–363Crossref, Medline, Google Scholar
39. Kendler KS, Martin NG, Heath AC, Eaves LJ: Self-report psychiatric symptoms in twins and their nontwin relatives: are twins different? Am J Med Genet Neuropsychiatr Genet 1995; 60:588–591Google Scholar
40. Kendler KS, Pedersen NL, Farahmand BY, Persson P-G: The treated incidence of psychotic and affective illness in twins compared to population expectation: a study in the Swedish Twin and Psychiatric Registries. Psychol Med 1996; 26:1135–1144Google Scholar
41. SAS/STAT Software: Changes and Enhancements Through Release 6.12, Cary, NC, SAS Institute, 1997Google Scholar
42. Rice JP, Rochberg M, Endicott J, Lavori PW, Miller C: Stability of psychiatric diagnoses: an application to the affective disorders. Arch Gen Psychiatry 1992; 49:824–830Crossref, Medline, Google Scholar
43. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: The lifetime history of major depression in women: reliability of diagnosis and heritability. Arch Gen Psychiatry 1993; 50:863–870Crossref, Medline, Google Scholar
44. Mazure C, Gershon ES: Blindness and reliability in lifetime psychiatric diagnosis. Arch Gen Psychiatry 1979; 36:521–525Crossref, Medline, Google Scholar
45. Bromet EJ, Dunn LO, Connell MM, Dew MA, Schulberg HC: Long-term reliability of diagnosing lifetime major depression in a community sample. Arch Gen Psychiatry 1986; 43:435–440Crossref, Medline, Google Scholar
46. Karkowski LM, Kendler KS: An examination of the genetic relationship between bipolar and unipolar illness in an epidemiologic sample. Psychiatr Genet 1997; 7:159–163Crossref, Medline, Google Scholar



