Twin Sisters With Psychotic Disorders
These cases of twin sisters with psychotic illness were presented in a case conference to enhance the treatment of each twin by examining both cases together, to inform clinicians regarding issues relevant to the care of twins, and to evaluate the roles of genetics and environment in psychosis. Although the zygosity of these twins is open to question in the absence of blood group analysis or other genetic markers, several observations associated with monozygosity (1) are apparent in these cases. Specifically, childhood photographs show remarkable similarities in appearance of the twins, family members perceived them as identical, and examination of their placenta led the obstetrician to state they were most likely monozygotic. Today zygosity can be determined by a knowledgeably performed examination of the placenta and membranes at the time of birth in about two-thirds of cases (2).
Case Presentation
Jane and Susan are 43-year-old, single, white, left-handed, Jewish women with the same current clinical diagnosis: schizoaffective disorder and a personality disorder characterized by unstable interpersonal relationships, identity disturbance, and affective instability. Both also have reading problems, and they were diagnosed with dyslexia in childhood. During the last year, Jane has been a patient in a research unit and has subsequently been treated both in the day hospital and by the continuing care service of a mental health center on the East Coast. During the 1970s and 1980s, Susan received inpatient and outpatient treatment at this center. She has lived on the West Coast for the last 6 years.
Psychiatric Histories
Jane
Jane was admitted to the mental health center for the first time at the age of 23, when she drank a nonlethal amount of paint thinner in an attempt to end her life. Precipitants to Jane’s admission seemed to be Susan’s first admission less than 12 months previously and the little contact Jane had had with her therapist during the preceding months. At that time, Jane was described in her records as paranoid, disorganized, and preoccupied with her therapist’s family, vitamin therapy, and her weight. She was treated with thiothixene, 400 mg/day.
Since then Jane has been readmitted nine times (Figure 1). Precipitants have been mainly changes in relationships (e.g., mother moving to a different state, conflicts in relationships with Susan, a therapist, and a significant other), job-related stress, and medication noncompliance. She has believed she was God; however, she has also heard voices of God referring to a man she met during a trip to Israel, and she has received messages from cars telling her to kill people. She has been variously described as cheerful, restless, and overtalkative and at other times as sad and suicidal, although these mood symptoms have not always been present. She has had suicidal ideation many times but has not injured herself since her early suicide attempt. She has, however, tried to hurt others, such as when she unsuccessfully attempted to smother her roommate with a pillow during one admission.
Jane was treated with lithium (up to 1500 mg/day) for approximately 16 years (age 25–41) in combination with perphenazine (up to 32 mg/day) for over 10 years (age 31–41). Lithium and perphenazine were discontinued because of uncontrolled symptoms and tardive dyskinesia, and olanzapine was used briefly before switching to clozapine treatment. Her current medication regimen includes clozapine, 425 mg/day, and clonazepam, 0.5 mg/day. She has been in individual and group therapy and in day programs. She currently sees a male psychiatrist for both medications and therapy. Her longest period without mental health center admissions (age 31–38) occurred during treatment with lithium and perphenazine, beginning immediately after termination with the female therapist she had seen since age 20. It was also during these 4.5 years of apparent “remission” that she had her only relationships, sequentially, with three significant others. During that time she lived with significant others and then with her mother and worked intermittently. Her admission at age 38 was precipitated by suspicion that a significant other had stolen her money.
Jane has worked as a waiter, a taxicab driver, and in real estate sales, although she is currently unemployed and receives Social Security Disability Insurance. She has had multiple sexual partners, including men and women, but currently has no significant other. She has not been married, has no children, and has had no pregnancies. She lives alone in an apartment.
Jane’s past medical history is significant for a left ovarian cyst diagnosed at age 40. She had normal head magnetic resonance imaging (MRI) and an EEG at age 42.
Susan
Susan was first admitted at age 22, after she had just lost a boyfriend, had not seen her therapist for 2 months, had just received a marriage proposal, and was facing final examinations in school. She thought that the radio was speaking to her and that the bottom of her body was falling off. She was described then as paranoid and disorganized, with thought blocking and loose associations. She was treated with trifluoperazine, 20 mg/day.
She was subsequently admitted eight more times, but she has not been admitted in over 7 years (Figure 1). Like Jane, precipitants to Susan’s admissions have usually been changes in relationships (e.g., changes in her relationship with Jane, therapists being away, feeling “too close” early in relationships with potential boyfriends), job-related stress, and medication noncompliance. Like Jane, Susan has experienced hearing voices of birds telling her to take her life. She has also been variously described as euphoric and depressed, but mood symptoms have not always been present. She has had suicidal ideation less frequently than Jane and has never injured herself. Like Jane, she has tried to hurt others, including hitting staff members, during two admissions.
Susan’s medication regimen has been similar to Jane’s. She was treated with a combination of lithium (up to 1500 mg/day) and a typical antipsychotic, trifluoperazine (up to 60 mg/day), for approximately 14 years (age 25–39). After she developed tardive dyskinesia, her trifluoperazine treatment was switched initially to risperidone and then to clozapine. She currently takes 600 mg/day of lithium carbonate, 425 mg/day of clozapine, and 20 mg/day of paroxetine for her anxiety symptoms. Susan has been in individual and group therapy and in day programs. She currently sees a male psychiatrist and a female therapist. Her longest admission-free period continues at 7 years. During this time her lithium and antipsychotic medication treatments have been continuous, and Susan has had three relationships, the first two of which lasted 6 months and the last of which continues after approximately 6 years. These are her only relationships with significant others that have lasted for more than 3 months. Earlier admission-free periods were associated with a therapeutic relationship (age 26–30) and with living with her mother (age 23–26).
Susan has worked as a bricklayer, ski instructor, and art therapist. She currently works part-time in food delivery and collects Supplemental Security Income and Social Security disability insurance. She has had numerous sexual relationships, mostly with men. She has not been married, has no children, and has had no pregnancies. She lives in a house with roommates.
Susan’s medical history is significant for one head injury with loss of consciousness when her father dropped her at age 18 months. She also had one seizure as a child, possibly febrile. When she was 40, a pituitary microadenoma was diagnosed and treated with bromocriptine, up to 7.5 mg/day. Bromocriptine treatment was discontinued after she began treatment with clozapine. Except for the pituitary microadenoma, the results of head computerized tomography scans and MRIs were normal at age 40; an EEG at age 30 was normal.
Psychological Testing
Neuropsychological and personality test results have been stable over many years. The best WAIS-R full-scale IQ estimates are 97 for Jane and 87 for Susan. Jane’s verbal IQ of 96 is notably higher than Susan’s 77. Both rank high on WAIS-R tests of fluid reasoning with nonverbal materials. Susan is stronger on visual tests that rely heavily on attention, sequencing, and an understanding of social schemas. Both have reading comprehension problems, but Susan’s are worse. Both have attention or executive system dysfunction, which is evident in difficulties encoding supra-span information and on the Wisconsin Card Sorting Test (3), but Jane’s is more pronounced.
On the basis of the MMPI, both women were noted to be narcissistic, but Susan seemed especially sensitive, thin skinned, and high strung. On the basis of the Thematic Apperception Test (4), Jane was noted to be particularly sensitive to affective arousal and quite susceptible to becoming disorganized. On the basis of the Rorschach test, both sisters are seen as having borderline character structures with impaired object relations, poor impulse control, and inadequate ego development. Both have been confused about their sexuality.
Family Psychiatric History
The twins report that their brother, now 39, has an affective disorder and dyslexia. Records indicate that both parents have suffered from affective disorders. According to the twins, one of their father’s sisters has an affective disorder. According to records, their paternal grandmother had a psychotic illness, the nature of which is not clear. Susan and her mother state that their paternal grandmother suffered from epilepsy. Records state that their maternal grandmother experienced postpartum depression.
Personal Developmental History
The twins were born after a normal pregnancy. Jane was delivered first, by low forceps, and weighed 2544 g. Susan was delivered spontaneously and weighed 2296 g. Records indicate they were normal newborns, and their mother reports they passed developmental milestones at appropriate ages.
Family life was chaotic. The twins’ father, an electrical engineer, had an explosive temper. The children feared him. They have described their mother, an actress and real estate broker, as self-centered. Their only sibling, a brother, is 4 years younger. Jane says that he has been cruel to her (e.g., once when she asked him to take her to the hospital, he took the keys to the car and left her at home alone). However, Susan has enjoyed a close relationship with him.
Both twins were diagnosed with dyslexia in grammar school and were subsequently tutored. When they were age 12, their parents divorced, triggering a period of instability in their living arrangements. During this time they lived variously with their mother and her boyfriend, at boarding school, and with their father and his new wife. While at boarding school, they experimented with LSD (Jane, “a few” times; Susan, approximately 20 times) and marijuana. At age 18 they graduated from high school and started living separately. Neither had many friends growing up. They do not report ever being physically or sexually abused.
They dropped out of different colleges after 2 years. Jane majored in psychology; Susan, in art and recreation therapy. At the suggestion of their father’s third wife, who was a psychologist, they each started individual psychotherapy focusing on anxiety related to separating from their family (Jane at age 20; Susan at 19). Both developed intense relationships with their therapists.
The twins grew up together in a variety of different environments and later remained close, although they did not live together. Their courses of illness and treatment have shown remarkable similarity, although Jane has been admitted several times in recent years, whereas Susan has not been admitted during the last 7 years. The twins’ relationships with each other, with significant others, and with their mother, as well as their medication compliance, appear to be important influences on their courses of illness. Both enjoy the company of others but can become paranoid and disorganized in close relationships. Their histories indicate that Susan has been involved with her current boyfriend for over 6 years, by far the longest relationship of either twin. Susan’s sexual orientation has been mainly toward men; Jane’s has been toward both men and women. Although the twins were reluctant to discuss their relationship directly, histories and interviews suggest that they sincerely care for one another, although they may be competitive at times. Jane said only that she thinks her sister had a more severe psychotic illness and more severe dyslexia but has adapted better over time and that her sister has received more attention from their mother. Susan said only that she has a positive regard for Jane and thinks Jane is more outgoing.
Interviews
Jane (Interviewed by M.T.T.)
During the interview Jane appeared well groomed and was casually dressed. She was cooperative and made good eye contact. There were no obvious abnormalities of speech. Her mood was “fine.” Her affect was generally euthymic, although she occasionally appeared anxious and sad, appropriate to the content of her speech. Her thought process was somewhat tangential. Her thought content was significant for grandiose and paranoid delusions (e.g., she thought that she was supposed to marry Prince Charles and that the CIA was after her; she thought that she received messages from trucks). Jane expressed a wish to be more independent of her mother and the messages. She reported no frank auditory hallucinations and showed no evidence of suicidal or homicidal ideation. Her insight and judgment were poor.
Susan (Interviewed Via Telephone by J.P.K.)
Susan had no abnormalities of speech and described her mood as “pretty good.” According to her psychiatrist, she experiences intermittent anxiety, apathy, and amotivation, and her affect is often “blunted.” During the interview her thought process was goal directed, and she reported no auditory hallucinations or suicidal or homicidal ideation. She said she was not sure if other people could read her mind. She stated that medication and her relationship with her boyfriend have helped control her illness. Her insight and judgment were fair.
Discussion
DSM-IV Diagnosis
On the basis of the information gathered so far, the most likely diagnosis for axis I may be schizoaffective disorder, based on the presence of both schizophrenic psychotic symptoms and affective symptoms, relatives with a history of psychotic and affective disorders, and a chronic clinical course of illness. For axis II, results of psychological testing and clinical manifestation of behavior patterns characterized by unstable interpersonal relationships, identity disturbance, and affective instability suggest the most likely diagnosis may be a borderline personality disorder.
Courses of Illness: The Role of Relationships
Concordance rates for schizophrenia in monozygotic twins have been generally reported as less than 50% (5), rising with increasing severity of illness (6) and female sex (7). Nonschizophrenic co-twins have a wide variety of clinical pictures, ranging from psychotic conditions to no mental illness (8). Studies of discordant pairs have shown that birth order, birth weight, difficulties during birth, physical condition at birth, or physical strength in early childhood have generally not been associated with the development of schizophrenia (8, 9).
In contrast to discordant pairs, concordant pairs were closer to each other in childhood, were more often brought up alike by their parents, tended to have less social contact with other children, and tended to come from a lower social class and a worse economic situation than discordant pairs (7). Kringlen (10) found similarities in age at both onset and admission in concordant twins (less than 4 years in 65% and 50%, respectively). Abe (11) showed that monozygotic twins were more likely to have a similar age at first episode if they lived together than if they lived apart.
The most extensively reported cases of sisters with schizophrenia are probably the Genains, identical quadruplets with schizophrenia who were evaluated initially in their 20s and later followed up at age 51 (12). These patients suggested that premorbid personality was indicative of later functioning since the most dependent sister during childhood and adolescence had the most impaired functioning during adulthood.
Jane and Susan are similar in a variety of respects (Table 1), including age at beginning of therapy, age at first admission, number of admissions, and medication history. Yet, based on admission data, Susan appears to have functioned much better than Jane since age 35. During an earlier 4-year period (age 31–35), Jane seems to have generally functioned better than Susan.
Available information suggests that sibling identification (13) and rivalry (14) may be important influences on courses of illness. Jane’s first admission occurred within 1 year of Susan’s, when she drank paint thinner at the time Susan was working as an art and recreation therapist. Also, Susan was admitted 3 months later after assaulting Jane, saying she was “tired of caring for” her sister, and Jane stated in the interview that their mother paid more attention to Susan. In addition, Jane thinks that Susan has a more severe illness, despite the fact that Jane does not appear to be functioning as well as her sister at this time.
The presence of a significant other may lead to improved functioning in these patients because it lets each twin feel valued for herself and decreases the competition for the mother’s attention. Accordingly, Susan has rarely been without a significant other during the last 7 years and has not been admitted during that time, and Jane had relationships with significant others during the 4.5 years of her longest interval between admissions (age 31–38). The only admission of either twin while with a significant other was Jane’s at age 38.
In addition to relationships with significant others, relationships with mother and therapists seem to affect the frequency of admissions. Susan was not admitted while she lived with her mother (age 23–26). Jane lived with her mother for 6 months during her longest period without admissions (age 31–38). Susan’s longest therapeutic relationship was associated with a 4-year period without admissions (age 26–30). However, Jane was admitted six times during her longest therapeutic relationship (age 20–31). Admissions for both twins have also been precipitated by job changes, which likely involve changes in relationships with co-workers and may be associated with vulnerability due to more independent functioning.
Both twins characterize their longest relationships as being with “supportive” partners, and both have struggled when they have experienced emotional overinvolvement by others. This is consistent with the finding that high expressed emotion in relatives (characterized mainly by critical comments, emotional overinvolvement, and hostility) is associated with a high relapse rate in patients with schizophrenia (15). The twins say that many of their relationships have ended at the choice of their partners (e.g., one ended because a partner needed more time for his son). Psychological testing suggests differences between the twins that may affect their relationships. Jane seems particularly sensitive to affective arousal and is susceptible to becoming disorganized, whereas Susan seems to understand social schemas better but is more “thin skinned.” In light of this, gradual development of relationships for both twins seems very important.
Role of Medication
Medication has also played an important role in preventing readmission for these twins, although compliance has been problematic. Records for both twins indicate that stable relationships are associated with medication compliance, whereas unstable relationships are associated with medication noncompliance and subsequent admission.
Medication response has been remarkably similar in these cases. Both twins responded to lithium and a typical antipsychotic. Both developed tardive dyskinesia. Both are now being treated with the same dose of clozapine, although they are being treated independently. It is of interest that monozygotic twins with schizophrenia have been reported to respond well to the same dose of clozapine (16). Given her current presentation, Jane may benefit from a higher dose of clozapine. Unlike her sister, Jane is no longer taking lithium and is not being treated with an antidepressant. History indicates that Jane has had more frequent suicidal ideation than her sister. She may benefit from the addition of an antidepressant in the future. Lithium treatment has been associated with decreased suicidality, and clozapine may have a similar effect (17, 18). These medications may have contributed to the rarity of Susan’s suicidal ideation, although they do not seem to have yielded the same benefit for Jane.
Other Influences on the Course of Illness
Some other factors may also be important to the twins’ courses of illness. Jane’s history, unlike Susan’s, is significant for a suicide attempt, which predicts a high rehospitalization rate in patients with schizoaffective disorder (19) and poor global mental health in patients with borderline personality disorder (20). Other differences between the twins, specifically Susan’s history of low birth weight (less than 2500 g), head injury with loss of consciousness, and greater use of LSD, would more likely lead to a poorer course for Susan compared with her twin (21–23), which is not shown by her history. Susan’s recent course is more consistent with improved functioning during the second and third decades after index admission in patients with borderline personality disorder, reported by McGlashan (24), but borderline personality disorder may be less influential in determining the overall course of illness than the axis I disorder (25). The intervals between the twins’ admissions do not become shorter over time, as would be suggested by a process of kindling or behavioral sensitization (26, 27). This may be due to the impact of psychotropic medications, but a role for relationships in interrupting this process (perhaps by promoting compliance or mediating stress) cannot be ruled out.
Conclusions
The cases of twin sisters presented here cannot definitively point to any particular hypothesis about the role of genes and environment in psychosis. Nonetheless, they suggest that significant relationships, as well as medications, have a strong impact on the course of illness. Living in a partnership has previously been found to predict better outcomes in patients with schizophrenia (28), and this seems likely also true for patients with other forms of psychotic disorder. More research is needed to clarify the most essential aspects of relationships in promoting higher functioning concerning identical twins concordant for psychosis with personality disorder.
 |
Presented at a clinical case conference at the Massachusetts Mental Health Center, Department of Psychiatry, Harvard Medical School, on March 9, 1998. Received July 13, 1999; revision received March 15, 2000; accepted March 28, 2000. From the Massachusetts Mental Health Center, Department of Psychiatry, Harvard Medical School. Address reprint requests to Dr. Tsuang, Massachusetts Mental Health Center, Department of Psychiatry, Harvard Medical School, 74 Fenwood Rd., Boston, MA 02115-6113; mtsuang @warren.med.harvard.edu (e-mail).Supported in part by a Dupont-Warren Fellowship from the Department of Psychiatry, Harvard Medical School, and a Janssen Research Fellowship to Dr. Kelleher, and by NIMH grants MH-41879, MH-46318, and MH-43518 and a National Alliance for Research on Schizophrenia and Depression distinguished investigator award to Dr. Tsuang.The authors thank Anthony Kalinowski, Ph.D., and Richard Frishman, M.D., for their help.
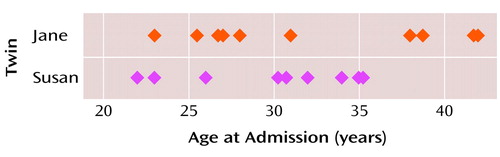
Figure 1. Ages at Hospital Admissions of Female Twins With Psychotic Illness
1. Segal NL: Entwined Lives: Twins and What They Tell Us About Human Behavior. New York, Dutton, 1999, pp 1–20Google Scholar
2. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GDV, Clark SL: Williams Obstetrics, 20th ed. Stamford, Conn, Appleton and Lange, 1997, pp 861–894Google Scholar
3. Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G: Wisconsin Card Sorting Test Manual. Odessa, Fla, Psychological Assessment Resources, 1993Google Scholar
4. Bellak L, Abrams DM: The Thematic Apperception Test, the Children’s Apperception Test, and the Senior Apperception Technique in Clinical Use, 6th ed. Boston, Allyn & Bacon, 1997Google Scholar
5. Tsuang MT: Schizophrenia: genes and environment. Biol Psychiatry 2000; 47:210–220Crossref, Medline, Google Scholar
6. Gottesman II, Shields J: Schizophrenia and Genetics: A Twin Study Vantage Point. New York, Academic Press, 1972Google Scholar
7. Gottesman II, Shields J: Schizophrenia: The Epigenetic Puzzle. Cambridge, UK, Cambridge University Press, 1982, pp 101–128Google Scholar
8. Kringlen E: Status of twin research in functional psychoses. Psychopathology 1986; 19:85–92Crossref, Medline, Google Scholar
9. Onstad S, Skre I, Torgerson S, Kringlen E: Birthweight and obstetric complications in schizophrenic twins. Acta Psychiatr Scand 1992; 85:70–73Crossref, Medline, Google Scholar
10. Kringlen E: Heredity and Environment in Functional Psychosis, vols 1–2. London, Heinemann, 1968Google Scholar
11. Abe K: The morbidity rate and environmental influence in monozygotic co-twins of schizophrenics. Br J Psychiatry 1969; 115:519–531Crossref, Medline, Google Scholar
12. Mirsky AF, Quinn OW: The Genain quadruplets. Schizophr Bull 1988; 14:595–612Crossref, Medline, Google Scholar
13. Burlingham D: Twins: observations of environmental influences on their development. Psychoanal Study Child 1946; 2:61–73Crossref, Medline, Google Scholar
14. Davidson S: Mother, other and self-love and rivalry for twins in their first year of life. Int Rev Psychoanal 1992; 19:359–374Google Scholar
15. Bebbington PE, Bowen J, Hirsch SR, Kuipers EA: Schizophrenia and psychosocial stresses, in Schizophrenia. Edited by Hirsch SR, Weinberger DR. Oxford, UK, Blackwell Science, 1995, pp 587–604Google Scholar
16. Vojvoda D, Grimmell K, Sernyak M, Mazure CM: Monozygotic twins concordant for response to clozapine (letter). Lancet 1996; 347:61Crossref, Medline, Google Scholar
17. Tondo L, Jamison KR, Baldessarini RJ: Effect of lithium maintenance on suicidal behavior in major mood disorders. Ann NY Acad Sci 1997; 836:339–351Crossref, Medline, Google Scholar
18. Meltzer HY: Suicide and schizophrenia: clozapine and the InterSePT study: International Clozaril/Leponex Suicide Prevention Trial. J Clin Psychiatry 1999; 60(suppl 12):47–50Google Scholar
19. Doering S, Muller E, Kopcke W, Pietzcker A, Gaebel W, Linden M, Muller P, Muller-Spahn F, Tegeler J, Schussler G: Predictors of relapse and rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Bull 1998; 24:87–98Crossref, Medline, Google Scholar
20. Mehlum L, Friis S, Vaglum P, Karterud S: The longitudinal pattern of suicidal behaviour in borderline personality disorder: a prospective follow-up study. Acta Psychiatr Scand 1994; 90:124–130Crossref, Medline, Google Scholar
21. Lane EA, Albee GW: Comparative birthweight of schizophrenics and their siblings. J Psychol 1966; 64:234–277Crossref, Google Scholar
22. Wilcox JA, Nasrallah HA: Childhood head trauma and psychosis. Psychiatry Res 1987; 21:303–306Crossref, Medline, Google Scholar
23. Abraham HD: Visual phenomenology of the LSD flashback. Arch Gen Psychiatry 1983; 40:884–889Crossref, Medline, Google Scholar
24. McGlashan TH: The Chestnut Lodge Follow-Up Study, III: long-term outcome of borderline personalities. Arch Gen Psychiatry 1986; 43:20–30Crossref, Medline, Google Scholar
25. McGlashan TH: The borderline syndrome, II: is borderline a variant of schizophrenia or affective disorder? Arch Gen Psychiatry 1983; 40:1319–1323Google Scholar
26. Post RM, Rubinow DR, Ballenger JC: Conditioning, sensitization, and kindling: implications for the course of affective illness, in The Neurobiology of Mood Disorders. Edited by Post RM, Ballenger JC. Baltimore, Williams & Wilkins, 1984, pp 432–466Google Scholar
27. Lieberman JA, Sheitman BB, Kinon BJ: Neurochemical sensitization in the pathophysiology of schizophrenia: deficits and dysfunction in neuronal regulation and plasticity. Neuropsychopharmacology 1997; 17:205–230Crossref, Medline, Google Scholar
28. Biehl H, Maurer K, Schubart C, Krumm B, Jung E: Prediction of outcome and utilization of medical services in a prospective study of first onset schizophrenics. Eur Arch Psychiatry Neurol Sci 1986; 236:139–147Crossref, Medline, Google Scholar



